 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Preventing Skin CancerFindings of the Task Force on Community Preventive Services on Reducing Exposure to Ultraviolet Light Prepared by SummaryRates of skin cancer, the most common cancer in the United States, are increasing. The most preventable risk factor for skin cancer is unprotected ultraviolet (UV) exposure. Seeking to identify effective approaches to reducing the incidence of skin cancer by improving individual and community efforts to reduce unprotected UV exposure, the Task Force on Community Preventive Services conducted systematic reviews of community interventions to reduce exposure to ultraviolet light and increase protective behaviors. The Task Force found sufficient evidence to recommend two interventions that are based on improvements in sun protective or "covering-up" behavior (wearing protective clothing including long-sleeved clothing or hats): educational and policy approaches in two settings---primary schools and recreational or tourism sites. They found insufficient evidence to determine the effectiveness of a range of other population-based interventions and recommended additional research in these areas: educational and policy approaches in child care centers, secondary schools and colleges, recreational or tourism sites for children, and workplaces; interventions conducted in health-care settings and targeted to both providers and children's parents or caregivers; media campaigns alone; and communitywide multicomponent interventions. This report also presents additional information regarding the recommended community interventions, briefly describes how the reviews were conducted, provides resources for further information, and provides information that can help in applying the interventions locally. The U.S. Preventive Services Task Force conducted a systematic review of counseling by primary care clinicians to prevent skin cancer (CDC. Counseling to prevent skin cancer: recommendation and rationale of the U.S. Preventive Services Task Force. MMWR 2003;52[No. RR-15]:13--17), which is also included in this issue, the first jointly released findings from the Task Force on Community Preventive Services and the U.S. Preventive Services Task Force. BackgroundIn the United States, the incidence and mortality from cutaneous malignant melanoma (CMM) have increased rapidly in the last few decades (1,2). In 2003, approximately 54,200 persons will have new diagnoses of melanoma, and 7,600 will die from the disease (3). The incidence of the other two skin cancers, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), is estimated to be >1 million new cases per year (3). According to the data from the Surveillance, Epidemiology and End Results (SEER) cancer registry of the National Cancer Institute, during 1995--1999, average annual age-adjusted incidence rates for melanoma per 100,000 population were 23.5 for men and 15.7 for women for non-Hispanic whites; 3.8 for men and 3.7 for women for Hispanics; 1.8 for men and 1.3 for women for Asians; 1.5 for men and 0.9 for American Indian/Alaska Natives; and 1.2 for men and 0.9 for women for non-Hispanic blacks (4). Well-established risk factors for skin cancer include family history of skin cancer, fair skin, red or blonde hair, propensity to burn, inability to tan, and preventable risk factors such as intermittent (for CMM and BCC) or cumulative exposure to ultraviolet (UV) radiation (for SCC) (5--8). Despite the adverse effects of unprotected UV exposure, approximately 32% of U.S. adults report having had a sunburn in the past year (9). Parents or caregivers reported that 72% of adolescents aged 11--18 years have had at least one sunburn (10), and 43% of white children aged <11 years experienced a sunburn in the past year (11). With respect to sun-protective behaviors, only one third of adults reported that they use sunscreen, seek shade, or wear protective clothing when out in the sun (12--13). Adolescents aged 11--18 years were found to routinely practice sun-protective behaviors slightly less than adults (using sunscreen [31%], seeking shade [22%], and wearing long pants [21%]) (14). Among children aged <11 years, sunscreen use (62%) and shade seeking (26.5%) were the most frequently reported sun-protective behaviors (15). The interventions reviewed in this article pertain to two objectives set in Healthy People 2010 (16):
By implementing interventions demonstrated to be effective in reducing exposure to UV light and increasing sun-protective behaviors, policy makers and public health providers can help their communities achieve these goals while using community resources efficiently. By producing additional research on other promising but as yet unproven interventions, researchers and communities can expand the portfolio of tested interventions. This report complements two reviews (17--18) and an updated Recommendation and Rationale statement (19) from the third U.S. Preventive Services Task Force (USPSTF) on the evidence for counseling and screening for skin cancer. This report and other related publications provide guidance from the Task Force on Community Preventive Services, an independent, nonfederal task force, to personnel in state and local health departments, education agencies, universities, community