 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. State Smoking Restrictions for Private-Sector Worksites, Restaurants, and Bars --- United States, 1998 and 2004Secondhand smoke is a known carcinogen (1). Exposure to secondhand smoke causes approximately 35,000 heart disease deaths and 3,000 lung cancer deaths among nonsmokers in the United States every year (2). Implementing policies that establish smoke-free environments is the most effective approach to reducing secondhand smoke exposure among nonsmokers (1). Smoking restrictions and smoke-free policies can take the form of laws or regulations implemented at the state or local level or of voluntary policies implemented by private employers and businesses. Smoking restrictions limit smoking to certain areas within a venue; smoke-free policies ban smoking within the entire venue. One of the national health objectives for 2010 is to establish laws in all 50 states and the District of Columbia (DC) that prohibit or restrict smoking in public places and worksites. A related objective calls for all worksites to voluntarily implement policies that prohibit or restrict smoking. To assess progress toward meeting the first objective, CDC reviewed the status of state laws restricting smoking as of December 31, 2004, updating a 1999 study that reported on such laws as of December 31, 1998 (3). This report summarizes the changes in state smoking restrictions for private-sector worksites, restaurants, and bars that occurred during 1999--2004.The findings indicate an increase in the number and restrictiveness of state laws regulating smoking in private-sector worksites, restaurants, and bars from 1999 through 2004. At the end of 2004, however, 16 states still had no restrictions on smoking in any of the three settings considered. Although secondhand smoke exposure among U.S. nonsmokers has decreased sharply in recent years, a substantial portion of nonsmokers continue to be exposed to secondhand smoke (4). The smoking restrictions in effect in each of the 50 states and DC* as of December 31, 1998, and December 31, 2004, were categorized into one of four levels for each of the three settings included in this study (Table). These settings were selected because worksites are a major source of secondhand smoke exposure for adult nonsmokers (1), and because workers in restaurants and bars are exposed to especially high levels of secondhand smoke (5). The four levels are as follows: 1) no restrictions, 2) designated smoking areas required or allowed, 3) no smoking allowed or designated smoking areas allowed if separately ventilated, and 4) no smoking allowed (i.e., 100% smoke-free). (These levels apply only to indoor areas of these settings.) These data were collected from CDC's State Tobacco Activities Tracking and Evaluation (STATE) System database, which contains tobacco-related epidemiologic and economic data and information on state tobacco-related legislation (6). The data used for this report are collected quarterly from an online database of state laws, analyzed by using a coding scheme and decision rules, and transferred into the STATE System database. The STATE System tracks state smoking restrictions in government worksites, private-sector worksites, restaurants, commercial and home-based child care centers, and other settings, including bars, shopping malls, grocery stores, enclosed arenas, public transportation, hospitals, prisons, and hotels and motels. Tobacco-control personnel in state health departments reviewed and commented on the coding of smoking restrictions in their states. Laws enacted before December 31, 2004, but not effective until after that date are not reflected in this report. For example, Rhode Island enacted comprehensive smoke-free indoor air legislation in 2004 that did not take effect until 2005 and was therefore not included in this assessment. The report also does not reflect legislation enacted since the end of 2004. For example, during January 1--June 30, 2005, Georgia, Maine, Montana, North Dakota, Rhode Island, and Vermont enacted smoking restrictions. During December 31, 1998--December 31, 2004, 10 states indicated changes in the level of their