

|

|

Volume 5:
No. 4, October 2008
ORIGINAL RESEARCH
Attempted Breastfeeding Before Hospital Discharge on Both Sides of the
US-Mexico Border,
2005: The Brownsville-Matamoros Sister City Project for Women’s Health
Brian C. Castrucci, MA, Leticia E. Piña Carrizales, MD, Denise V. D’Angelo, MPH, Jill A. McDonald, PhD, Hillary Foulkes, MPH, Indu B. Ahluwalia, PhD, Ginger L. Gossman, PhD, Juan Acuña, MD, MSc, Tracy Erickson, RD, LD, Kathy Clatanoff, RN, MSN, Kayan Lewis, PhD, Gita Mirchandani, PhD, MPH, Brian Smith, MD
Suggested citation for this article: Castrucci BC, Piña Carrizales LE, D’Angelo DV, McDonald JA, Foulkes H, Ahluwalia IB, et al. Attempted breastfeeding before hospital discharge on both sides of the
US-Mexico border,
2005: the Brownsville-Matamoros Sister City Project for Women’s Health. Prev Chronic Dis 2008;5(4).
http://www.cdc.gov/pcd/issues/2008/
oct/08_0058.htm. Accessed [date].
PEER REVIEWED
Abstract
Introduction
The US-Mexico border region has a growing population and limited health care infrastructure. Preventive health behaviors such as breastfeeding ease the burden on this region’s health care system by reducing morbidity and health care costs. We examined correlates of attempted breastfeeding before hospital discharge on each side of the
US-Mexico border and within the border region.
Methods
The cross-sectional study included women who delivered a live infant in Matamoros, Tamaulipas, Mexico (n = 489), and Cameron County, Texas (n = 457), which includes Brownsville, Texas. We interviewed women before hospital discharge from August 21 through November 9, 2005. We used multivariate logistic regression to estimate the odds of attempted breastfeeding before hospital discharge in Cameron County, Texas, the municipality of Matamoros, Mexico, and the 2 communities combined.
Results
Prevalence of attempted breastfeeding before hospital discharge was 81.9% in Matamoros compared with 63.7% in Cameron County. After adjusting for potential confounders, the odds of attempted breastfeeding before hospital discharge were 90% higher in Matamoros than in Cameron County (adjusted odds ratio [AOR],
1.93; 95% confidence interval [CI], 1.31-2.84 for the combined model). In the 2 communities combined, odds of attempted breastfeeding before hospital discharge were higher among
women who had a vaginal delivery than among women who had a cesarean delivery (AOR, 1.98; 95% CI, 1.43-2.75) and were lower among women who delivered infants with a low birth weight than among women who delivered infants with a normal birth weight (AOR, 0.26; 95% CI, 0.15-0.44).
Conclusion
The rate of attempted breastfeeding in Matamoros was significantly higher than in Cameron County. Additional breastfeeding support and messages on the
US side of the US-Mexico border are needed.
Back to top
Introduction
Between 1950 and 2000, the US-Mexico border population increased by
approximately 10 million people (1). This growth is expected to continue. Conservative estimates predict a 34% increase in population between 2000 and 2030, and more liberal estimates suggest a 97% increase (2). Population growth on the border has led to quality-of-life improvements such as paved streets and access to education. However, this population growth is also a potential burden on the health care system, which could result
in limited health care access and contribute to significant cross-border use of services (3,4). In a region with limited health care infrastructure, increasing the prevalence of preventive health behaviors such as breastfeeding may ease the burden on the health care system by reducing morbidity and health care costs.
Human milk is a more beneficial form of nutrition for infants than formula (5,6). Breastfeeding has proven short-term and long-term maternal and infant health benefits and reduces health care costs (5-10). Infants who are breastfed have reduced incidence and severity of several infectious diseases (5,6). Breastfeeding has been associated with a lower risk of childhood overweight and obesity, diabetes, asthma, and some cancers (5,6). Women who breastfeed
experience increased postpartum weight loss, decreased risk of women’s cancers, and possibly improved bone health during the postmenopausal period (5,6).
