 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. HIV Transmission Among Black College Student and Non-Student Men Who Have Sex With Men --- North Carolina, 2003In the United States, young black men who have sex with men (MSM) and reside in urban settings have high rates of infection with human immunodeficiency virus (HIV), with incidence and prevalence as high as 14% and 32%, respectively (1--4). Few epidemiologic and behavioral studies have been conducted in this population, and even fewer data are available for black MSM from non-urban areas of the southern United States. In November 2002, the North Carolina Department of Health (NCDOH) identified two cases of acute HIV infection among non-Hispanic black male college students. A retrospective review of all men aged 18--30 years with HIV diagnosed during January 2000--May 2003 indicated an increase in HIV case reports in male college students, from two cases in 2000 to 56 during January 2001--May 2003 (5). Of these 56, a total of 49 (88%) were black, and nearly all were MSM, including some men who had sex with both men and women. In August 2003, NCDOH invited CDC to assist with an epidemiologic investigation of young HIV-positive black MSM in North Carolina. This report summarizes the results of that investigation, which indicated that black MSM college students and non-students in North Carolina had high rates of HIV risk behaviors, underscoring the need for enhanced HIV-prevention programs in these populations. NCDOH surveillance data from 1998--2002 for newly reported HIV infections and North Carolina census data were reviewed (6); age- and race-specific HIV rates were calculated. A case-control study was conducted to identify behavioral risk factors for HIV infection in young black MSM. Cases were defined as those occurring in HIV-positive college students who had HIV diagnosed during 2001--2003, were black MSM aged 18--30 years, and were North Carolina residents. Two groups of HIV-negative controls were enrolled in the study (i.e., college students and non-students), all of whom also were black MSM aged 18--30 years who lived in North Carolina. Face-to-face interviews were conducted to obtain epidemiologic and behavioral information. Sexual behaviors were reported for the 12-month period preceding either the date of diagnosis for HIV-positive college students or the date of interview for HIV-negative college students and non-students. To complement quantitative information collected by questionnaire, all participants were asked to share insights about why high-risk sexual behavior was occurring among young black MSM. In addition, three discussion groups were convened with approximately 60 black male and female students from 11 colleges in North Carolina to discern perceived barriers to sexual risk reduction and to elicit suggestions for prevention programs targeting college students. During 1998--2002, rates of newly reported HIV infection in North Carolina were higher in black men in all age groups compared with white men overall (Figure). Among black men aged 18--24 years, a statistically significant increase was observed during this period, from 65 per 100,000 population in 1998 to 92 in 2002 (p<0.01). Of the 49 HIV-positive black male college students who had been identified previously by the NCDOH HIV surveillance system, 17 (35%) were recruited for the study; 24 could no longer be located or did not respond to inquiries, seven refused participation, and one was deceased. One case was identified in an HIV-positive college student during control recruitment activities. Overall, 19 HIV-negative college students and 15 HIV-negative non-students were recruited during HIV pre- or post-test counseling activities at local health departments (n = five), gay nightclubs (n = 26), and the North Carolina Pride Festival (n = three). In general, characteristics of the HIV-positive and HIV-negative college student groups were similar to one another but different from the HIV-negative non-student group (Table). Other than lifetime history of gonorrhea, no statistically significant differences were seen among the three groups. College students were younger than non-students, and the mean number of lifetime sex partners was lower for college students than non-students. The mean number of partners and the frequency of unprotected receptive anal intercourse with casual and steady partners were similar for the three groups. The majority of both steady and casual sexual partners for all three groups were black and aged 18--30 years. Approximately 20% of study participants had a female sex partner during the preceding 12 months. Nearly one third of both HIV-positive and HIV-negative college students met sex partners on college campuses, but the majority of both of these groups met their sex partners at gay nightclubs or over the Internet. Fewer college students than non-students identified as gay or disclosed their sexual identity to everyone or to most people. Nearly 70% of study participants previously had tested for HIV, and 70% believed they were unlikely to have been infected with HIV at the time of their most recent HIV test. Two HIV-positive students, six HIV-negative students, and four non-students reported having had recent sex partners in multiple states outside of North Carolina, including Delaware, Florida, Georgia, New York, South Carolina, Tennessee, Texas, Virginia, and the District of Columbia. Both MSM study participants and college student discussion group participants provided similar