 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Urban Planning and Public Health at CDCChris S. Kochtitzky, MSP,1 H. Frumkin, MD,
DrPH,2 R. Rodriguez, MA,2 A. L. Dannenberg,
MD,2 J. Rayman, MPH,2 K. Rose,
MPA,2 R. Gillig, MCP,2 T. Kanter,
MURP3
Corresponding author: Chris S. Kochtitzky, MSP, Office of the Director, Coordinating Center for Environmental Health and Injury Prevention, 1600 Clifton Road, N.E., MS E-28, Atlanta, GA 30333. Telephone: 404-498-0668; Fax: 404-498-0083; E-mail: csk3@cdc.gov. IntroductionUrban planning, also called city and regional planning, is a multidisciplinary field in which professionals work to improve the welfare of persons and communities by creating more convenient, equitable, healthful, efficient, and attractive places now and for the future. The centerpiece of urban planning activities is a "master plan," which can take many forms, including comprehensive plans, neighborhood plans, community action plans, regulatory and incentive strategies, economic development plans, and disaster preparedness plans (1). Traditionally, these plans include assessing and planning for community needs in some or all of the following areas: transportation, housing, commercial/office buildings, natural resource utilization, environmental protection, and health-care infrastructure. Urban planning and public health share common missions and perspectives. Both aim to improve human well-being, emphasize needs assessment and service delivery, manage complex social systems, focus at the population level, and rely on community-based participatory methods. Both fields focus on the needs of vulnerable populations. Throughout their development, both fields have broadened their perspectives. Initially, public health most often used a biomedical model (examining normal/abnormal functioning of the human organism), and urban planning often relied on a geographic model (analysis of human needs or interactions in a spatial context). However, both fields have expanded their tools and perspectives, in part because of the influence of the other. Urban planning and public health have been intertwined for most of their histories. In 1854, British physician John Snow used geographic mapping of an outbreak of cholera in London to identify a public water pump as the outbreak's source. Geographic analysis is a key planning tool shared by urban planning and public health. In the mid-1800s, planners such as Frederick Law Olmsted bridged the gap between the fields by advancing the concept that community design contributes to physical and mental health; serving as President Lincoln's U.S. Sanitary Commission Secretary (2); and designing hundreds of places, including New York's Central Park. By 1872, the disciplines were so aligned that two of the seven founders of the American Public Health Association were urban designers (an architect and a housing specialist) (3). In 1926, the U.S. Supreme Court, in validating zoning and land-use law as a legal government authority in Village of Euclid v. Ambler Realty, cited the protection of public health as part of its justification (4,5). Other connections have included 1) pioneering urbanist Jane Jacobs, who during the 1960s, called for community design that offered safe and convenient options for walking, biking, and impromptu social interaction; and 2) the Healthy Cities movement, which began in Europe and the United States during the 1980s and now includes projects in approximately 1,000 cities that in various ways highlight the role of health as much more than the presence of medical care (6). Contributions of Urban Planning to Public HealthDuring the 19th and early 20th centuries, the synergies between urban planning and public health were evident in at least three areas: creation of green space to promote physical activity, social integration, and better mental health; prevention of infectious diseases through community infrastructure, such as drinking water and sewage systems; and protection of persons from hazardous industrial exposures and injury risks through land-use and zoning ordinances. During the middle of the 20th century, the disciplines drifted apart, to a certain extent because of their success in limiting health and safety risks caused by inappropriate mixing of land uses. The disciplines recently have begun to reintegrate. During the last 20 years, shared concerns have included transportation planning to improve air quality, encourage physical activity, prevent injuries, and promote wellness. In addition, some original crossover ideas, such as the potential for parks and recreational facilities to contribute to physical activity and mental health, have reemerged. Relatively recently, urban planning has focused on the effects of community design on energy use and greenhouse gas emissions to affect the growing public health concern of climate change. Finally, emergency preparedness (e.g., community infrastructure assurance, evacuation planning) and access to health care (e.g., assurance of accessibility and adequacy of facilities) are topics important to both disciplines. Recent contributions to the public health knowledge-base by urban planners and other community designers, such as architects and engineers, are important. A recent tabulation of the 50 most-read/most-cited articles within the American Journal of Public Health (AJPH) (as of October 1, 2006) included topics of interest to both urban planning and public health professionals, such as social capital, neighborhood-level effects on health, housing and health, and clustering of fast-food establishments around schools (7). Examples of