coalitions, organizations that fund public health programs, health-care systems, and others who have interest in or responsibility for reducing exposure to UV light and increasing protective behaviors for prevention of skin cancer. IntroductionThe Task Force on Community Preventive Services (the Task Force) is developing the Guide to Community Preventive Services (the Community Guide), a resource that will include multiple systematic reviews, each focusing on a preventive health topic. The Community Guide is being developed with the support of the U.S. Department of Health and Human Services (DHHS) in collaboration with public and private partners. Although CDC provides staff support to the Task Force for development of the Community Guide, the recommendations presented in this report were developed by the Task Force and are not necessarily the recommendations of DHHS or CDC. This report is one in a series of topics included in the Community Guide. It provides an overview of the process used by the Task Force to select and review evidence and summarize its recommendations regarding interventions to reduce UV exposure and increase UV protective behaviors for prevention of skin cancer. A full report on the recommendations, additional evidence (i.e., discussions of applicability, additional benefits, potential harms, existing barriers to implementation, costs, cost benefit, and cost effectiveness of the interventions [when available]), and remaining research questions will be published in the American Journal of Preventive Medicine. Community Guide topics are prepared and released as each is completed. The findings from systematic reviews on vaccine-preventable diseases, tobacco use prevention and reduction, motor vehicle occupant injury, physical activity, diabetes, oral health, and the effects of the social environment on health have already been published. A compilation of systematic reviews will be published in book form. Additional information regarding the Task Force and the Community Guide and a list of published articles are available on the Internet at http://www.thecommunityguide.org. MethodsThe methods used by the Community Guide for conducting systematic reviews and linking evidence to recommendations have been described elsewhere (20). In brief, for each Community Guide topic, a multidisciplinary team (the systematic review development team) conducts a review consisting of the following steps:
For each review of interventions regarding skin cancer prevention, the systematic review development team developed a conceptual model (or analytic framework) to show the relationship of the intervention to relevant intermediate outcomes (e.g., knowledge, attitudes and beliefs, and intentions regarding sun-protective behaviors), to implementing key sun-protective behaviors, and to the assumed relationships of improvements in sun-protective behaviors to skin cancer prevention. A representative example of an analytic framework for mass media interventions is illustrated (Figure). The analytic frameworks for the other interventions were similar to this example except that they included environmental and policy components. The analytic frameworks focused on key health outcomes (e.g., sunburn or nevi*) and sun-protective behaviors:
--- seeking shade, and
--- wearing a hat,
The team also examined intermediate outcomes that were postulated to be associated with sun-protective behaviors (e.g., knowledge, attitudes, and intentions). Recommendations were based either on better health outcomes (rare with this subject matter because relevant cancer outcomes would become apparent long after the time of the intervention) or risk behaviors that were thought to be established proxies for cancer outcomes (in this case, avoiding peak UV hours or covering up). The team considered sunscreen use to be a key secondary outcome of sun protection programs because sunscreens prevent sunburn (a marker of unprotected UV exposure and a health outcome associated with increased risk of skin cancer in epidemiologic studies) and reduce the incidence of SCC, and better alternatives are not always available (e.g., when swimming). Sunscreen's role in preventing skin cancer has been demonstrated to be complex, according to information in recent reports from national and international groups (18,21) and summarized in the last section of this report. Epidemiologic studies suggest that sunscreen use could be considered harmful if it increased a person's total time in the sun and total UV exposure. Partly for that reason, suncreen use alone might not protect against melanoma despite its protective effect on SCC. The International Agency for Research on Cancer (IARC) recommends that sunscreens not be used as the sole method for skin cancer prevention and not be used as a means to extend the duration of UV exposure (21). The team therefore did not consider sunscreen use, by itself, to be an established proxy for better health. The coordination team,† which conducted the systematic review, and their consultants§ generated a comprehensive list of interventions to reduce skin cancer. From this, a priority list of interventions for review was developed through a process of polling the coordination team, the consultants, and other specialists in the