 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Reducing Falls and Resulting Hip Fractures Among Older WomenPlease note: An erratum has been published for this article. To view the erratum, please click here. The material in this report was prepared for publication by: National Center for Injury Prevention
and Control Division of Unintentional Injuries Prevention Reducing Falls and Resulting Hip Fractures Among Older WomenJudy A. Stevens, Ph.D. Abstract Scope of the Problem: Fall-related injuries are the leading cause of injury deaths and disabilities among older adults (i.e., persons aged >65 years). The most serious fall injury is hip fracture; one half of all older adults hospitalized for hip fracture never regain their former level of function. In 1996, a total of 340,000 hospitalizations for hip fracture occurred among persons aged >65 years, and 80% of these admissions occurred among women. From 1988 to 1996, hip fracture hospitalization rates for women aged >65 years increased 23%. Etiologic or Risk Factors: Risk factors for falls include increasing age, muscle weakness, functional limitations, environmental hazards, use of psychoactive medications, and a history of falls. Age is also a risk factor for hip fracture. Women aged >85 years are nearly eight times more likely than women aged 65-74 years to be hospitalized for hip fracture. White women aged >65 years are at higher risk for hip fracture than black women. Other risk factors for hip fracture include lack of physical activity, osteoporosis, low body mass index, and a previous hip fracture. Recommendations for Prevention: Because approximately 95% of hip fractures result from falls, minimizing fall risk is a practical approach to reducing these serious injuries. Research demonstrates that effective fall prevention strategies require a multifaceted approach with both behavioral and environmental components. Important elements include education and skill building to increase knowledge about fall risk factors, exercise to improve strength and balance, home modifications to reduce fall hazards, and medication assessment to minimize side effects (e.g., dizziness and grogginess). Program and Research Needs: Coordination needs to be improved among the diverse Federal, state, and local organizations that conduct fall prevention activities. The effectiveness of existing fall prevention programs among specific groups of women (e.g., those aged >85 years or living with functional limitations) needs careful evaluation. New primary fall prevention approaches are needed (e.g., characterizing footwear that promotes stability), as well as secondary prevention strategies (e.g., protective hip pads) that can prevent injuries when falls occur. Finally, efforts are needed to increase collaboration among national experts from various disciplines, to reach consensus regarding priority research areas and program issues, and to work toward long-term strategies for reducing falls and fall-related injuries among older adults. Conclusion: Persons aged >65 years constitute the fastest-growing segment of the U.S. population. Without effective intervention strategies, the number of hip fractures will increase as the U.S. population ages. Fall prevention programs have reduced falls and fall-related injuries among high-risk populations using multifaceted approaches that include education, exercise, environmental modifications, and medication review. These programs need to be evaluated among older adults aged >65 years who are living independently in the community. In addition, secondary prevention strategies are needed to prevent hip fractures when falls occur. Effective public health strategies need to be implemented to promote behavioral changes, improve current interventions, and develop new fall prevention strategies to reduce future morbidity and mortality associated with hip fractures among older adults. BACKGROUNDOlder adults (i.e., persons aged >65 years) are the fastest-growing segment of the U.S. population. In 1990, 13% of the population was aged >65 years; by 2050, this proportion will nearly double to 23% (1). The number of persons aged >65 years is projected to increase from 31.0 million in 1990 to 68.1 million by 2040; for persons aged >85 years, the relative growth is even faster (1). This report summarizes current knowledge about falls and hip fracture among women aged >65 years and describes both primary and secondary strategies for preventing fall-related injuries. When discussing research results, the term "significant" refers to a documented p-value of p < 0.05. SCOPE OF THE PROBLEMFalls are the leading cause of injury deaths and disabilities among persons aged >65 years. In the United States, one of every three older adults falls each year (2,3). In 1997, nearly 9,000 persons aged >65 years