cross-discipline collaborations (Table 1) from publications such as JAMA and AJPH address such diverse CDC program areas as aging studies, air pollution and respiratory diseases, disability and health, unintentional injury, and nutrition and physical activity. As individual collaborations have increased, calls for broad profession-level integrations also have increased (Table 2). Thus far, CDC has employed only a few urban planners, either temporarily or permanently. Urban planners, for instance, have worked within the ATSDR Policy Office, Division of Health Assessment and Consultation, and Office of Tribal Affairs; within the National Center for Environmental Health Policy Office and Division of Emergency and Environmental Health Services; within the National Center on Birth Defects and Developmental Disabilities Division of Human Development and Disability; and within the National Center for Chronic Disease Prevention and Health Promotion Division of Nutrition and Physical Activity. Although these urban planners have conducted some research, their primary role has been to bridge the broader urban planning, academic, and practitioner worlds. Specific Findings, Activities, and ContributionsThe interdependence of urban planning and public health in both research and intervention activities is evident in many areas. For example, to increase physical activity, persons need safe and accessible areas; development of these areas can be aided by determining the environmental barriers and facilitators that affect activity levels; designing, constructing, and maintaining community environments to help ensure safety and accessibility; and developing programs to encourage people to use improved community environments to increase their activity levels. Without the contributions of both disciplines, the odds of substantial increases in community physical activity decrease considerably. Pedestrian and bicycle safety programs also illustrate the interdependence of public health and urban planning. Transportation planners are charged with creating streets and intersections on which all modes of transportation can safely coexist. However, considerable morbidity and mortality occur annually because of injuries related to interactions between motorists, bicyclists, and pedestrians, indicating that many communities have failed to truly balance choices of transportation modes. Examples of recent successful cross-discipline activities include chronic disease prevention, injury prevention, health promotion for older adults and persons with disabilities, and air- and water-quality assurance. Reviews of research studies conducted by cross-disciplinary teams on behalf of the Guide to Community Preventive Services have documented that street-scale urban design and land-use policies affect levels of physical activity and result in recommendations for wider implementation of such policies (8). Similarly, research has documented the potential for design choices to reduce both unintentional (9,10) and intentional (11,12) injuries. Research has described some of the impacts of physical environments on the health and quality of life of persons with disabilities (13), residents of low-income housing projects (14), and older adults (15). In environmental health, data analysis of waterborne-disease outbreaks and extreme weather events indicates potential interaction between land-use patterns and risk for waterborne diseases (16). In an equally important area of environmental health---air quality and respiratory health---CDC staff used the unique "natural experiment" of the Atlanta Olympics to document a 42% decrease in acute asthma events among children that were attributable to reductions in automobile traffic and associated air pollution (17). Other impacts of the interdependence of urban planning and public health also have been demonstrated (Table 3). Urban planning in particular and the array of community design professions in general historically have played major roles in public health, and public health disciplines have played major roles in urban planning. In recent years, as reintegration between the two professions has accelerated, academia has responded by offering cross-cutting courses and, in at least five schools, joint graduate degrees in urban planning and public health. At the federal level, CDC leadership selected seven "place-related" goals reflecting this reintegration (18), many of which are impacted by urban planning. CDC scientifically and programatically addresses all factors associated with the interaction between people and their natural and human-made environments and promotes design and construction of places that improve both physical and social environments (http://www.cdc.gov/healthyplaces). Providing safe and healthy places in which to live, work, and play is more likely to succeed if urban planning and public health work together. Future integration of and collaborations between the disciplines can serve as a cornerstone for the immediate and long-term success of the Healthy Places goals (19). A long-term blending of the responsibilities, tools, and eventually perspectives of public health and urban planning can result in many positive outcomes, including the following:
This renewed integration is essential in restoring and enhancing the health and vitality of the nation's places and people. References
Table 1 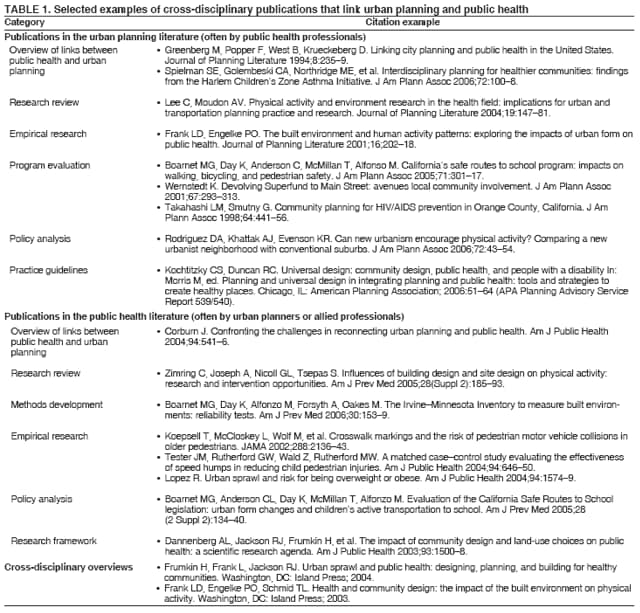 Return to top. Table 2 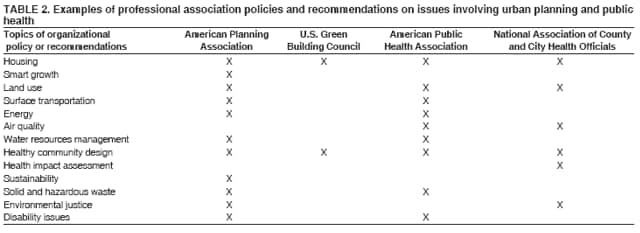 Return to top. Table 3 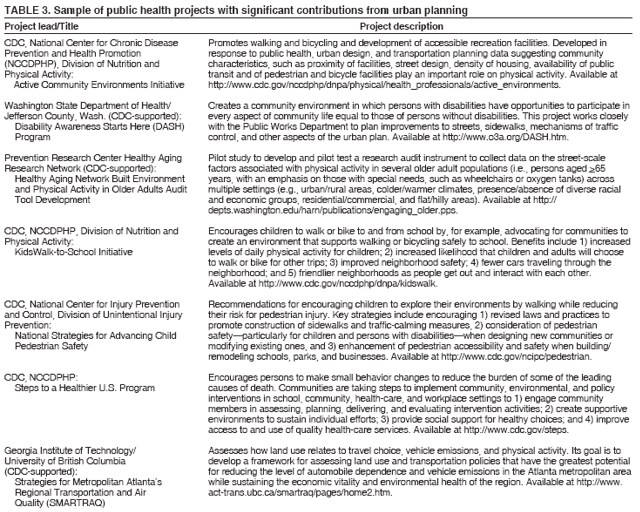 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 12/18/2006 |
|||||||||
|