field regarding their perception of the public health importance (number of persons affected), the practicality of application, and the need of those promoting UV protective behaviors for information regarding each intervention. To conduct the review, the team organized interventions into three groups: setting-specific, target population-specific, and communitywide (Table). Setting was used as an organizing structure because it was a convenient proxy for key characteristics of the target populations and the implementers of the interventions. The majority of the interventions in this group involved diverse activities --- provision of information, environmental approaches (e.g., planting shade trees), or policy approaches (e.g., implementing a policy to reschedule outdoor activities or a requirement to wear hats when outside). Interventions in the setting-specific group consisted of educational and policy approaches in the following settings:
The target population of interest category included one intervention: children's parents or caregivers (some of these interventions might have already been examined in setting-specific groups). The category of communitywide interventions included two types of interventions and a subgroup:
Interventions reviewed were either single component (i.e., using only one activity to achieve desired outcomes) or multicomponent (i.e., using more than one activity, such as a policy or environmental intervention with a media campaign). Certain studies provided results relevant to more than one intervention and were included in each of the reviews to which they were applicable. Studies and outcome measures were classified according to definitions developed as part of the review process. The nomenclature used in this report sometimes differs from that used in the original studies. To be included in the reviews of effectiveness, studies had to 1) be primary investigations of interventions selected for evaluation rather than, for example, guidelines or reviews; 2) be published in English during the years 1966--2000; 3) be conducted in established market economies¶; and 4) compare outcomes among groups of persons exposed to the intervention with outcomes among groups of persons not exposed or less exposed to the intervention (i.e., the study design included a concurrent or before-and-after comparison.) Searches of three computerized databases (MEDLINE, PsychINFO, CINAHL)** were conducted. Team members also reviewed reference lists and consulted with other specialists in the field (e.g., participants in a skin cancer prevention listserv) to identify relevant studies. Each included study was evaluated by using a standardized abstraction form and was assessed for suitability of the study design and threats to validity (22). Studies were characterized as having good, fair, or limited execution based on the number of threats to validity (20). Results for each outcome of interest were obtained from each study that met the minimum quality criteria. Net effects were derived when appropriate by calculating the difference between the changes observed in the intervention and comparison groups relative to the respective baseline levels.†† The median was used to summarize a typical measure of effect across the body of evidence for each outcome of interest; both the median and the range are reported. For bodies of evidence consisting of four or more studies, an interquartile range was used to represent variability. The strength of the body of evidence of effectiveness was characterized as strong, sufficient, or insufficient on the basis of the number of available studies, the suitability of study designs for evaluating effectiveness, the quality of execution of the studies as defined by the Community Guide (20), the consistency of the results, and the effect size. The Task Force uses these systematic reviews to evaluate the evidence of intervention effectiveness and makes recommendations based on the findings of the reviews (20). The strength of each recommendation is based on the evidence of effectiveness (i.e., an intervention is recommended on the basis of either strong or sufficient evidence of effectiveness) (20). Other types of evidence can also affect a recommendation. For example, harms resulting from an intervention that outweigh benefits might lead to a recommendation that the intervention not be used even if it is effective in improving some outcomes. A finding of insufficient evidence to determine effectiveness should not be interpreted as evidence of ineffectiveness. Insufficient evidence may be found for any of a number of reasons, alone or in combination, including an insufficient number of studies; too many threats to the validity of the available studies based on their design, execution, or both; conflicts in the results of the studies that preclude a coherent summary of effectiveness; or no indication that the outcomes measured to date, by themselves, represent success in improving health. In all these situations, a finding of insufficient evidence to determine effectiveness is important for identifying areas of uncertainty and continuing research needs. In contrast, sufficient or strong evidence of ineffectiveness would lead to a recommendation against use of the intervention. ResultsDatabase