Studies of breastfeeding in the US-Mexico border region have focused on samples from the United States (11-23) and have explored acculturation (11-17) and the
effect of nativity, ethnicity, and immigration on breastfeeding rates (18-23). Interest in binational approaches to health promotion is increasing, and information is needed to assess the prevalence and correlates of breastfeeding in the border region. Despite this need, differences in data collection, measurement practices, and
confidentiality issues, stemming from legal and cultural restrictions, inhibit the sharing of information
across the US-Mexico border (24). We eliminated the challenges of binational data collection by using identical sampling and survey instruments on each side of the
US-Mexico border.
The purpose of this study was to determine the rates of attempted breastfeeding before hospital discharge among women who recently gave birth in the
US-Mexico border region, using data collected in 1 of 14 pairs of sister cities located on the
US-Mexico border: Brownsville, Texas, and Matamoros, Tamaulipas, Mexico (25)
(Figure).
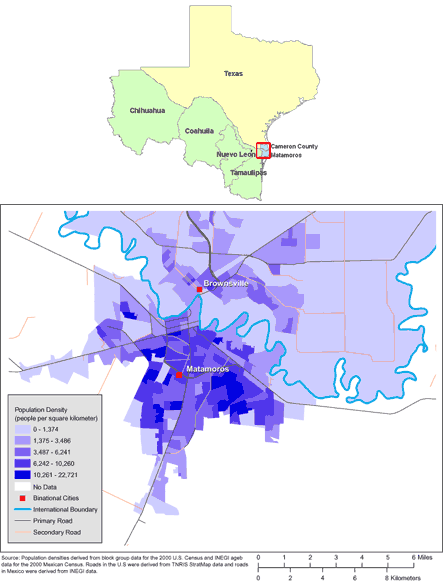
[
View enlarged image and descriptive text. ]
Figure. Maps of the US-Mexico Border Region (Top) and
of Brownsville, Texas, and Matamoros, Tamaulipas, Mexico (Bottom). (The authors
thank Allison Abell Banicki of the Office of Border Health, Texas Department of
State Health Services, for creating the map of the Texas-Mexico border states
and thank Jean W. Parcher, Sylvia N. Wilson, and the United States Geological
Survey [USGS] for providing the map of population density in Brownsville and
Matamoros.)
Back to top
Methods
Data collection
We used data that were collected as part of the Brownsville-Matamoros Sister City Project for Women’s Health (BMSCP).
The BMSCP pilot project was reviewed for human subject concerns by the Centers for Disease Control and Prevention (CDC) and was determined to be “nonresearch”
or public health practice. Therefore, institutional review board approval was not required. The study used a stratified, systematic, cluster-sampling probability design to select women who delivered live infants in Matamoros, Mexico, and Cameron County, Texas. Strata were hospitals with 100 deliveries or more per year in either location. We used systematic sampling to select specific days within each stratum, and every woman who gave birth on selected days
(within a cluster of days) was included in the sample. Of the 999 women sampled on selected days from August 21 through November 9, 2005 in hospitals with 100 or more deliveries per year, 947 (95%) completed interviews. A more thorough description of the data collection process and other methods used in the BMSCP
is available in this issue of Preventing Chronic Disease (26).
Measures
The outcome variable of interest was attempted breastfeeding before hospital discharge. Women were asked, “Have you ever tried to breastfeed your new baby?” One respondent did not provide a response for the outcome variable and was eliminated from the analysis. The final unweighted
sample was 946 women, distributed between Matamoros (n = 489) and Cameron County
(n = 457). A detailed list of measures used in this study is presented in
Table 1.
Data analysis
We weighted the data to account for probability of selection, population noncoverage, hospital noncoverage, and nonresponse. We used SUDAAN version 9.01 (RTI International, Research Triangle Park, North Carolina) to account for the complex survey design. Data were analyzed by place of residence and for the 2 communities combined. We used the χ2 test for independence to assess differences in the prevalence of attempted breastfeeding before hospital discharge between women
delivering in Matamoros and women delivering in Cameron County. Statistical significance was set at α = .05. We could not assess differences between either community and the overall combined sample because the combined data were a composite of the data from the individual communities, and observations were not independent.
