

|

|

Volume
7: No. 3, May 2010
ORIGINAL RESEARCH
Prevalence, Awareness, Treatment, and Control of High LDL Cholesterol in New York City, 2004
Ushma D. Upadhyay, PhD, MPH; Elizabeth Needham Waddell, PhD, MA; Stephanie Young, MPH; Bonnie D. Kerker, PhD, MPH; Magdalena Berger, MPH; Thomas Matte, MD, MPH; Sonia Y. Angell, MD, MPH
Suggested citation for this article: Upadhyay UD, Waddell EN, Young S, Kerker BD, Berger M, Matte T, et al. Prevalence, awareness, treatment, and control of high LDL
cholesterol in New York City, 2004. Prev Chronic Dis 2010;7(3):A61.
http://www.cdc.gov/pcd/issues/2010/
may/09_0196.htm. Accessed [date].
PEER REVIEWED
Abstract
Introduction
Low-density lipoprotein (LDL) cholesterol is a major contributor to coronary heart disease and the primary target of cholesterol-lowering therapy. Substantial disparities in cholesterol control exist nationally, but it is unclear how these patterns vary locally.
Methods
We estimated the prevalence, awareness, treatment, and control of high LDL cholesterol using data from a unique local survey of New York City’s diverse population. The New York City Health and Nutrition Examination Survey 2004 was administered to a probability sample of New York City adults. The National Health and Nutrition Examination Survey 2003-2004 was used for comparison. High LDL cholesterol and coronary heart disease risk were defined using National Cholesterol Education
Program Adult Treatment Panel III (ATP III) guidelines.
Results
Mean LDL cholesterol levels in New York City and nationally were similar. In New York City, 28% of adults had high LDL cholesterol, 71% of whom were aware of their condition. Most aware adults reported modifying their diet or activity level (88%), 64% took medication, and 44% had their condition under control.
More aware adults in the low ATP III risk group than those in higher risk groups had
controlled LDL cholesterol (71% vs 33%-42%); more whites than blacks and
Hispanics had controlled LDL cholesterol (53% vs 31% and 32%, respectively).
Conclusions
High prevalence of high LDL cholesterol and inadequate treatment and control contribute to preventable
illness and death, especially among those at highest risk. Population approaches — such as making the food environment more heart-healthy — and aggressive clinical management of cholesterol levels are needed.
Back to top
Introduction
Coronary heart disease (CHD) is the leading cause of death in the United States, accounting for 27% of all deaths in 2005 (1). An established body of evidence points to reducing low-density lipoprotein (LDL) cholesterol as one of the most effective ways to prevent and treat CHD, regardless of a person’s risk (2-4). On average, every 1% reduction in LDL cholesterol is matched by a 1% reduction in the likelihood of a major cardiac event (5). Thus, small reductions in
population LDL cholesterol could prevent many CHD-related deaths.
Despite advances in lowering total blood cholesterol, particularly throughout the 1980s (6,7), and the recent broad-scale use of medications targeting LDL cholesterol, control of lipid levels remains poor in the United States. Prevalence of high total cholesterol and high LDL cholesterol remained virtually unchanged between 1988-1994 and 1999-2004 (8,9), and only one-fourth of US adults with elevated LDL cholesterol have their condition appropriately controlled (8). Blacks and Mexican
Americans are less likely than whites to take drugs from the statin class, and they have poorer control (8,10).
National estimates of high LDL cholesterol are not available for other Hispanics or for Asians.
Local monitoring of the prevalence, treatment, and control of CHD risk factors is
needed for planning and evaluating interventions to prevent disease. Previous studies suggest that New York City is similar to or better than the rest of the country in terms of prevalence and management of some CHD risk factors (hypertension and obesity) (11,12) but worse for others (diabetes) (12,13). However, no study has examined LDL cholesterol levels
by using a representative sample in New York City or in
any exclusively urban setting. In this study, we examine prevalence, awareness, treatment, and control of high LDL cholesterol in New York City adults
by using the first community Health and Nutrition Examination Survey (NYC HANES). To define high LDL levels, we used the National Cholesterol Education Program Adult Treatment Panel III (ATP III) guidelines, which provide thresholds for diagnosing and targets for lowering high LDL cholesterol
on the basis of individual CHD risk (5,14). Findings on
variation in LDL cholesterol levels in this population may be useful for researchers and policy makers in other urban environments.