smoking restrictions for private-sector worksites, nine states indicated changes in the level of their smoking restrictions for restaurants, and five states indicated changes in the level of their smoking restrictions for bars, on the basis of the STATE System coding scheme. In every case, the restrictions became more stringent. As of December 31, 1998, only one state (Maryland) banned smoking in private-sector worksites. As of December 31, 2004, six additional states (Delaware, Florida, Idaho, Massachusetts, New York, and South Dakota) had done so. In 1998, one state (California) required that private-sector worksites restrict smoking to separately ventilated employee break rooms. In 2004, two additional states (Connecticut and Oregon) had enacted smoking restrictions of this type. In 1998, 20 states required or allowed designated smoking areas in worksites. In 2004, 18 states had laws of this type in place, with two states moving from no smoking restrictions into this category and four states moving from this category into one of the more restrictive categories. In 1998, a total of 29 states had no smoking restrictions in place for private-sector worksites. In 2004, this number had decreased to 23 states. In 1998, two states (Utah and Vermont) banned smoking in restaurants. During 1999--2004, six additional states (Delaware, Florida, Idaho, Maine, Massachusetts, and New York) did so. In 1998, one state (California) required that restaurants restrict smoking to separately ventilated employee break rooms. In 2004, one additional state (Connecticut) had enacted a smoking restriction of this type. In 1998, 27 states required or allowed designated smoking areas in restaurants; in 2004, 22 states had smoking restrictions of this type in place, with two states moving from no restrictions into this category and seven states moving from this category into one of the more restrictive categories. In 1998, 21 states had no smoking restrictions for restaurants. In 2004, this number had decreased to 19 states. In 1998, no states required bars to be smoke-free. During 1999--2004, four states (Delaware, Maine, Massachusetts, and New York) enacted laws that banned smoking in bars. In 1998, one state (California) required that bars restrict smoking to separately ventilated employee break rooms. In 2004, one additional state (Connecticut) had enacted a smoking restriction of this type. In 1998, two states required or allowed designated smoking areas in bars; this remained the case in 2004. In 1998, a total of 48 states had no smoking restrictions for bars. In 2004, this number had decreased to 43 states. In 2004, three states (Delaware, Massachusetts, and New York) banned smoking in all three settings considered in this study, compared with no states in 1998. At the end of 2004, 16 states had no smoking restrictions in place in any of these three settings, compared with 19 states in 1998. Many other states had no restrictions, or restrictions that did not provide full protection, in some of these settings. Reported by: J Chriqui, PhD, J O'Connor, JD, MayaTech Corporation, Silver Spring, Maryland. S Babb, MPH, NA Blair, MPH, G Vaughn, A MacNeil, MPH, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings of this analysis indicate that the number and restrictiveness of state laws regulating smoking in private-sector worksites, restaurants, and bars increased from 1999 to 2004. This increase has provided U.S. nonsmokers with greater protection from exposure to secondhand smoke (1,4,10). As of 1998--1999, 69.3% of U.S. workers reported that their workplace had an official policy that prohibited smoking in work areas and public or common areas, compared with 46.5% in 1993 (7). However, despite recent progress, many workers are still not protected by smoke-free workplace policies. Moreover, the proportion of workers covered by such policies during 1998--1999 varied by occupation, from 42.9% among food-preparation and food-service workers to 90.8% of primary-school teachers (7). The proportion of waiters (27.7%) and bartenders (12.9%) who reported being covered by smoke-free policies was lower than the proportion of food-preparation and -service workers