To quantify the difference in the odds of attempted breastfeeding before hospital discharge by selected sociodemographic characteristics, health behaviors, and perinatal/delivery experiences, we used logistic regression analysis. Variables that were statistically significant (P <.05) in the bivariate analyses were included in the multivariate logistic regression models. In addition to these variables, we included variables that approached significance (P <.10 and >.05)
in the logistic regression models to account for other potential sources of variance and confounders. Only variables with at least 30 cases unweighted per level were considered in the logistic regression analysis. Models were estimated separately for Cameron County and Matamoros and for the combined sample.
Back to top
Results
Distribution of demographic and behavioral variables, by place of residence, is presented in
Table 2. Although only 5.0% of all Matamoros residents delivered in the United States, all Cameron County residents, with the exception of 1, delivered their infants in the United States. Nearly all residents in Matamoros completed the interview in Spanish. In Cameron County, the language in which the interview was completed was approximately evenly distributed between English and Spanish. The
ethnicity of respondents from Cameron County was primarily Hispanic. Despite having a greater percentage of respondents report early entry into prenatal care, the percentage of low-birth-weight infants was higher in Cameron County than in Matamoros.
Sociodemographic characteristics and attempted breastfeeding
In Matamoros, the rate of attempted breastfeeding before hospital discharge was higher among respondents with fewer years of education
(Table 3). In the multivariate model, respondents in Matamoros with fewer than 8 years of education were nearly twice as likely to attempt breastfeeding as were respondents with more than 12 years of education (Table 4). Respondents in Matamoros with 8
to 12 years of education were almost 3 times as likely to attempt breastfeeding as were respondents
with more than 12 years of education.
The prevalence of attempted breastfeeding was 81.9% among the women who lived in Matamoros, compared with 63.7% among the women who lived in Cameron County (data not shown). In the multivariate analysis, residing in Matamoros was associated with nearly a
2-fold increase in the odds of attempted breastfeeding before hospital discharge (Table 4).
In Cameron County, non-Hispanic women had a greater prevalence of attempted breastfeeding before hospital discharge than did
Hispanic women. After adjusting for other factors, Hispanic women who resided in Cameron County had decreased odds of attempted breastfeeding before hospital discharge compared with non-Hispanic women in Cameron County.
Perinatal experiences
Women who delivered vaginally had increased prevalence and odds of attempted breastfeeding in Matamoros and in the 2 communities combined (Tables 3 and 4). Prevalence of attempted breastfeeding was higher among women who delivered vaginally in Cameron County, but odds of attempted breastfeeding
among these same women were not significant in the multivariate model.
In Matamoros, Cameron County, and the 2 communities combined, women who delivered a low-birth-weight infant (ie, <2,500 g) had a lower rate of attempted breastfeeding before hospital discharge than did women who delivered an infant of normal weight (ie, ≥2,500 g) (Table 3). In each of the multivariate logistic regression models, women who delivered a low-birth-weight infant were
approximately 75% less likely to have attempted breastfeeding before hospital discharge than were women who
delivered infants of normal weight (Table 4).
Women with any previous live births had a higher prevalence of attempting to breastfeed in Matamoros, but the same was not true in Cameron County (Table 3). In the multivariate logistic regression model, women in Matamoros who had a previous live birth were nearly twice as likely to attempt breastfeeding before hospital discharge as were women who had not had a previous live birth. However, this was not true of the women in Cameron County (Table 4).
In Cameron County and in the 2 communities combined, women who indicated that their pregnancy was intended had a higher prevalence of attempted breastfeeding before hospital discharge than did women who indicated that their pregnancy was unintended (Table 3). In the multivariate logistic regression model, the odds of attempted breastfeeding before hospital discharge were 50% lower among women who identified their pregnancy as unintended than among women with intended pregnancies. In the
combined model, the decrease in odds was 34% (Table 4).
Back to top
Discussion
The prevalence of attempted breastfeeding before hospital discharge was nearly 20 percentage points higher in Matamoros than in Cameron County, and the adjusted odds of attempted breastfeeding before hospital discharge among Matamoros residents were nearly twice the odds among Cameron County residents. The rates we report in Matamoros and Cameron County are lower than previously reported state rates on both sides of the
US-Mexico border. Rates of ever breastfeeding in Texas have been
reported to be 75% (27), and rates of ever breastfeeding in northern Mexico, an area that includes Tamaulipas, have been reported to be 91% (28). These statistics suggest that breastfeeding rates in border areas may be lower than
statewide rates.