Back to top
Methods
NYC HANES is a population-based, cross-sectional, examination survey of noninstitutionalized New York City adult residents aged 20 years or older. A 3-stage cluster sampling design was used to recruit participants from June through December 2004. Detailed study methods are published elsewhere (15). The survey consisted of personal interviews, physical examinations, and laboratory testing. All survey instruments, protocols, and measurements were standardized to National Health and Nutrition
Examination Survey (NHANES) specifications. Lipid profiles were analyzed at the Lipoprotein Analytical Laboratory at Johns Hopkins University Hospital. Most laboratories that perform testing for NHANES were used for NYC HANES (16).
The NYC HANES protocol was approved by the New York City Department of Health and Mental Hygiene and the New York State Department of Health institutional review boards. Study participants provided written, informed consent.
A total of 3,047 eligible participants were identified (84% household contact rate); 1,999 completed the face-to-face interview and at least 1 examination measurement (66% participant response rate), yielding an overall response rate of 55%. Of the 1,999 participants, valid
high-density lipoprotein (HDL) and total cholesterol measurements were obtained for 1,783 participants. A random sample of participants (80%) was assigned to fast for at least 8 hours before giving blood, and of these,
valid measurements were available for 1,150 participants. An additional 136 participants not assigned to fast but who did voluntarily were
similar to those assigned to fast for all demographic characteristics except age and were included in the sample. Valid LDL cholesterol data were available for 1,286 participants.
ATP III risk groups
Participants were categorized into 1 of 4 CHD risk groups — high, moderately high, moderate, or low — following ATP III guidelines (14). These consider 1) presence of CHD or CHD risk equivalents, 2) presence of CHD risk factors, and 3) 10-year CHD risk using Framingham risk scoring
(Table 1).
CHD and CHD risk equivalents were self-reported history of congestive heart failure, coronary heart disease, angina pectoris, myocardial infarction, stroke, or diabetes (determined by self-report or having a fasting glucose value ≥126 mg/dL). CHD risk factors were self-reported cigarette smoking, hypertension (measured blood pressure ≥140/90 mm Hg or self-reported current use of antihypertensive medications) (11), measured HDL cholesterol <40 mg/dL, family history of
premature CHD (reported knowledge of heart attack or angina before age 50 among biological grandparents, parents, or siblings), and older age (men ≥45 y, women ≥55 y). Measured HDL cholesterol ≥60 mg/dL was considered protective and offset the presence of 1 risk factor. The Framingham risk score estimates risk of developing angina pectoris, myocardial infarction, or CHD death within 10 years (17) and was calculated for each participant
by using algorithms provided in ATP III
guidelines.
Cholesterol levels
Serum total and HDL cholesterol concentration were measured directly (12). LDL cholesterol was calculated from the fasting subsample’s sera by using the Friedewald equation (18):
LDL cholesterol [mg/dL] = total cholesterol [mg/dL] – HDL [mg/dL] – triglycerides [mg/dL]/5.
High LDL cholesterol was defined as currently taking cholesterol-lowering medications or having LDL cholesterol levels at or greater than the ATP III risk-specific thresholds recommended for initiation of drug therapy in each risk group (5) (Table 1).
Awareness, treatment, and control of high LDL cholesterol
Participants were asked if they had ever had their cholesterol checked, and if so, whether a doctor or other health professional had told them their cholesterol level was high. Those who answered yes were considered aware of their diagnosis of high cholesterol and then asked the following questions about treatment: “To lower your blood cholesterol, have you ever been told by a doctor or other health professional to: a) eat fewer high-fat or high-cholesterol foods, b) control your weight or
lose weight, c) increase your physical activity or exercise, or d) take prescribed medicine?” Respondents who answered yes to any of the questions were asked whether they were following this advice. Those who reported following at least 1 of these recommendations were classified as having adopted a healthier behavior to lower their cholesterol. Those who said they were taking prescribed cholesterol-lowering medications were classified as treated with medication. For all participants with high
LDL cholesterol, control was defined as measured LDL cholesterol lower than the ATP III goal for their specific risk group (Table 1).