died from falls (4). Of those who fall, 20%-30% sustain moderate to severe injuries that reduce mobility and independence and increase the risk for premature death (5). Older adults are hospitalized for fall-related injuries five times more often than they are for injuries from other causes (5), and women are nearly three times more likely than men to be hospitalized for a fall-related injury (5). The most prevalent fall-related injuries among older adults are fractures of the hip; spine; upper arm; forearm; and bones of the pelvis, hand, and ankle (6). Of these, the most serious injury is hip fracture, a leading cause of morbidity and excess mortality among older adults (7). During 1988-1996, the estimated number of hospital admissions for hip fracture increased from 230,000 to 340,000 (Figure 1). In 1996, 80% of the admissions for hip fracture occurred among women (8). The rate of hospitalization for hip fracture differs by sex. The hip fracture hospitalization rate for persons aged >65 years is significantly higher for women than men (9). During 1988-1996, the rates for women increased significantly, from 972 per 100,000 to 1,356; for men, rates remained stable (9). A Healthy People 2010 objective is to reduce the hip fracture hospitalization rate among women aged >65 years to no more than 879 per 100,000 (objective 15-28a). Hip fracture hospitalization rates are substantially higher for white women than black women. In 1996, the hospitalization rate for white women aged >65 years was 1,174 per 100,000, five times the rate for black women (9). A Healthy People 2010 objective is to reduce hip fracture hospitalization rates among white women aged >65 years to no more than 932 per 100,000 (objective 15-28a). The overall increase in hip fracture hospitalization rates can be explained in part by the increasing U.S. population of very old adults (i.e., persons aged >85 years). Today, a larger proportion of the population is living to age >85 years than in the past because of reduced mortality from cardiovascular and other chronic diseases. Since 1987, death rates from coronary heart disease, stroke, and cancer have declined, and the proportion of adults aged >70 years living with some functional limitation* has increased (10). Frail older adults are twice as likely to fall as healthier persons (11). Hip fractures are expensive. A recent study documented that the cost of a hip fracture (including direct medical care, formal nonmedical care, and informal care provided by family and friends) was $16,300-$18,700 during the first year following the injury (12). In 1991, hip fracture accounted for an estimated $2.9 billion in Medicare costs (13). On the basis of the annual cost of hip fracture in 1984, an assumption that the average cost will remain constant, an inflation rate of 3%-5%, and the increasing number of hip fractures, the estimated total annual cost of hip fracture in the United States could reach $82-$240 billion by the year 2040 (14). An even more important factor than the monetary cost of hip fracture is the injury's impact on a person's life in the form of loss of independence and decreased quality of life. Nationwide, only 50% of older adults hospitalized for hip fracture are able to return home or live independently after the injury (15,16). ETIOLOGIC OR RISK FACTORSApproximately 95% of hip fractures are caused by falls (17). Other causes include being knocked over and being injured in a motor-vehicle crash; <2% of hip fractures occur spontaneously (e.g., as the result of a metabolic bone disease) (17). Not all falls are equally likely to cause hip fracture. Biomechanical studies have demonstrated that, although both bone strength and the force of the impact are important factors, the point of impact must be on or near the hip for a fall to cause a hip fracture (18). Many factors contribute to falls and subsequent fall injury. Fall risk increases rapidly with advancing age for persons aged >65 years (19). Other fall risk factors include lack of current or previous physical activity (20,21), muscle weakness or balance problems that can contribute both to the risk for falling and the inability to break the impact of a fall (2,22,23), functional limitations (e.g., difficulty with activities of daily living such as dressing or bathing) (22,24), cognitive impairment or dementia (2), use of psychoactive medications (e.g., tranquilizers or antidepressants), some combinations of medications (2,25), environmental factors (e.g., tripping hazards) (26), having fallen previously (27), having more than one chronic disease (28), having had a stroke (28), Parkinson disease (29) or a neuromuscular disease (30), urinary incontinence (31), and visual difficulties (32,33). Less clear is the fall risk associated with wearing shoes with thick, soft soles (e.g., jogging shoes) that can affect balance and proprioception or become a tripping hazard by catching in carpeting (34). Similar to fall risk, hip fracture risk increases sharply with advancing age (19). Women aged >85 years are nearly eight times more likely than women aged 65-74 years to be hospitalized for hip fracture (9). White women aged >65 years are at higher risk for hip fracture (19) than black women, in part because the prevalence and severity of osteoporosis -- a condition that predisposes to bone fragility -- is greatest among white women. Other risk factors include low body mass index (weight in kilograms divided by height in meters squared [weight [kg]/height squared [m2]) (7,35,36), previous history of osteoporosis (27), and having sustained a previous hip fracture (27). Falls are caused by personal (intrinsic) and environmental (extrinsic) factors. Personal risk factors include problems with gait and balance, functional impairments or limitations in activities of daily living, visual problems, and behavioral risk factors (e.g., lack of physical activity and taking certain psychoactive medications such as tranquillizers or antidepressants). Environmental factors include home hazards (e.g., clutter; no stair railings; loose rugs or other tripping hazards; no grab bars in the bathroom; and poor lighting, especially on stairs). Frequently, a fall is the result of an interaction between personal and environmental factors. RECOMMENDATIONS FOR PREVENTIONBecause approximately 95% of hip fractures result from falls (17), minimizing fall risk is a practical approach to reducing these serious injuries. Primary prevention of fall-related injuries involves reducing the occurrence of falls; secondary prevention of fall-related injuries involves preventing injuries when falls occur. Primary PreventionPrimary prevention of fall-related injuries among older adults can be targeted to persons living independently in the community or residents of nursing homes. Research has established that effective fall intervention programs employ a multifaceted approach and incorporate both behavioral and environmental elements: exercises to improve strength and balance, environmental modifications, education about fall prevention, medication review and assessment to minimize side effects, and risk factor reduction (36-39). Community InterventionApproximately 90% of adults aged >65 years live in the community and many fall prevention programs target these persons; however, few of these programs have been evaluated for effectiveness. During 1990-1992, a prospective, multifaceted, fall- prevention study was conducted among 301 community-dwelling men and women who were aged >70 years and had at least one fall risk factor (e.g., sedative use or some limitation in arm or leg strength) (36). A total of 153 persons participated in an intervention that consisted of behavioral instructions and training to reduce specific risk factors (e.g., persons with gait or balance impairments received specialized training in these areas), exercise programs to increase strength, and medication adjustments. After 1 year, the group that received the intervention had 30% fewer falls than the control group. Further research is needed to evaluate the effectiveness of such a program among all persons aged >65 years living independently in the community. Physical Activity. Increasing physical activity can be an effective component of fall prevention programs. Activities that improve strength, balance, and coordination can reduce the risk for falls and fall-related injuries among healthy (40,41) and frail persons (42). Studies have demonstrated a 40%-60% reduction in hip fracture risk with increasing levels of physical activity (36,43). Although fall prevention programs have focused on several techniques to improve strength, balance, coordination, mobility, and flexibility, Tai Chi is probably the most frequently studied type of exercise (40). Effective programs have been employed with persons of different ages and with varied physical abilities; however, persons with functional limitations might require more individualized physical activity programs (44). Environmental Modifications. Because approximately 50%-60% of all falls among older adults occur at home, fall prevention programs should address home hazards that can contribute to falls (45). Home-visiting programs (e.g., those using visiting nurses) provide opportunities to identify potential fall hazards and take corrective action. These programs can increase awareness of fall risks among informal caregivers, (e.g., family and friends who frequently visit the homes of older adults) and the older adults themselves. Health Education. Fall prevention programs frequently include health education and health promotion materials about reducing