Most women’s first breastfeeding experience occurs in the hospital environment, and exclusive breastfeeding rates decline substantially
after hospital discharge. Failure to establish breastfeeding during the hospital stay is a factor in breastfeeding cessation following hospital discharge (29). Although the importance of breastfeeding is highlighted in the United States at the national level in documents like Healthy People 2010 (30), no national policy exists to support
breastfeeding.
Unlike the United States, Mexico has federal regulations that support breastfeeding. Mexico’s official norms for breastfeeding, or Ministry of Health clinical practice guidelines (La Norma Oficial Mexicana), support breastfeeding initiation within the first 2 hours
after delivery when conditions permit; support and facilitate breastfeeding on infant demand; and include standards, criteria, and procedures that promote and protect exclusive breastfeeding (eg, standards for
training and personnel, requirements that medical units provide appropriate conditions to enable mothers to practice exclusive breastfeeding and to educate mothers about the benefits of exclusive breastfeeding) (31). CAALMA Curso, a training program for hospital personnel, has been implemented throughout Mexico to support these federal regulations (32).
A study in Texas among WIC (Supplemental Nutrition Program for Women, Infants, and Children) recipients who breastfed found that 55% of women were not informed that breastfeeding could occur at the demand of the infant, 56% of women did not initiate breastfeeding in the first hour after delivery, and 74% of women reported their infants were fed something in addition to breast milk (33). At least
1 US study found that hospitals that adopted supportive breastfeeding policies have
more patients who breastfeed and who breastfeed longer (34).
Another difference between the United States and Mexico is the provision of infant formula
in hospitals. Federal regulations in Mexico restrict the distribution of formula in the hospital, the free distribution or promotion of breast milk substitutes by medical units, and the distribution of incentives to health care providers from the manufacturers of breast milk substitutes (31). Furthermore, in September 2007, an agreement (Acuerdo con Productores de Alimentos y Fórmulas
Infantiles) was reached with Mexican health officials and manufacturers of
infant formula to restrict the distribution of formula in the hospital, the free
distribution or promotion of breast milk substitutes by medical units, and the
distribution of incentives to health care providers from the manufacturers of
breast milk substitutes (Cuitlahuac Ruiz Matus, MD, written communication, February 14, 2008). Similar regulations are not in place in the United States. In Texas, nearly three-quarters of women
who received WIC benefits
reported receiving formula before hospital discharge.
Women in our study who delivered infants weighing ≥2,500 g had increased odds of breastfeeding in Matamoros, Cameron County, and in the combined sample. Women who delivered vaginally had increased odds of breastfeeding in Matamoros and in the combined sample. These findings are consistent with previous studies and identify opportunities for cross-border collaboration (35-38). Cross-border work groups may design continuing education for providers or develop protocols and best practices
that address the unique breastfeeding needs of women who deliver infants weighing <2,500 g or who
have a cesarean delivery. In Mexico, strategies and best practices to increase breastfeeding among women in these vulnerable groups could be disseminated through the CAALMA Curso.
Women who did not intend to become pregnant had decreased odds of attempted breastfeeding before hospital discharge in Cameron County and in the combined sample. Previous research on this association has shown mixed results (39-41). At least
1 study found an association between pregnancy intention and attempted breastfeeding before hospital discharge in the United States (40). However, studies in Bolivia and Paraguay did not find an association between these variables (40,41). Although
practitioners should discuss breastfeeding with all pregnant women, more education and counseling may be needed for women whose pregnancy is unintended.
Our study has 2 limitations. The first limitation was with regard to duration of hospital stay. Women who delivered in Matamoros were typically discharged on the same day of their delivery, and women who delivered in Cameron County typically remained hospitalized for up to 48 hours
after delivery. Therefore, women who delivered in Cameron County had more time to attempt to breastfeed than did women who delivered in Matamoros. Despite this difference, women who delivered in Matamoros
still attempted to breastfeed at a greater rate than did women who delivered in Cameron County, suggesting that differences on the basis of place of residence would be larger if the
length of hospital stay
after delivery
were equal. The second limitation is that previous infant feeding method was not included in the questionnaire. However, the exclusion of this variable most likely affected point estimates within the 2 locations rather than the estimate associated with place of residence.