Demographics and health characteristics
NYC HANES assessed basic demographic characteristics (age, sex, race/ethnicity, place of birth, income, and education), health insurance status, cigarette smoking, and physical activity.
We used the NHANES definition of “US-born,” which includes the 50 states and Washington, DC; participants born in Puerto Rico and other US territories were categorized as foreign-born. “Vigorous physical activity” was based on Healthy People 2010 guidelines and defined as activity that causes
heavy sweating or increases in breathing or heart rate for at least 20 minutes, at least 3 days per week. Body mass index (BMI) was calculated from weight and height measurements.
Data analyses
We compared age-standardized New York City with national mean total and LDL cholesterol using the NHANES 2003-2004 fasting sample aged 20 years or older (16). We also compared the distribution of adults across various categories of total and LDL cholesterol levels.
We assigned each participant to a CHD risk group based on ATP III criteria and then estimated age-standardized prevalence of high LDL cholesterol among New York City adults overall and by ATP III risk group. To identify New York City populations at increased risk for high LDL cholesterol, we estimated age-standardized prevalence of high LDL cholesterol by demographic and health characteristics, including BMI, physical activity, smoking status, and other indicators of CHD risk.
We estimated awareness among adults with high LDL cholesterol, treatment and control among adults aware of their condition, and control among those treated with cholesterol-lowering medication. Awareness, treatment, and control of high LDL cholesterol were also examined by sociodemographic characteristics, insurance status, and ATP III risk group.
All statistical analyses were conducted by using SUDAAN version 10.0 (RTI
International, Research Triangle Park, North Carolina) to account for complex survey design. Prevalence estimates were age-adjusted to the 2000 US standard population (19). Significance of univariate differences in prevalence, awareness, treatment, and control of high LDL was determined by using t tests derived from the general linear contrast procedure.
We used χ2 tests to identify significant associations
between the outcomes and covariates with 3 or more levels. Relative standard errors and 95% confidence intervals (CIs) were calculated for percentages. Analytic weights were poststratified to represent the New York City adult population for NYC HANES data and the US adult population for NHANES data, then further adjusted for age, sex, and race/ethnicity to address component and item nonresponse (20). Significance was set at P < .05.
Back to top
Results
Mean total and LDL cholesterol
Mean total cholesterol was significantly lower in New York City (197.7 mg/dL) than in the United States overall (203.0 mg/dL)
(Table 2). No difference was seen in mean LDL cholesterol overall, but New York City foreign-born adults had higher mean LDL cholesterol than US foreign-born adults (122.5 vs 117.8).
Prevalence of ATP-defined high LDL cholesterol
Most New York City adults (64.8%; 95% CI, 61.4%-68.1%) were in the low ATP III risk group, while 17.9% (95% CI, 15.2%-20.9%) were in the high-risk group (Figure). According to ATP III-defined thresholds, total prevalence of high LDL cholesterol was 27.8% (Figure).
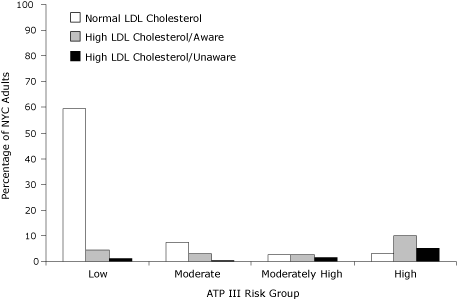
Figure. Age-standardized prevalence of high LDL cholesterol among
New York City adults by ATP III risk category (5,14), New York City Health and Nutrition Examination Survey 2004. High LDL cholesterol defined as currently taking cholesterol-lowering medications or having LDL cholesterol levels at or greater than the ATP III risk-specific thresholds recommended for initiation of drug therapy: ≥100 mg/dL for the high-risk group, ≥130 mg/dL for the moderately high-risk group,
≥160 mg/dL for the moderate-risk group, and ≥190 mg/dL for the
low-risk group. Abbreviations: NYC, New York City; ATP III, National Cholesterol
Education Program Adult Treatment Panel III; LDL, low-density lipoprotein.
