Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Mumps Outbreak --- New York, New Jersey, Quebec, 2009
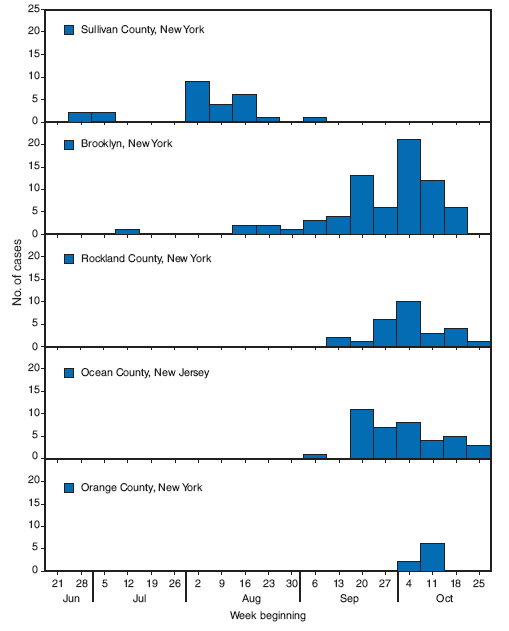
Mumps is a vaccine-preventable viral infection characterized by fever and inflammation of the salivary glands and whose complications include orchitis, deafness, and meningo-encephalitis (1). In August 2009, CDC was notified of the onset of an outbreak of mumps in a summer camp in Sullivan County, New York. The outbreak has spread and gradually increased in size and is now the largest U.S. mumps outbreak since 2006, when the United States experienced a resurgence of mumps with 6,584 reported cases (2). On August 18, public health departments in Sullivan County, New York state, and CDC began an investigation into the mumps outbreak, later joined by departments in New York City and other locales. As of October 30, a total of 179 confirmed or probable cases had been identified from multiple locations in New York and New Jersey (Figure), and an additional 15 cases had been reported from Canada. The outbreak primarily has affected members of a tradition-observant religious community; median age of the patients is 14 years, and 83% are male. Three persons have been hospitalized. Although little transmission has occurred outside the Jewish community, mumps can spread rapidly in congregate settings such as colleges and schools; therefore, public health officials and clinicians should heighten surveillance for mumps and ensure that children and adults are appropriately vaccinated.
Mumps cases in the United States have been classified according to the 2008 case definition of the Council of State and Territorial Epidemiologists,* and cases in Canada have been classified in accordance with Case Definitions for Diseases Under National Surveillance.† Patients in the United States are considered to have age-appropriate vaccinations for mumps if they are aged 1--6 years and have received 1 dose of a mumps-containing vaccine, aged 7--18 years and have received 2 doses of vaccine, or aged 19--52 years and have received 1 dose of vaccine (3,4). Patients aged 7--18 years who have received 1 dose are considered to have received a partially age-appropriate vaccination.
Outbreak Reports
Sullivan County, New York. On August 18, 2009, the New York State Department of Health was notified of mumps cases in a summer camp serving approximately 400 boys from the tradition-observant religious community. The index patient was a boy aged 11 years who had returned on June 17 from the United Kingdom, where a mumps outbreak is ongoing with approximately 4,000 cases, primarily in unvaccinated young adults in the general population.§ The boy became symptomatic at camp on June 28. A total of 25 cases were reported among camp attendees and staff members. The median age of patients was 12 years (range: 9--30 years), and all were male. Of the 24 patients for whom vaccination status was reported, 20 (83%) had received age-appropriate vaccination with 2 doses, one (4%) had received partial age-appropriate vaccination with 1 dose, and three (13%) were unvaccinated. The attack rate in this camp was approximately 6% (25 of 400).
Brooklyn, New York. The majority of campers were residents of the Borough Park neighborhood of Brooklyn, where mumps transmission began after their return home from camp. Although returning campers were implicated in most of the initial exposures, no predominant focus of spread was identified. By October 30, 79 additional persons from Brooklyn or other boroughs who were linked to the outbreak had been reported, exclusive of returning campers. The median age of these patients was 14 years (range: 8 months--84 years), and 81% were male. Of the 61 patients (77%) for whom vaccine is recommended and vaccination status and age were reported, 47 (77%) had received age-appropriate vaccination, six (10%) had received partial age-appropriate vaccination, and eight (13%) were unvaccinated.
Ocean County, New Jersey. On September 26, the New Jersey Department of Health and Senior Services was informed of eight suspected mumps cases in two Ocean County private schools for boys with both boarder and commuter students from the same religious community. The index patient, who became symptomatic at one of the boarding schools on September 6, was aged 20 years and a resident of the Borough Park neighborhood of Brooklyn, New York. Transmission was initially limited to the schools but subsequently was observed in households and the community. By October 30, a total of 40 cases had been reported. The median age of patients was 19.5 years (range: 1--65 years), and 83% were male. Mumps vaccination status was reported for 29 (73%) patients, of whom 28 (97%) had received age-appropriate vaccination.
