 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Injury and Illness Surveillance in Hospitals and Acute-Care Facilities After Hurricanes Katrina and Rita --- New Orleans Area, Louisiana, September 25--October 15, 2005In response to Hurricane Katrina, CDC and the Louisiana Department of Health and Hospitals (LDHH) implemented active surveillance on September 9, 2005, to monitor for injuries and illnesses at functioning hospitals and other acute-care facilities in the greater New Orleans area (Jefferson, Orleans, Plaquemines, St. Bernard, St. Charles, and St. Tammany parishes) (1,2). On September 20, the system was interrupted because of mandatory evacuation for Hurricane Rita. Surveillance was reestablished on September 24, and repopulation of Orleans Parish began on September 30. This report updates a previous report (3) on injuries and illness surveillance during September 8--25, 2005, after Hurricane Katrina and describes frequencies of these events during the days after Hurricane Rita and during repopulation of the city. The results indicate that 17,446 visits occurred at participating facilities during this period. Whereas the proportion of relief workers who had acute respiratory illnesses and unintentional injuries was higher compared with residents, the proportion of falls and motor-vehicle crashes among relief workers was lower. Moreover, although the collection of detailed data using a paper-based active surveillance system was required in response to Hurricane Katrina, the burden of this system required the implementation of an electronic syndromic surveillance system, which is more sustainable. Data were collected prospectively for the period September 25--October 15, 2005. Eight hospitals and 19 acute-care clinics (i.e., staffed by disaster medical assistance teams [DMATs]) located in greater New Orleans participated in the system; one hospital and four acute-care clinics had been deactivated (i.e. closure of acute-care clinics staffed by DMATs) after Hurricane Rita. Because no access to electronic data was possible, a standardized paper case-report form (CRF) was used to collect patient-specific data regarding demographics, symptoms, clinical impressions, and mechanism of injury. CRFs were completed by health-care providers and entered into a computer database by surveillance staff. Data were analyzed every 24 hours for trends or aberrations in illness and injury categories and for single cases of select illnesses (e.g., rash illness), which were reported to city and state health authorities for investigation (3). With the assistance of infection-control professionals, follow-up investigations were conducted for any aberrations detected through daily analysis and review of the data. Because baseline data were unavailable, the frequency and proportional morbidity of injury and illness categories were reported for September 25--October 15 for all six parishes. Proportion estimates for each illness and injury category were calculated by dividing the number of persons with a specific condition by all persons who reported an illness or injury, respectively. Analyses were stratified by relief worker status, with persons identified as relief workers 1) if they were coded as a relief worker on the CRF, or 2) if they reported to specific facilities that primarily served relief workers. During September 25--October 15, a total of 17,446 CRFs were recorded, including 8,997 (51.6%) for illness; 4,579 (26.2%) for injury (Tables 1 and 2); and 3,870 (22.2%) for nonacute (e.g., medication refill and follow-up visits) or undetermined reasons. A total of 178 CRFs recorded both injury and illness (1.0%). For patients whose disposition status was known (n = 13,717), a total of 11,169 (81.4%) were discharged, 1,500 (10.9%) were admitted to a hospital, 537 (3.9%) left without medical advice or treatment, 486 (3.5%) were transferred to another facility, and 25 (0.2%) died. The most common reasons for hospital admission were heart disease (26.6%), nondiarrheal gastrointestinal illness (e.g., gastritis or other gastrointestinal condition not including gastroenteritis) (12.3%), mental health condition (6.7%), and heat-related illness (6.1%). Of the 25 deaths, 23 occurred in patients who were seen for an illness (92%), and two occurred in patients seen for an injury (8%). Of 13,576 visits for injuries and illnesses, 1,235 (9.1%) were reported among relief workers (e.g., paid military, paid civilian, self-employed, or volunteer), and 5,437 (40.1%) were among residents (i.e., those who were not relief workers). Relief worker status was unknown for 6,904 (50.9%) events. Among patients with a reported illness (n = 8,997), a higher proportion of acute respiratory events were observed among relief workers (25.5% versus 14.8%) than among residents. Among patients with a reported injury, residents had a higher proportion of falls (25.0% versus 12.0%) and motor-vehicle crashes (9.0% versus 3.8%) and a lower proportion of unintentional injuries (51.9% versus 62.7%), when compared with relief workers. Unintentional injuries included cuts, blunt trauma, burns, and environmental exposures. Reported by: C Lopez, East Jefferson General Hospital, T Bergeron, West Jefferson Medical Center, New Orleans; R Ratard, MD, S Straif-Bourgeois, PhD, T Sokol, MPH, Louisiana Dept of Health and Hospitals, Office of Public Health. C Rubin, DVM, S