[A tabular version of this figure is also available.]
Significant differences in the prevalence of high LDL cholesterol were observed by ATP III risk group and across several demographic and health characteristics (Table 3). There was a strong, graded association between ATP III risk group and
the presence of high LDL cholesterol: 11.1% of those at low risk, 31.3% of those at moderate risk, 56.9% of those at moderately high risk, and 78.4% of those at high risk. Older age was associated with increased risk of high LDL cholesterol;
more adults
aged 60 years or older (58.6%) had high LDL cholesterol than did adults aged 40
to 59 years (31.4%) and aged 20 to 39 years (6.6%). LDL cholesterol levels were
higher among men than among women and among adults with high school education or less than among those with more education. A particularly low proportion of uninsured adults had high LDL cholesterol (15.4%).
More overweight (29.6%) and obese (38.9%) participants had high LDL cholesterol than
did those with normal or underweight BMI (17.6%), and more current smokers had high LDL cholesterol than nonsmokers (37.2% vs 24.8%).
More adults with hypertension (41.3%) or diabetes (79.1%) had high LDL cholesterol than
did those without these conditions (22.4% and 22.1%, respectively).
Awareness, treatment, and control of high LDL cholesterol
Among New York City adults with high LDL cholesterol, more than two-thirds (70.9%) were aware of their condition (Table 4). Rates of awareness varied significantly by age group, education, and health insurance status.
Fewer adults aged 20 to 39 years (48.4%) and aged 40 to 59 years (65.7%) were aware of their high LDL cholesterol than those aged 60 or older (80.4%).
Fewer adults with high school education or less (64.0%) were aware of their condition than those with
more education (80.8%). Three-fourths (73.8%) of insured adults with high LDL cholesterol were aware of their condition, compared with 46.2% of the uninsured (P = .005).
Among adults who were aware of their high LDL cholesterol, most (88.1%) reported changing their diet, trying to lose weight, or increasing physical activity to lower cholesterol.
A lower proportion of younger people than older people (68.0% vs 92.0%) and a
higher proportion of women than men (93.4% vs 83.8%) adopted healthier behaviors.
Fewer aware adults in the high-risk group were treated with medication than those in the low-risk group (62.0% vs 77.1%).
Aware adults aged 60
or older (72.8%) had higher rates of treatment with medication than those aged 40 to 59 years (57.1%) and 20 to 39 years (35.7%). Only 43.7% had their LDL cholesterol adequately controlled
(Table 5). We observed significant disparities in rates of control among those who were aware of their condition by risk group, age, and race/ethnicity. More than two-thirds (71.3%) of adults in the low-risk group had their LDL cholesterol controlled, compared with only one-third of adults in the high-risk
group. A smaller proportion of younger adults who were aware of their high cholesterol (22.4%)
had their LDL cholesterol controlled than did those aged 60 or older (51.3%). Rates of control among whites (53.2%) were higher than among blacks (31.2%) and Hispanics (31.8%).
Among those treated with cholesterol-lowering medication, two-thirds (68.3%; 95% CI, 56.9%-77.7%) had LDL cholesterol at recommended levels for their risk group.
Fewer adults treated with medication in the high-risk group had their condition under control than
did those in the low-risk group (53.8% vs 92.5%; P < .001), as were treated foreign-born adults compared with treated US-born adults (57.8% vs 78.0%, P = .04).
Back to top
Discussion
This study documents the large burden of high LDL cholesterol in New York City. We found that more than 1 in 4 New York City adults have high LDL cholesterol, placing them at elevated risk for CHD (2,3). This proportion is similar to national levels (8).