fall hazards that are distributed at central locations (e.g., senior centers or health fairs). However, educational materials alone might not promote behavioral changes. Many programs employ home-hazard checklists that can be used by the caregiver or health agency personnel (e.g., a visiting nurse or home health aide) to help persons identify fall hazards and to suggest corrective action (e.g., eliminating potential tripping hazards such as clutter and throw rugs, adding stair railings, improving lighting, adding nonslip floor surfaces, and installing grab bars in bathrooms). Checklists are also given to residents to help them assess personal and environmental risks and take preventive action, including behavioral changes (45). Research is needed to evaluate and assess the effectiveness of educational materials and home-hazard checklists to promote fall-risk reduction activities and behaviors. Risk Factor Reduction. Approaches that address specific risk factors can supplement fall prevention program efforts. Medical approaches might include reducing fall risk factors (e.g., maximizing control of concomitant chronic diseases) and reducing hip fracture risk factors (e.g., counseling women aged >65 years against inappropriate weight loss). Nursing-Home InterventionNursing-home residents, who constitute approximately 5% of the population aged >65 years, are at particularly high risk for fall-related injuries. Approximately one half of the estimated 1.7 million nursing-home residents in the United States fall at least once each year, and 11% sustain a serious fall-related injury (46). A randomized trial of seven pairs of nursing homes that included 500 residents evaluated an intensive, multifaceted intervention of extensive environmental modifications (e.g., obtaining wheel locks for beds, changing lighting, modifying floor plans, and purchasing raised toilet seats), medication review, and increased attention to individual resident needs (39). Repeat falls declined 19% among nursing-home residents who had fallen at least once during the previous year. However, approximately one third of the safety recommendations implemented in the study group were discontinued within 3 months of the completion of the study. Strategies are needed to institutionalize fall prevention interventions in the nursing-home setting, and additional programs designed for high-risk nursing-home residents need to be implemented and evaluated. Secondary PreventionSecondary prevention strategies are being developed to reduce the incidence of hip fracture among older women (47). Most hip fractures are caused by falling directly on the hip, and biomechanical studies have demonstrated that a pad that shunts the energy away from the point of impact is highly effective in reducing the force of a fall on the proximal femur (48). A 1993 clinical study in a Copenhagen nursing home demonstrated that hip protectors reduced the risk for hip fracture by approximately 50% (47). During 1994-1996, researchers in Finland conducted a study to determine whether nursing-home residents would wear an undergarment with energy-shunting hip pads. The findings indicated that 63% of the residents wore the pads (49). U.S. manufacturers have considered producing and marketing an undergarment with energy-absorbing hip pads, but how acceptable and effective this garment might be among community-dwelling older adults is unknown. A promising technologic innovation for preventing fall-related injuries is a recently developed safety floor (50). Under laboratory conditions, this flooring material provides a firm walking surface and, if a fall occurs, reduces the force of impact through the use of special energy-absorbing flooring material. Field trials are under way in nursing homes to evaluate the effectiveness of this material in preventing fall-related hip fractures among nursing-home residents. PROGRAM AND RESEARCH AGENDAMany professional and community-level organizations within the public health community, federal agencies, nongovernmental organizations, and state and local health departments are involved in efforts to reduce falls and fall-related injuries among older adults. However, coordination among these entities has been limited. CDC's National Center for Injury Prevention and Control has funded the National Resource Center on Aging and Injury at San Diego State University to collect, organize, and evaluate information and to increase awareness about preventing unintentional injuries among older adults. Information will be available through fact sheets, formal publications, and the Internet (at <http://www.olderadultinjury.org>) and will be provided to health-care professionals, caretakers, and other persons concerned about reducing injuries among older adults. Researchers do not know all the factors that