overall (7). A previous study has indicated that food-service workers have a 50% greater risk for developing lung cancer than the general population, resulting in part from their higher level of occupational exposure to secondhand smoke (8). As a result of continuing gaps in policy coverage for many private-sector worksites, restaurants, and bars, a substantial portion of the U.S. nonsmoking population remains at risk for exposure to a known carcinogen in these settings, either as employees or customers. In addition to protecting both workers and patrons from secondhand smoke exposure, smoke-free workplace policies also are associated with decreased cigarette consumption and possibly with increased cessation rates among workers and members of the general public (1). Peer-reviewed studies relying on objective indicators such as sales tax revenue and employment levels have consistently found that smoking restrictions do not have a negative economic impact on restaurants and bars (9). Studies have also reported high levels of public support for and compliance with these laws (1,10). The findings in this report are subject to at least four limitations. First, the STATE System only captures certain types of state smoking restrictions (primarily statutory laws and executive orders) and does not capture state administrative laws, such as regulations, or implementation guidelines. As a result, the manner in which a state smoking restriction is implemented in practice might differ from how it is coded in the STATE System. For example, this report does not reflect a regulation in the state of Washington that restricts smoking in private-sector worksites and an administrative rule in Utah that imposes restrictions on smoking in certain bars. The STATE System also does not capture the extent to which state smoking restrictions are actually enforced. Second, some state smoking restrictions apply only to private-sector worksites with more than a certain number of employees, to restaurants with more than a specified number of seats, or to bars of at least a certain size. In these cases, the state laws are coded according to the level of these restrictions, even though these restrictions do not apply to venues below the relevant size limit.† Third, because the STATE System only collects state-level data, it does not reflect local smoking restrictions that are in place in many states. Some states with no or minimal state smoking restrictions have strong local smoking restrictions in place in many communities (1). State legislative provisions that do not preempt communities from enacting more stringent local laws allow continued passage and enforcement of local smoking restrictions that can establish a greater level of protection of public health (3). Finally, this report does not address sources of secondhand smoke exposure other than private-sector worksites, restaurants, and bars. Homes are another important source of exposure, especially for children (1), who on average are exposed to higher levels of secondhand smoke than adults (4). The importance of smoke-free indoor air laws and policies as a component of comprehensive tobacco-control interventions is reflected by their inclusion in national health objectives for 2010 and in CDC surveillance (1). Although population-based data indicate declining secondhand smoke exposure in the workplace over time, this exposure remains a common public health hazard that is entirely preventable (1). Optimal protection of nonsmokers and smokers requires a smoke-free environment (1). Acknowledgments The findings in this report are based, in part, on contributions by L Lineberger, MayaTech Corporation, Silver Spring, Maryland. D Coleman, MPH, Northrop Grumman, Atlanta, Georgia. TF Pechacek, PhD, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. References
* For this report, DC is included among the states. † Information on worksite and restaurant size exemptions is available at http://www.cdc.gov/tobacco/statesystem. The STATE System does not track information on bar size exemptions.
Table 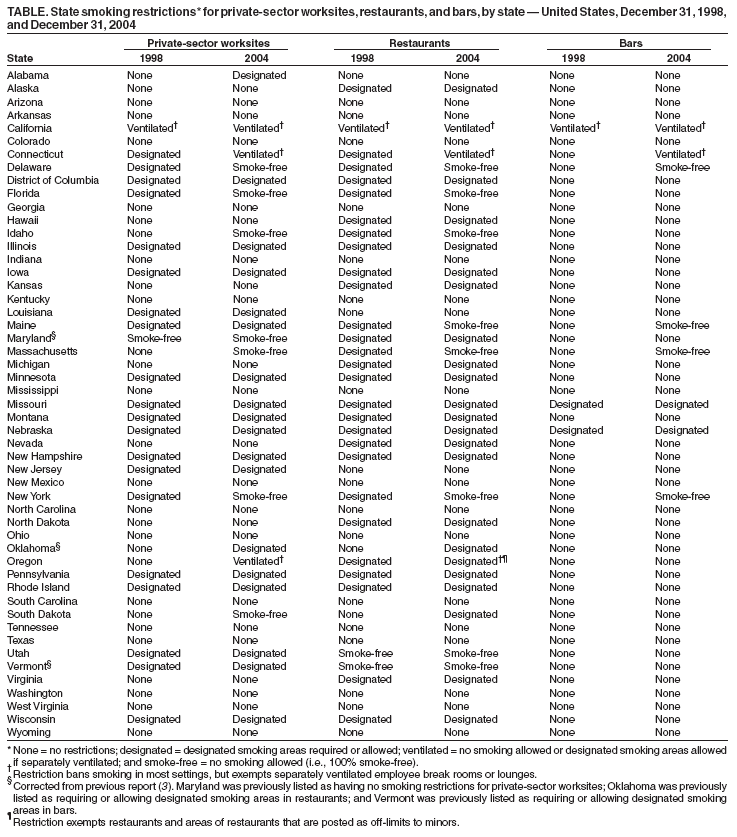 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 7/6/2005 |
|||||||||
|