Rockland County, New York. Four of the patients who had attended the Sullivan County summer camp resided in Rockland County, New York. By October 30, an additional 27 cases (exclusive of returning campers) had been reported among members of the same religious community, with transmission occurring in a variety of settings, including a school for boys. The median age of patients was 12 years (range: 1--62 years), and 23 (85%) were male. Mumps vaccination status was reported for 19 (70%), of whom 11 had received age-appropriate vaccination, and two had received partial age-appropriate vaccination.
Orange County, New York. In September, members of the same religious community in Orange County visited a synagogue in Brooklyn. During October 8--14, eight cases occurred among the travelers. The median age of patients was 18 years (range: 11--23 years), and five were male. Seven patients had received age-appropriate vaccination with 2 doses, and one was unvaccinated.
Quebec, Canada. Members of affected New York and New Jersey communities traveled to the province of Quebec to attend religious gatherings during September 19--October 11. By October 30, 15 cases (patient age range: 8--47 years) from Montreal and the Laurentian region of the province had been reported to the Public Health Agency of Canada. All patients were male, and 11 had documented vaccination with at least 1 dose of mumps-containing vaccine.
Transmission Outside the Religious Community
During June 28--October 30, five cases outside the affected religious community were reported. Two cases occurred in New York City, and three occurred in Ocean County, New Jersey. The two New York City patients were a man aged 40 years who had probable worksite exposures to members of the affected community and a boy aged 4 years who had no identified exposure. The three New Jersey cases were patients aged 17, 29, and 66 years who had no identified exposures. Two of the five patients had received 2 documented doses of mumps-containing vaccine, one had received 2 undocumented doses, and two had unknown vaccination status.
Laboratory Testing
Of the 179 cases reported as of October 30 in the United States, 85 (47%) have been laboratory-confirmed, and the remaining 94 cases (53%) have met the clinical case definition. Laboratory tests used to confirm cases of mumps included detection of mumps immunoglobulin M antibodies by various methods, detection of mumps RNA by real-time reverse transcription--polymerase chain reaction (5), and isolation of mumps virus in cell culture. These tests were conducted by CDC and state and commercial laboratories. Mumps virus classified as genotype G was identified from multiple specimens sent to CDC, consistent with the probable importation of mumps into Sullivan County from the ongoing mumps outbreak in the United Kingdom (6).
Epidemiologic Summary
Of the 178 (99%) patients whose sex is known, 149 (84%) are male. The median age of the 178 patients for whom age is known is 14 years (range: 8 months--84 years). Of the 141 patients (79%) for whom vaccine is recommended and vaccination status and age were reported, 113 (80%) had received age-appropriate vaccination, nine (6%) had received partial age-appropriate vaccination, and 19 (13%) were unvaccinated (Table). Of the 141 patients, 102 (72%) had received 2 doses, 20 (14%) 1 dose, and 19 (13%) zero doses (Table). Complications have occurred in 16 (9%) cases, including orchitis (15 cases) and temporary deafness (1 case). Three hospitalizations for orchitis have been reported. No deaths have occurred.
Response Measures
Health officials issued alerts in New Jersey, New York City, and elsewhere in New York state to health-care providers, urging them to increase active surveillance for mumps, to consider mumps diagnoses even if patients had documented vaccinations and, when indicated, to perform appropriate diagnostic testing. Isolation and quarantine procedures were reviewed, and health-care providers were urged to ensure that all children and adults were appropriately vaccinated.
Reported by: P High, MPH, Ocean County Health Dept, EF Handschur, MPH, OS Eze, MD, B Montana, MD, C Robertson, MD, C Tan, MD, New Jersey Dept of Health and Senior Svcs. JB Rosen, MD, KP Cummings, MPH, MK Doll, MPH, JR Zucker, MD, CM Zimmerman, MD, New York City Dept of Health and Mental Hygiene. T Dolinsky, Rockland County Dept of Health. S Goodell, MPH, Orange County Health Dept. C Schulte, D Blog, MD, New York State Dept of Health. MA Leblanc, Ministère de la santé et des services sociaux du Québec. YA Li, MD, Public Health Agency of Canada. A Barskey MPH, G Wallace, MD, K Gallagher, DSc, G Armstrong, MD, L Lowe, MS, R McNall, PhD, J Rota, MPH, P Rota, PhD, C Hickman, PhD, WJ Bellini, PhD, Div of Viral Diseases, National Center for Immunization and Respiratory Diseases. A Apostolou, PhD, EIS Officer, CDC.