If breastfeeding rates reached the goal of 75% in the early postpartum period established in Healthy People 2010 (29), the potential cost savings could exceed $1 billion (10). Results from this study are encouraging for Matamoros but indicate a need for additional breastfeeding support and messages in Cameron County. Because of the cross-border mobility of the population, joint
US-Mexico strategies to promote breastfeeding are needed.
Back to top
Acknowledgments
The BMSCP was funded through the Division of Reproductive Health and the Office of Global Health Promotion at the National Center for Chronic Disease Prevention and Health Promotion, CDC, under a cooperative agreement with the United States-Mexico Border Health Association, No. U65 CCU 623699-01-2, and through interagency personnel agreements with the University of Texas at Brownsville and Texas Southmost College and the University of Texas-Houston
School of Public Health, Brownsville Regional Campus. In-kind project support was provided by the Division of Health Examination Statistics at the National Center for Health Statistics, CDC; the Texas Department of State Health Services, Region 11; the Secretariat of Health, Tamaulipas; and the Mexican Institute of Social Security, Tamaulipas.
In addition to contributions from these partners, support from the following local, regional, and national institutions was critical to the
project: the National Center for Gender Equity and Reproductive Health, Mexican Health Secretariat; National Center for Epidemiologic Surveillance and Disease Control, Mexican Health Secretariat; National Center for Health Promotion, Mexican Health Secretariat; National Institute of Statistics, Geography and Informatics, Tamaulipas; Civil Registry, Tamaulipas; Institute of Social Security Serving State Workers, Tamaulipas; Secretariat of Health, Jurisdiction III, Tamaulipas;
Texas Department of State Health Services, Region 11, and Office of Border Health; City of Brownsville Department of Public Health; Cameron County Health Department; Valley Baptist Medical Center in Harlingen; Valley Baptist Medical Center in Brownsville; Valley Regional Medical Center; Harlingen Medical Center; Cameron Park Cultural Center; Brownsville Community Health Center; General Hospital of Matamoros “Dr. Alfredo Pumarejo Lafaurie”; Mexican Institute of Social Security General Hospital,
Zone 13, Matamoros; Dr Manuel F. Rodríguez Brayda Clinical Hospital, Matamoros; Hospital Guadalupe; Matamoros Center of Family Orientation; Medical Center of Surgical Specialties of Matamoros; and the United States-Mexico Border Health Commission. Special thanks to the National Center for Gender Equity and Reproductive Health, Secretariat of Health, Mexico, for review of this manuscript and to the United States-Mexico Border Health Commission for providing the English-Spanish translation.
The findings and conclusions of this article are those of the authors and do not necessarily represent the views of the Texas Department of State Health Services or other institutions with which the authors are affiliated.
Back to top
Author Information
Corresponding Author: Brian C. Castrucci, MA, Office of Title V, Division of Family and Community Health Services, Texas Department of State Health Services, 1100 West 49th St, Austin,
TX 78756. Telephone: 512-458-7111, ext 2006. E-mail: brian.castrucci@dshs.state.tx.us.
Author Affiliations: Leticia E. Piña Carrizales, Jurisdiction III, Secretariat of Health, Tamaulipas, Mexico; Denise V. D’Angelo, Jill A. McDonald, Juan Acuña, Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), Centers for Disease Control and Prevention (CDC), Atlanta, Georgia; Hillary Foulkes, Ginger L. Gossman, Kathy Clatanoff, Kayan Lewis, Gita Mirchandani, Office of Title V, Division of Family and Community
Health Services, Texas Department of State Health Services, Austin, Texas; Indu B. Ahluwalia, Division of Adult and Community Health, NCCDPHP, CDC, Atlanta, Georgia; Tracy Erickson, Nutrition Services Section, Division of Family and Community Health Services, Texas Department of State Health Services, Austin, Texas; Brian Smith, MD, Region 8 Medical Director, Division of Regional and Local Health Services, Texas Department of State Health Services, Harlingen, Texas.