We also found that nearly one-third of New York City adults with high LDL cholesterol were unaware of their condition. Among those who were aware, less than two-thirds were taking cholesterol-lowering medications and less than half had their LDL cholesterol under control, suggesting that adults in New York City are not adequately treated. We found particularly low levels of treatment and control among those in the highest CHD risk groups, and low levels of control among black and Hispanic
populations. Intensive efforts are needed to reduce LDL cholesterol among these groups (4).
Lower awareness and treatment rates may be due in part to providers’ use of guidelines other than the 2004 ATP III. Providers who use the US Preventive Services Task Force (USPSTF) guidelines would not screen low-risk men before age 35 or women before age 45 (21). ATP III recommends screening all adults from age 20, every 5 years. Using USPSTF guidelines, 16% of those we defined as unaware of high LDL cholesterol would not have been routinely screened. Similarly, low rates of treatment
in the high-risk group may be due to limited provider adoption of the 2004 ATP III guidelines, which reduced the threshold for drug therapy in the high-risk group from ≥130 mg/dL to ≥100 mg/dL. However, using the former threshold of 130 mg/dL for the high-risk group results in a similarly low treatment rate of 69.0% among those who were aware of having high LDL cholesterol.
Our analysis of the distribution of mean LDL cholesterol found similar levels between New York City and the United States, but a higher mean LDL cholesterol among foreign-born adults in New York City than among foreign-born adults in the United States overall. Foreign-born adults make up more than one-third (36.7%) of New York City’s population (compared with 12.5% of the US population) (22). The higher mean in New York City may be due to differences in the racial/ethnic diversity in
the NYC
HANES foreign-born population (22% white, 18% black, 19% Asian, 39% Hispanic, and 2% “other”) compared with
the NHANES foreign-born population (27% white, 7% black, 28% Mexican American, 18% other Hispanic, and 21% “other/multiracial”).
This study builds on previous NHANES studies by measuring LDL cholesterol among Hispanics and Asians, which
could not be assessed in prior national surveillance data, and a closer examination of the foreign-born. New York City Hispanics had particularly low levels of awareness compared with whites, possibly because of less access to care. Lack of insurance was associated with lower awareness levels. Diagnosis of high cholesterol requires a blood test, and treatment requires ongoing
monitoring, costs of which can be barriers for people without insurance coverage. Also of concern is the disparity in control rates between foreign- and US-born adults who are treated with medication. These findings support the need to identify and respond to health disparities (23) to ensure increased access to health care for all groups.
The high prevalence of high LDL coupled with poor levels of control suggests that effective strategies to reduce cholesterol requires a multilevel approach that includes and goes beyond the clinic. Population approaches to prevent and reduce high LDL cholesterol offer opportunities to reduce risk across all risk groups (24).
Our findings are consistent with those of other studies that associated overweight or obesity and smoking with high LDL cholesterol (25,26) and underscore the need for policies that improve the food environment and reduce smoking. New York City has introduced such population-based initiatives. These include restricting the use of artificial trans fat in restaurants
(27), increasing the number of mobile vendors that sell vegetables, and setting nutrition standards for foods purchased by New York City
agencies. Such policies aim to normalize heart-healthy eating and represent a promising strategy to reduce cholesterol levels and CHD risk (24). Smoking prevalence is dramatically lower in New York City (28) after an increase in local and state cigarette taxes (making them among the most expensive in the country), hard-hitting antitobacco advertising, and wide distribution of free nicotine patches and gum (29). Federal action to extend similar and other effective policies across the country are
needed for widespread reductions in LDL cholesterol.
In addition to environment change approaches, improved clinical approaches to diagnosis and management of high LDL cholesterol are needed. Studies have demonstrated that delayed initiation of treatment for high LDL
is common, despite evidence that early initiation and longer duration of therapy
mitigates the atherosclerotic process (30). Once initiated, medication therapy
is often not aggressive enough to reach targets because of providers’ concerns
about adverse effects, tolerance, and patient adherence to specific medications (31).
