 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Assessment of Local Health Department Smoking Policies --- North Carolina, July--August 2003Secondhand smoke is a cause of disease in healthy nonsmokers (1--6), and an increasing number of states have adopted laws prohibiting smoking in private-sector worksites, restaurants, and bars (7). However, certain state governments have provisions in their state smoking restrictions that preempt more stringent local laws (8). North Carolina has such a preemptive state smoking law,* passed in 1993, which mandates that 20% of the space within state-controlled buildings be designated as smoking areas. Exemptions from the law included local health departments (LHDs), providing an opportunity for public health practitioners to enact more stringent policies. To assess smoking policy gains from this exemption, a research team from the University of North Carolina at Chapel Hill (UNC) surveyed LHD directors. Results of the survey indicated uncertainty regarding the state law, with 37% of LHD directors believing they were prohibited from enacting a 100% tobacco-free policy on LHD grounds† and 20% not knowing whether they were prohibited. The North Carolina Association of Local Health Directors used these findings to work with legislators in the North Carolina General Assembly to amend the state smoking law in 2005, specifying that the exemption applies to both LHD buildings and grounds. North Carolina has 85 county or multicounty LHD directors, representing all 100 counties in the state. Of the 85 directors, a total of 76 (89.4%) agreed to participate in the study. During July--August 2003, the LHD directors responded to a telephone survey that included questions related to their knowledge and opinions regarding 1) the effects of exposure to secondhand smoke; 2) state legislation on smoking in public spaces; 3) tobacco-use policies, enforcement provisions, and availability of smoking-cessation support services at their LHDs; and 4) perceived LHD employee support for a 100% tobacco-free policy. LHD directors also were asked whether smoking was permitted in 13 traditional smoking sites§ in the buildings or on the grounds of their LHDs. To assess the accuracy of such self-reported data on tobacco-use policies, 15 written policies were obtained at random from the LHDs and compared with the responses of their 15 respective directors. The responses were determined to be 86% in agreement with the written policies. The survey received approval by the Biomedical Institutional Review Board of the UNC School of Medicine. Among the 76 county or multicounty LHDs represented, the median number of employees was 85 (range: 15--600), the average number of buildings occupied was 3.2, and the median number of patients or visitors annually was 20,000 (range: 3,000--400,000). Among the 76 LHD directors, 53 (69.7%) were nonsmokers, 20 (26.3%) were former smokers, and three (3.9%) were current smokers.¶ According to LHD director estimates, the mean percentage of current smokers among employees at the 76 LHDs was 10% (range: 1%--42%). Approximately 60% of LHD directors reported their departments did not routinely offer cessation services for employees who smoked. High percentages of LHD directors agreed or strongly agreed that exposure to secondhand smoke can trigger asthma attacks (98.7%), cause lung cancer (97.4%) and lead to adverse short-term cardiovascular effects (84.3%). Official, written tobacco-use policies were in effect at 89.5% of the LHDs, whereas 10.5% operated with unofficial tobacco-use policies. Among 75 of the 76 LHDs, 33 (44.0%) had tobacco-use policies specific to the LHD, 33 (44.0%) operated under countywide policies, four (5.3%) operated under both LHD and countywide policies, and five (6.7%) operated under the federal Pro-Children Act of 1994.** At 100% of the LHDs, smoking was prohibited in indoor hallways and corridors, waiting areas and lobbies, administrative and private offices, clinics and doctors' offices, cafeterias, locker rooms, and restrooms. One LHD reported having a 100% tobacco-free policy. However, among those LHD directors who answered the questions, 38 of 66 (57.6%) said smoking was permitted at LHD events and functions, 29 of 39 (74.4%) said smoking was permitted on outdoor walkways and loading docks, 60 of 76 (78.9%) said smoking was permitted outside all entrances and exits, and 74 of 76 (97.4%) said smoking was permitted in parking lots (Figure). Among the LHD directors, 57 of 75 (76.0%) said they were very familiar or somewhat familiar with the preemptive provisions of North Carolina's state law on smoking in public places (9). However, 28 of 75 (37.3%) incorrectly believed the law prevented enactment and enforcement of a 100% tobacco-free policy on LHD grounds, and 15 (20.0%) said they did