Back to top
References
- Anderson JB. The U.S.-Mexico border: a half century of change. Soc Sci J 2003;40:535-54.
- Peach J, Williams J. Population dynamics of the US-Mexican border region. San Diego (CA):
Southwest Center for Environmental Research and Policy; 2003. http://www.scerp.org/population.htm.
Accessed December 2, 2007.
- Brandon JE, Crespin F, Levy C, Reyna DM. Border health issues. In: Bruhn
JG, Brandon JE, editors. Border health: challenges along the U.S.-Mexico border.
New York (NY): Garland Press; 1997.
- Health care: availability in the Texas-Mexico border area. GAO Document # HRD-89-12. Washington
(DC): Governmental Accounting Office; 1988.
- Gartner LM, Morton J, Lawrence RA, Naylor AJ, O'Hare D, Schanler RJ, et al.
Breastfeeding and the use of human milk. Pediatrics 2005;115(2):496-506.
- Goldman AS, Hopkinson JM, Rassin DK.
Benefits and risks of breastfeeding.
Adv Pediatr 2007;54:275-304.
- Ball TM, Wright AL.
Health care costs of formula-feeding in the first year of life. Pediatrics 1999;103(4
Pt 2):870–6.
- Montgomery DL, Splett PL.
Economic benefit of breast-feeding infants enrolled in WIC. J Am Diet Assoc 1997;97(4):379–85.
- Tuttle CR, Dewey KG.
Potential cost savings for Medi-Cal, AFDC, food stamps, and WIC programs associated with increasing breast-feeding among low-income Hmong women in California. J Am Diet Assoc 1996;96(9):885–90.
- Weimer D. The economic benefits of breastfeeding: a review and analysis.
Food Assistance and Nutrition Research Report No. 13. Washington (DC): U.S. Department
of Agriculture; 2001.
- Harley K, Stamm NL, Eskenazi B.
The effect of time in the U.S. on the duration of breastfeeding in women of Mexican
descent. Matern Child Health J 2007;11(2):119-25.
- Gibson MV, Diaz VA, Mainous AG 3rd, Geesey ME.
Prevalence of breastfeeding and acculturation in Hispanics: results from NHANES 1999-2000 study. Birth 2005;32(2):93-8.
- Libbus MK.
Breastfeeding attitudes in a sample of Spanish-speaking Hispanic American women. J Hum Lact 2000;16(3):216-20.
- Kaiser LL, Melgar-Quiñonez HR, Lamp CL, Johns MC, Harwood JO.
Acculturation of Mexican-American mothers influences child feeding strategies. J Am Diet Assoc 2001;101(5):542-7.
- Byrd TL, Balcazar H, Hummer RA.
Acculturation and breast-feeding intention and practice in Hispanic women on the US-Mexico border. Ethn Dis 2001;11(1):72-9.
- Rassin DK, Markides KS, Baranowski T, Richardson CJ, Mikrut WD, Bee DE.
Acculturation and the initiation of breastfeeding. J Clin Epidemiol 1994;47(7):739-46.
- Rassin DK, Markides KS, Baranowski T, Bee DE, Richardson CJ, Mikrut WD, et al.
Acculturation and breastfeeding on the United States-Mexico border. Am J Med Sci 1993;306(1):28-34.
- Merewood A, Brooks D, Bauchner H, MacAuley L, Mehta SD.
Maternal birthplace and breastfeeding initiation among term and preterm infants: a statewide assessment for Massachusetts. Pediatrics 2006;118(4):e1048-54.
- Singh GK, Kogan MD, Dee DL.
Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics 2007;119(Suppl 1):S38-46.
- Gibson-Davis CM, Brooks-Gunn J.
Couples’ immigration status and ethnicity as determinants of breastfeeding. Am J Public Health 2006;96(4):641-6.
- Celi AC, Rich-Edwards JW, Richardson MK, Kleinman KP, Gillman MW.
Immigration, race/ethnicity, and social and economic factors as predictors of breastfeeding initiation. Arch Pediatr Adolesc Med 2005;159(3):255-60.