contribute to falls and fall-related injuries or how personal and environmental factors interact to cause a fall. These factors have been difficult to identify because persons frequently cannot explain the causes or circumstances surrounding fall events. In one prospective study, one fourth to one third of the participants did not remember a fall that occurred 36 months earlier (51). Older adults might either blame themselves for falling or consider falls to be an inevitable consequence of the aging process. Longitudinal prospective studies are needed to accurately assess the associations between fall risk factors (e.g., interactions between intrinsic and extrinsic factors), the occurrence of falls, and fall outcomes (e.g., frequency of falls, whether an injury results, and level of injury severity). To decrease the incidence and severity of fall-related injuries, injury-prevention programs for older adults need to integrate research findings into multifaceted, community-level programs that include both implementation and evaluation components. A model program would employ a prospective design to accurately record fall occurrences and establish whether a fall resulted in an injury. Such a program should incorporate four critical elements: a) education and skill-building activities to increase knowledge about fall risk factors, b) exercise to increase strength and improve balance, c) home safety modifications and repairs to reduce fall hazards, and d) medication review to maximize control of comorbid conditions while reducing adverse side effects. Because persons must take an active role to reduce their risk for falling, a model fall prevention program should also include effective strategies to promote behavioral changes. Because of the increasing number of persons aged >65 years in the United States, the need is increasing to develop an effective national plan to address the problem of falls and fall-related injuries within the constraints of limited health-care resources. To accomplish this goal, efforts are needed to increase collaboration among national experts from various disciplines (e.g., gerontologists, health educators, behavioral epidemiologists, home designers, and ergonomic experts), to reach consensus regarding the priority research areas and program issues, and to work toward long-term strategies for reducing falls and fall-related injuries among older adults. Some subgroups of older adults (e.g., women aged >85 years and older adults with functional limitations) might have different fall-injury risks than most community- dwelling older adults (44). Efforts are needed to adapt existing fall prevention programs or develop new interventions to reduce falls in these groups. Finally, in addition to existing behavioral and environmental interventions, new fall prevention approaches (e.g., characterizing footwear that promotes stability and developing more effective home lighting) need to be developed. CONCLUSIONPersons aged >65 years constitute the fastest-growing segment of the U.S. population. The average life expectancy for both men and women is increasing, in part because of healthier life styles and better control and treatment of chronic conditions (e.g., cardiovascular disease). Without effective intervention strategies, the number of hip fractures will increase as the U.S. population ages. Fall prevention programs have effectively reduced falls in select populations by 30%-50%, using multifaceted approaches that include various combinations of education, exercise, medication assessment, risk factor reduction, and environmental modifications. Such programs need to be expanded to include multiple intervention components tailored for diverse populations of older adults and evaluated for effectiveness. In addition, secondary prevention strategies (e.g., reducing the amount of energy transferred to the hip) are needed to prevent hip fracture when falls occur. The problem of fall-related hip fractures will continue to increase unless effective intervention strategies are developed and implemented to improve fall prevention interventions and expand existing programs. Older adults must take an active role in reducing their risk for falling. Because most older adults live independently, fall prevention programs must include effective strategies to promote behavioral changes. Innovative and effective fall prevention strategies are needed to reduce future morbidity and mortality associated with hip fractures, increase independence, and improve quality of life for the growing number of older adults. References
*Defined as having difficulty with two or more activities of daily living. Figure 1 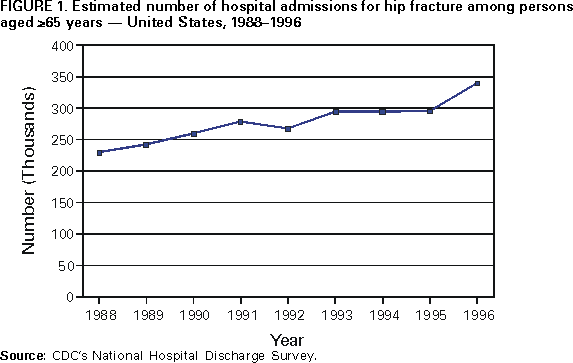 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 3/28/2000 |
|||||||||
This page last reviewed 5/2/01
|