explanations for why MSM specifically, and young black people in general, continue to engage in high-risk sexual behavior. The most common reasons were 1) lack of sustained prevention messages targeting young blacks, 2) feeling personally disconnected from the reality that they might contract HIV, and 3) believing that physical characteristics and appearance can inform one about their partner's HIV status. Reported by: P Leone, L Hightow, MD, Univ of North Carolina, Chapel Hill; E Foust, MPH, J Owen-O'Dowd, S Phillip, MHA, P Gray, MPH, B Jones, MPH, North Carolina Dept of Health. L Fitzpatrick, MD, G Millett, MPH, K Jones, MSW, R Stall, PhD, S Holmberg, MD, A Greenberg, MD, Div of HIV/AIDS Prevention, National Center for HIV, STD, and TB Prevention; L Ahdieh-Grant, PhD, C Eure, MD, EIS officers, CDC. Editorial Note:The findings in this report highlight the need for enhanced HIV-prevention programs among young black MSM and are consistent with previous studies documenting elevated HIV risk behaviors and infection in this population (3,4). The high-risk sexual behaviors noted among the limited number of black MSM college students and non-students in this investigation could be related to the increase in HIV rates observed for black men aged 18--24 years in North Carolina surveillance data and might provide insights into the broader HIV transmission patterns among young, black MSM in general. Although one third of black MSM college students reported meeting partners on campus, the majority reported meeting partners either at nightclubs or over the Internet, suggesting that prevention activities need to be targeted both on and off campus. Moreover, because many young black MSM might not regularly visit traditional testing sites such as health departments for sexually transmitted disease (STD)- and HIV-related health concerns, alternative venues such as nightclubs and the Internet should be considered as nontraditional testing and/or prevention sites for this population. Despite the high rates of high-risk behaviors, STDs, and previous HIV testing in this population, the majority of study participants did not perceive themselves at risk for HIV infection at the time of their most recent HIV tests. This finding suggests that current HIV-prevention messages are not effectively reaching young black MSM and that education about HIV risk needs to be more effectively communicated at the time of HIV testing. Moreover, because risk perception might be diminished by receipt of a negative HIV test, reports of high-risk sexual behavior must be addressed with appropriate prevention messages at the time of HIV pre- and post-test counseling. In addition, the results of this study support the integration of HIV-prevention activities into routine STD evaluation and care. Because a substantial proportion of the college students either did not identify as gay or were not open about their sexual identity, prevention messages that focus on sexual risk reduction rather than gay identity should be developed for young black MSM. In addition, because nearly 20% of study participants also reported having recent female sex partners, HIV risk--reduction messages should be developed and communicated to young women as well. The information collected in the discussion groups with black college students highlights the value of soliciting community input before developing on- and off-campus HIV-prevention messages for this population. Because study participants reported having recent sex contacts in multiple states, the frequency of high-risk behaviors in this population might not be limited to North Carolina. Further surveillance activities are needed to define the extent of high-risk behaviors among young black MSM in other geographic areas so appropriate on- and off-campus HIV-prevention activities can be designed. The findings in this report are subject to at least four limitations. First, the sexual behaviors of enrolled participants might have been different from those persons not enrolled. Second, recall bias for high-risk behaviors might have occurred, especially for students with HIV diagnosed in 2001. Third, a selection bias might have been introduced because HIV-positive participants were identified through case reports, whereas HIV-negative participants were recruited primarily at nightclubs. Finally, the small sample size limits the ability to make certain inferences regarding differences in sexual behaviors. This investigation demonstrates that expansion of multiple HIV-prevention activities for young black MSM is needed. Because this is the first investigation conducted in young black MSM outside of large urban settings, further studies should explore whether similar phenomena are occurring in other states, particularly in the southern United States. In response to these findings, CDC and NCDOH are collaborating to adapt a scientifically based preventive intervention for the black MSM population in North Carolina (7). In addition, CDC recently announced the availability of funding to implement rapid-- HIV-testing demonstration projects in settings that include college campuses. State and local health departments as well as community-based organizations should consider engaging in similar HIV-prevention efforts and in the development of effective preventive interventions for young black MSM. References
Table 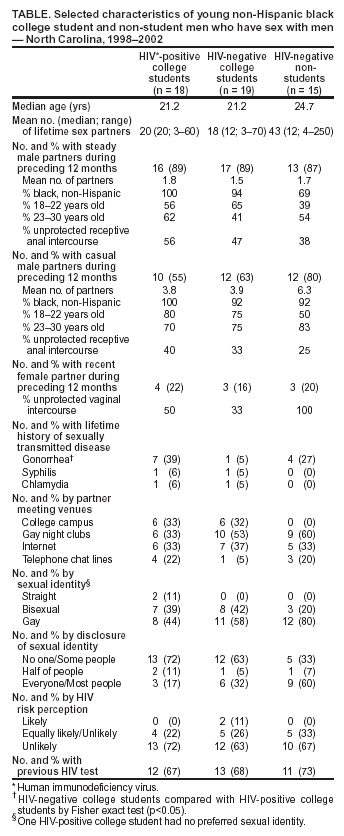 Return to top. Figure  Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 8/19/2004 |
|||||||||
This page last reviewed 8/19/2004
|