not know whether the law prohibited such a policy. Sixty-six of the 76 LHD directors (86.8%) believed the majority of their employees would support a 100% tobacco-free policy at their LHDs. Fifty-eight (76.3%) reported that no single person was officially responsible for enforcing their tobacco-use policy. In May 2005, the North Carolina General Assembly, in response to data indicating uncertainty about exemptions and with leadership from the North Carolina Association of Local Health Directors, amended the section of the state's smoking law, enabling LHDs to implement more stringent policies. The new law specifies that the exemption applies to both LHD buildings and grounds, including areas within 50 feet of a building.†† Reported by: AO Goldstein, MD, C Gray, MPH, AY Butzen, KM Ribisl, PhD, Dept of Family Medicine, School of Public Health, Univ of North Carolina at Chapel Hill. Editorial Note:The findings described in this report indicate uncertainty among the majority of LHD directors in North Carolina regarding whether the state's 1993 smoking law prevented them from implementing a tobacco-free policy. The North Carolina Tobacco Control Program works to implement a comprehensive tobacco prevention and control program, of which smoke-free policies are a substantial component. Achieving tobacco-free policies in North Carolina LHDs will require leadership from LHD directors, policy approval from local boards of health, and support from LHD employees. Given that 86.8% of LHD directors reported that their employees would support 100% tobacco-free policies and given the known health benefits of such policies, policy gains might be possible. Implementation of such policies can reduce smoking and encourage cessation among LHD employees while protecting employees, patients, and visitors from exposure to secondhand smoke. The findings in this report are subject to at least three limitations. First, the survey consisted of self-reported data and opinions of LHD directors regarding smoking policies; LHD directors might overestimate or underestimate the percentage of employees who smoke or employee support for tobacco-free policies. Second, although opinions of LHD directors are influential, LHD policies also are influenced by opinions from local boards of health, which might differ from those of directors. Finally, these data represent LHDs only in North Carolina. Other states already have tobacco-free policies in place at LHDs; however, such policies are not tracked. If LHDs establish 100% tobacco-free policies, they will need to ensure enforcement. In the study described in this report, most directors reported that no single person was officially responsible for enforcement; new policies should include language and mechanisms to ensure prohibition of tobacco use in difficult-to-monitor locations such as in LHD vehicles, outside entrances, on loading docks, and at LHD events and functions. LHD employees who smoke also should be provided access to cessation-support services, which can substantially improve their odds of quitting smoking (9). In this study, LHD directors indicated their awareness of the adverse health effects of secondhand smoke. By implementing tobacco-free policies, they also can acknowledge the important role that LHD policies can play in modeling healthy behavior to the public and changes in social norms regarding the acceptability of smoking. References
* North Carolina General Statutes 143-595 to 143-601. Article 64. Smoking in public places (1993). Available at http://www.ncga.state.nc.us/sessions/1993/bills/house/html/h957v5.html. † Defined as prohibiting the use of all tobacco products by anyone, at any time, at any place on LHD grounds, in LHD vehicles, or at LHD events or functions. § Indoor hallways and corridors; outdoor walkways and loading docks; waiting areas and lobbies; administrative and private offices; clinics and doctors' offices; cafeterias; break rooms and lounges; locker rooms; restrooms; LHD events and functions; outside entrances and exits; parking lots and structures; and LHD vehicles. ¶ Current smoker was defined as a person who uses pipes, cigars, or cigarettes. Nonsmoker was defined as a person who never uses pipes, cigars, or cigarettes. Former smoker was defined as a person who has used pipes, cigars, or cigarettes but not currently. ** Pro-Children Act of 1994. Pub. L. 103-227. 20 USC 6081-6084 (March 31, 1994). †† North Carolina General Statute 143-599. An act to exempt from the law governing smoking restrictions local health departments and the buildings and grounds where they are located (2005). Available at http://www.ncga.state.nc.us/sessions/2005/bills/house/html/h239v4.html.
Figure 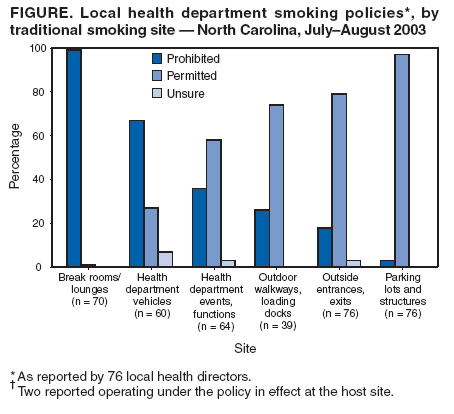 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 7/6/2005 |
|||||||||
|