- Balcazar H, Trier CM, Cobas JA.
What predicts breastfeeding intention in Mexican-American and non-Hispanic white women? Evidence from a national survey. Birth 1995;22(2):74-80.
- Smith JC, Mhango CG, Warren CW, Rochat RW, Huffman SL.
Trends in the incidence of breastfeeding for Hispanics of Mexican origin and Anglos on the U.S.-Mexico border. Am J Public Health 1982;72(1):59-61
- Barriers to binational cooperation in public health between Texas and Mexico.
Austin (TX): Texas Department of State Health Services. http://www.dshs.state.tx.us/borderhealth/legis_rpts.shtm. Accessed April 7, 2008.
- Mortality profiles of the sister communities on the United States — Mexico
border, 2000 edition. Washington (DC): Pan American Health Organization; 2000.
- McDonald JA, Johnson CH, Smith R, Folger SG, Chavez AL, Mishra N, et al. Reproductive health surveillance in
the US-Mexico border region, 2003-2006: the Brownsville-Matamoros Sister
City Project for Women’s Health. Prev Chronic Dis 2008;5(4).
http://www.cdc.gov/pcd/issues/2008/oct/08_0055.htm.
- Centers for Disease Control and Prevention.
Breastfeeding trends and updated national health objectives for exclusive
breastfeeding — United States, birth years 2000-2004. MMWR Morb Mortal
Wkly Rep 2007;56(30):760-3.
- González-Cossío T, Moreno-Macías H, Rivera JA, Villalpando S, Shamah-Levy
T, Monterrubio EA, et al.
Breast-feeding practices in Mexico: results from the Second National Nutrition Survey 1999.
Salud Publica Mex 2003;45(Suppl 4):S477-89.
- Harrod-Wild K.
Lessons from the latest infant feeding survey. J Fam Health Care 2007;17(5):153-4.
- Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health. 2 vols. Washington
(DC): U.S. Department of Health and Human Services; 2000.
- Atención de la mujer durante el embarazo, parto y puerperio y del recién nacido. Criterios y procedimientos para la prestación del servicio. Norma Oficial
Mexicana. NOM-007-SSA2-1993.
- Argomedo AL, Bribiesca F, Reyes-Vazquez H, et al. CAALMA Curso, avanzado de apoyo a la lactancia materna. Conepeme; 2005.
- Breastfeeding beliefs, attitudes, and practices in the Texas WIC population:
findings from the 2006 Infant Feeding Survey. Austin (TX): Texas Department
of State Health Services; 2006. http://www.dshs.state.tx.us/wichd/nut/pdf/InfantFeedingPracticesSurvey.pdf.
Accessed December 2, 2007.
- Murray EK, Ricketts S, Dellaport J.
Hospital practices that increase breastfeeding duration: results from a population-based study. Birth 2007;34(3):202-11.
- Meier PP, Brown LP.
State of the science. Breastfeeding for mothers and low-birth-weight infants. Nurs Clin North Am 1996;31(2):351-65.
- Callen J, Pinelli J.
A review of the literature examining the benefits and challenges, incidence and duration, and barriers to breastfeeding in preterm infants. Adv Neonatal Care 2005;5(2):72-88.
- Rowe-Murray HJ, Fisher JR.
Baby friendly hospital practices: cesarean section is a persistent barrier to early initiation of breastfeeding. Birth 2002;29(2):124–31.
- Rowe-Murray HJ, Fisher JR.
Operative intervention in delivery is associated with compromised early mother-infant interaction. BJOG 2001;108(10):1068–75.
- Taylor JS, Cabral HJ.
Are women with an unintended pregnancy less likely to breastfeed? J Fam Pract 2002;51(5):431-6.
- Shapiro-Mendoza C, Selwyn BJ, Smith DP, Sanderson M.
Parental pregnancy intention and early childhood stunting: findings from Bolivia. Int J Epidemiol 2005;34(2):387-96.
- Shapiro-Mendoza CK, Selwyn BJ, Smith DP, Sanderson M.
The impact of pregnancy intention on breastfeeding duration in Bolivia and Paraguay. Stud Fam Plann 2007;38(3):198-205.
Back to top
|
|