Editorial Note:
Before routine mumps vaccination was initiated, most persons acquired infection during childhood. In 1967, a live, attenuated mumps virus vaccine was licensed in the United States, and by 2005 high coverage with 2 doses among children had reduced the incidence of mumps by 99% (2). In 2006, a resurgence occurred in the United States, with the highest attack rate among persons aged 18--24 years; 57% of patients had previously received 2 doses of vaccine (2). In 2007 and 2008, incidence declined to 800 and 454 cases, and outbreaks involved fewer than 20 cases.
The ongoing mumps outbreak is the largest since 2006 and primarily has affected a tradition-observant religious community. Mumps outbreaks perpetuated by community transmission outside of congregate settings (e.g., camps, schools, and colleges) are unusual in highly-vaccinated populations (2). In this outbreak, the limited transmission of mumps into the general population might be attributable to generally high vaccination levels and little interaction between members of the affected religious community and persons in surrounding communities. Vaccination rates in the religious community in this outbreak have not been measured, but according to the 2008 National Immunization Survey, overall age-appropriate mumps vaccination rates for children in New York City, New York state, and New Jersey were high: ≥90% for receipt of 1 dose among children aged 19--35 months and ≥90% for receipt of 2 doses among adolescents aged 13--17 years.¶ However, mumps incidence commonly peaks in the winter (2), and vaccine-preventable diseases have spread from religious communities to the general population during the peak transmission season (7).
Of those patients in this outbreak whose vaccination status was known, 72% had received 2 doses of mumps-containing vaccine, compared with 57% in the 2006 outbreak. Mumps vaccine effectiveness has been estimated at 73%--91% for 1 dose and 76%--95% for 2 doses (8,9). Studies during the 2006 U.S. mumps resurgence suggested that outbreaks could occur among highly-vaccinated populations such as college students, where frequent close contact occurs and where >10 years have passed since most of the population received a second dose (9). However, even in such settings, attack rates were <8% in 2006 for those with 2 doses, suggesting that the vaccine was highly effective in preventing disease for the vast majority of those exposed (9). In the current outbreak, the attack rate at the summer camp was approximately 6%.
Because 43% of the world's nations have no mumps vaccination program (10), and certain nations with mumps vaccination programs, such as the United Kingdom, have experienced large-scale outbreaks, the risk for mumps exposure is increased with foreign travel. When importations occur, congregate settings in the United States, such as colleges and schools, have been foci of indigenous mumps transmission (2).
When possible, persons with suspected mumps should be isolated for 5 days after onset of parotitis and, if they visit a health-care setting, droplet precautions should be initiated immediately. Clinical specimens (both serum and buccal swabs) should be collected from persons with suspected mumps as soon as possible after symptom onset. Adults and children should receive age-appropriate vaccination. University students, health-care personnel, and persons with potential mumps outbreak exposure should have documentation of 2 doses of mumps vaccine or other proof of immunity to mumps. Although vaccination is not considered effective postexposure prophylaxis for mumps, nonimmune contacts should be vaccinated with measles, mumps, rubella (MMR) vaccine to prevent risk from subsequent exposures. Any suspected mumps case should be reported to the health department in the area where the patient resides. Additional information regarding mumps vaccination is available at http://www.cdc.gov/vaccines/vpd-vac/mumps/default.htm#recs.
References
- Plotkin SA, Rubin SA. Mumps vaccine. In: Plotkin SA, Orenstein WA, Offit PA, eds. Vaccines. 5th ed. Philadelphia, PA: Elsevier; 2008:435--65.
- Barskey AE, Glasser JW, LeBaron CW. Mumps resurgences in the United States: a historical perspective on unexpected elements. Vaccine 2009;27:6186--95.
- CDC. Measles, mumps, and rubella--vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1998;47(No. RR-8).
- CDC. Updated recommendations of the Advisory Committee on Immunization Practices (ACIP) for the control and elimination of mumps. MMWR 2006;55:629--30.
- Boddicker JD, Rota PA, Kreman T, et al. Real-time reverse transcription-PCR assay for detection of mumps virus RNA in clinical specimens. J Clin Microbiol 2007;45:2902--8.
- Rota JS, Turner JC, Yost-Daljev MK, et al. Investigation of a mumps outbreak among university students with two measles-mumps-rubella (MMR) vaccinations, Virginia, September--December 2006. J Med Virol 2009;81:1819--25.
- Parent du Chatelet I, Floret D, Antona D, Levy-Bruhl D. Measles resurgence in France in 2008, a preliminary report. Eurosurveillance 2009;14(6):5--7.
- Dayan GH, Rubin S. Mumps outbreaks in vaccinated populations: are available mumps vaccines effective enough to prevent outbreaks? Clin Infect Dis 2008; 47:1458--67.
- Marin M, Quinlisk P, Shimabukuro T, Sawhney C, Brown C, LeBaron CW. Mumps vaccination coverage and vaccine effectiveness in a large outbreak among college students---Iowa, 2006. Vaccine 2008;26:3601--7.
- World Health Organization. Global status of mumps immunization and surveillance. Wkly Epidemiol Rec 2005;80:418--24.