The introduction
of panel management in primary care practices is an emerging proactive
systematic approach to improve care, for example, by identifying a list of the
provider’s patients with poorly controlled LDL for individualized outreach and
follow-up by the health care team (32).
Limitations of the study include recall bias and measurement error associated with self-report. The study strictly adhered to quality assurance procedures from NHANES
to limit response bias. Poststratification weighting on the basis of age group,
sex, race/ethnicity, and borough was applied to decrease the effect of component and item nonresponse. Additional analyses of treatment and control of LDL cholesterol within specific subgroups may have provided a deeper understanding of disparities but
were limited by sample size.
An unacceptably large proportion of the New York City population has high or uncontrolled LDL cholesterol. New York City adults who are at the greatest risk for CHD need aggressive medical intervention to reduce their LDL cholesterol levels. On a broader level, programs that address primary prevention of high cholesterol through changes in the food environment and tobacco policies
can prevent CHD-related illness and death and reduce health disparities.
Back to top
Acknowledgments
This study was funded by New York City tax levy dollars. We appreciate the review comments from Thomas R. Frieden, James L. Hadler, Lynn Silver, and Lorna Thorpe, and we gratefully acknowledge the NYC HANES participants and staff who made this study possible.
Back to top
Author Information
Corresponding Author: Elizabeth Needham Waddell, Bureau of Epidemiology Services, New York City Department of Health and Mental Hygiene, 125 Worth St, Room 315, CN No. 6, New York, NY 10013. Telephone: 212-788-9662. E-mail:
ewaddell@health.nyc.gov.
Author Affiliations: Ushma D. Upadhyay, New York City Department of Health
and Mental Hygiene, New York, New York, and University of California San Francisco School of Medicine, San Francisco, California. Stephanie Young, Bonnie D. Kerker,
Magdalena Berger, Thomas Matte, Sonia Y. Angell, New York City Department of
Health and Mental Hygiene, New York, New York.
Back to top
References
- Kung HC, Hoyert DL, Xu J, Murphy SL.
Deaths: final data for 2005. Natl Vital Stat Rep 2008;56(10):1-120.
- Domanski MJ.
Primary prevention of coronary artery disease. N Engl J Med 2007;357(15):1543-5.
- Stamler J, Daviglus ML, Garside DB, Dyer AR, Greenland P, Neaton JD.
Relationship of baseline serum cholesterol levels in 3 large cohorts of younger men to long-term coronary, cardiovascular, and all-cause mortality and to longevity. JAMA 2000;284(3):311-8.
- O’Keefe JH Jr, Cordain L, Harris WH, Moe RM, Vogel R.
Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. J Am Coll Cardiol 2004;43(11):2142-6.
- Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, et al.
Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. J Am Coll Cardiol 2004;44(3):720-32.
- Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, et al.
Explaining the decrease in US deaths from coronary disease, 1980-2000. N Engl J Med 2007;356(23):2388-98.
- Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, et al.
Trends in serum lipids and lipoproteins of adults, 1960-2002. JAMA 2005;294(14):1773-81.
- Hyre AD, Muntner P, Menke A, Raggi P, He J.
Trends in ATP III-defined high blood cholesterol prevalence, awareness, treatment and control among US adults. Ann Epidemiol 2007;17(7):548-55.
- Health, United States, 2007, with chartbook on trends in the health of Americans. National Center for Health Statistics; 2007. http://www.cdc.gov/nchs/data/hus/hus07.pdf. Accessed December 17, 2009.
- Mann D, Reynolds K, Smith D, Muntner P.
Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother 2008;42(9):1208-15.
- Angell SY, Garg RK, Gwynn RC, Bash L, Thorpe LE, Frieden TR.
Prevalence, awareness, treatment, and predictors of control of hypertension in New York City. Circ Cardiovasc Qual Outcomes 2008;1(1):46-53.
- Gwynn RC, Garg RK, Kerker BD, Frieden TR, Thorpe LE.