Young, MPH, Div of Environmental Hazards and Health Effects; J Mott, PhD, A Fleischauer, PhD, A Khan, MD, National Center for Infectious Diseases; S Sandhu, PhD, N Arboleda, MD, P Vranken, MBA, EIS officers, CDC. Editorial Note:Active surveillance for injuries and illnesses was rapidly implemented in hospital emergency departments (EDs), community clinics, and temporary acute-care facilities staffed by DMATs in response to Hurricane Katrina. Although resource intensive, operation of this paper-based active surveillance system was useful in providing timely patient-specific information on suspected illnesses, mechanisms of injury, and unmet needs of persons with chronic diseases or other conditions (e.g., medication refills). In addition to the paper-based active surveillance system, infection-control professionals conducted follow-up of cases and were the sole source of information during the evacuation period for Hurricane Rita. Information obtained through surveillance and communication with infection-control professionals aided epidemiologic investigations, provided timely and appropriate public health messages, and facilitated decisions in resource distribution (4). The system identified illness clusters (e.g., rash illness and acute respiratory infection) and increasing injury trends (e.g., motor-vehicle crashes) and disproved unconfirmed illness reports (3,5). For example, on September 30, surveillance staff completing CRFs through medical-record abstraction at a single participating ED recognized an increase in rash-illness visits among construction workers. A joint epidemiologic investigation by CDC and the U.S. Army was performed to determine illness etiology, along with the help of infection-control professionals. A cohort of 100 construction workers residing in close quarters in a temporary camp on a U.S. military installation were interviewed for sources of exposure, and environmental samples were collected. Preliminary results indicated multiple etiologies, including arthropod bites and exposure to fiberglass. Compared with the immediate post-Hurricane Katrina surveillance period (September 8--25, 2005), the proportion of illness and injury events during this post-Hurricane Rita reporting period (September 25--October 15, 2005) was similar (3). However, the distribution of specific illness categories changed, with a lower proportion of skin or wound infections (9.8% versus 15.4%) and heat-related illnesses (2.6% versus 5.0%) during the post-Hurricane Rita and repopulation periods, compared with the immediate post-Hurricane Katrina period (3). Nonetheless, any changes in proportional morbidity of a specific condition might reflect actual changes or possibly a consequence of change in another condition (e.g., an increase in unintentional injuries). The findings in this report are subject to at least four limitations. First, illnesses and injuries might have been misclassified, particularly certain conditions (e.g., chest pain) that could be classified under multiple diagnostic categories (6). Second, information regarding denominator data (i.e., target population at risk) was limited. Thus, calculating rates for illnesses and injuries was not feasible. Third, because a true baseline was not available for comparison, determining whether observed data reflected actual increases was difficult. Finally, data were incomplete, especially for variables such as residency status, and thus might have introduced bias into these analyses. The public health response to this major disaster involved the implementation of a paper-based active surveillance system in hospital EDs and acute-care facilities. However, because of the burden imposed on health-care workers and capacity required by public health staff to maintain this system, an ED-based electronic syndromic surveillance system was implemented on October 17, 2005. Six participating EDs in the New Orleans area consented to transmit ED data electronically (e.g., patient demographics and chief complaint) every 24 hours to LDHH, where data were analyzed using the Early Aberration Reporting System (EARS) (7). These six hospitals were representative of the community, including public, private, and children's hospitals, whereas the two hospitals not participating were outside of the city and were smaller facilities. Although electronically reported data commonly used in syndromic surveillance are limited and nonspecific (i.e., chief complaint versus detailed clinical and etiologic questions on a CRF), electronic ED-based syndromic surveillance is a more sustainable method to continue long-term surveillance for injury and illness after the initial response phase of a major disaster. Acknowledgments This report is based, in part, on contributions by K Stephens, MD, City of New Orleans Health Department; emergency department staff and infection-control practitioners at Northshore Regional Medical Center, Ochsner Hospital, St. Charles Parish Hospital, East Jefferson Medical Center, West Jefferson Medical Center, Touro Hospital, Tulane Lakeside Hospital, Kenner Hospital, and other acute-care facilities, New Orleans, Louisiana; and the Greater New Orleans Public Health Support Team, CDC. References
Table1 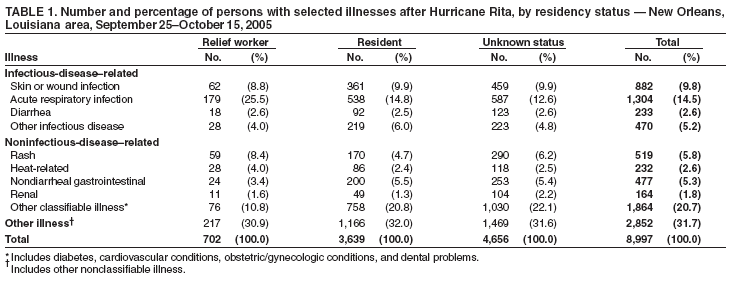 Return to top. Table2 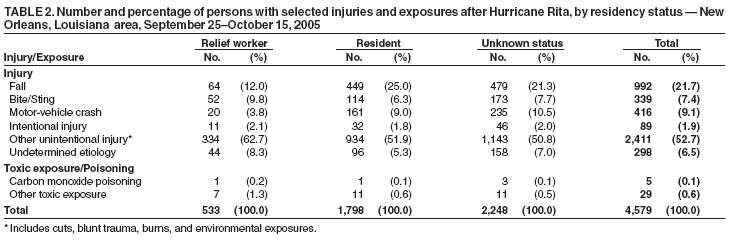 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 1/19/2006 |
|||||||||
|