Contributions of a local health examination survey to the surveillance of chronic and infectious diseases in New York City. Am J Public Health 2009;99(1):152-9.
- Thorpe LE, Upadhyay UD, Chamany S, Garg R, Mandel-Ricci J, Kellerman S, et al.
Prevalence and control of diabetes and impaired fasting glucose in New York City. Diabetes Care 2009;32(1):57-62.
- National Cholesterol Education Program. Detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Bethesda (MD): National Institutes of Health; 2002.
- Thorpe LE, Gwynn RC, Mandel-Ricci J, Roberts S, Tsoi B, Berman L, et al. Study design and participation rates of the New York City Health and Nutrition Examination Survey, 2004. Prev Chronic Dis 2006;3(3).
http://www.cdc.gov/pcd/issues/2006/jul/05_0177.htm. Accessed December 17, 2009.
- National Health and Nutrition Examination Survey 2003-2004. US Department
of Health and Human Services, Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/nhanes03_04.htm.
Accessed January 29, 2010.
- Anderson KM, Wilson PW, Odell PM, Kannel WB.
An updated coronary risk profile. A statement for health professionals. Circulation 1991;83(1):356-62.
- Friedewald WT, Levy RI, Fredrickson DS.
Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18(6):499-502.
- Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected US population. Healthy People 2010 Stat Notes 2001(20):1-10. http://www.cdc.gov/nchs/data/statnt/statnt20.pdf. Accessed December 17, 2009.
- Mohadjer L, Montaquila J, Waksberg J. National Health and Nutrition Examination Survey III: weighting and examination methodology. Hyattsville (MD): National Center for Health Statistics; 1996.
- Screening for lipid disorders in adults. Agency for Healthcare Research and Quality; 2008. http://www.ahrq.gov/CLINIC/uspstf/uspschol.htm. Accessed December 17, 2009.
- US Census Bureau. Fact sheet. American Community Survey 3-Year Estimates American FactFinder; 2005-2007. http://factfinder.census.gov. Accessed December 31, 2009.
- Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington (DC): National Academies Press; 2003.
- Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR Jr.
Associations of the local food environment with diet quality — a comparison of assessments based on surveys and geographic information systems: the multi-ethnic study of atherosclerosis. Am J Epidemiol 2008;167(8):917-24.
- Despres JP.
Dyslipidaemia and obesity. Baillieres Clin Endocrinol Metab 1994;8(3):629-60.
- Scheffler E, Wiest E, Woehrle J, Otto I, Schulz I, Huber L, et al.
Smoking influences the atherogenic potential of low-density lipoprotein. Clin Investig 1992;70(3-4):263-8.
- Angell SY, Silver LD, Goldstein GP, Johnson CM, Deitcher DR, Frieden TR,
et al.
Cholesterol control beyond the clinic: New York City’s trans fat
restriction. Ann Intern Med 2009;151(2):129-34.
- Ellis JA, Perl SB, Frieden TR, Huynh M, Ramaswamy C, Gupta LS, et al.
Decline in smoking prevalence — New York City, 2002-2006. MMWR Morb Mortal Wkly Rep 2007;56(24):604-8.
- Frieden TR, Bassett MT, Thorpe LE, Farley TA.
Public health in New York City, 2002-2007: confronting epidemics of the modern era. Int J Epidemiol 2008;37(5):966-77.
- Ford I, Murray H, Packard CJ, Shepherd J, Macfarlane PW, Cobbe SM.
Long-term follow-up of the West of Scotland Coronary Prevention Study. N Engl J Med 2007;357(15):1477-86.
- Foley KA, Simpson RJ Jr, Crouse JR 3rd, Weiss TW, Markson LE, Alexander CM.
Effectiveness of statin titration on low-density lipoprotein cholesterol goal attainment in patients at high risk of atherogenic events. Am J Cardiol 2003;92(1):79-81.
- Neuwirth EB, Schmittdiel JA, Tallman K, Bellows J.
Understanding panel management: a comparative study of an emerging approach
to population care. The Permanente Journal 2007;11(3):12-20.
Back to top
|
|

![]()