searches and bibliographic reviews yielded a list of 6,373 potentially relevant titles. After review of the abstracts and consultation with specialists in the field, a total of 313 reports were retrieved. Of these, 154 were not used in the review because they did not provide results, did not refer to an intervention, or reported on noncomparative studies. The remaining 159 were retained for full review. On the basis of limitations in execution or design or because they provided only background information on studies that were already included, 74 of these were excluded and were not considered further. The remaining 85 studies were considered qualifying studies. The Task Force recommendations in this report are based on the systematic review and evaluation of these qualifying studies, all of which had good or fair quality of execution. The Task Force recommended two interventions, both in the setting-specific category (Table):
Interventions in primary school settings were designed to increase sun-protective knowledge, attitudes, intentions, and behavior among children from kindergarten through eighth grade. The interventions ranged from a curriculum that included interactive classroom and take-home activities to staff education, brochures for parents, and a working session to develop skin protection plans for schools. All interventions focused on some combination of increasing application of sunscreen, scheduling activities to avoid peak sun hours, increasing availability of shade and encouraging children to play in shady areas, and encouraging children to wear sun-protective clothing. Interventions in this category included at least one of the following activities:
Single- and multicomponent interventions in recreational settings were designed to increase knowledge; influence attitudes, beliefs, and intentions; and change behavior of adults and children. Interventions included one or more of the following: educational brochures, including culturally relevant materials and photographs of skin cancer lesions; sun-safety training for lifeguards, aquatic instructors, and outdoor recreation staff and role-modeling by these groups; sun-safety lessons, interactive activities, and incentives for parents and children; increasing available shaded areas; providing sunscreen; and point-of-purchase prompts. The recommended interventions had small to moderate behavior change scores. In primary schools, the median net relative increase was 25% (interquartile range: 1%--40%, six studies). In recreational settings, the median net relative increase was 11.2% (interquartile range: 5.1%--12.9%, five studies). It should be noted that the interventions were targeted to populations rather than single persons. Small changes in behavior in large populations can result in substantial public health benefits. The Task Force found insufficient evidence on which to make recommendations for or against the following interventions: educational and policy approaches in child care centers; educational and policy approaches in secondary schools and colleges; educational and policy approaches in recreational or tourism settings for children; educational and policy approaches in occupational settings; interventions oriented to health-care settings and providers; interventions oriented to children's parents or caregivers; media campaigns alone; and communitywide multicomponent interventions (Table). The finding of insufficient evidence to determine effectiveness was most often based on the limited numbers of studies that measured behavioral or health outcomes, inconsistent evidence among studies that measured changes in sun-protective behaviors, and limitations in the design and execution of available studies. Summary tables of the reviews will be available at http://www.thecommunityguide.org/cancer when the full evidence is published in a supplement to the American Journal of Preventive Medicine. Use of Recommendations in Communities and Health-Care SettingsMalignant melanoma is the deadliest of the skin cancers, and its incidence in the United States has increased rapidly in the past 2 decades. Melanoma accounts for approximately three fourths of all skin cancer deaths. Basal cell and squamous cell skin cancers are seldom fatal but, if advanced, can cause severe disfigurement and morbidity (3). UV exposure in childhood and intense intermittent UV exposures are the major environmental risk factors for melanoma and BCC, and cumulative UV exposure is the major preventable risk factor for SCC (23). National surveys indicate that only one third of Americans practice sun-protective behaviors, and their practices vary greatly, depending on age, sex, and their ability to tan and burn (9,12,13). The two Task Force recommendations --- educational and policy approaches in primary schools, and educational and policy approaches for adults in outdoor recreational or tourism settings --- are based on improving covering-up behaviors. These recommendations represent tested interventions that promote decreased UV exposure at the community level. They can be used for planning interventions to promote UV protection or to evaluate existing programs. Several of the studies reviewed included multiple components that could not be evaluated separately. For example, a school-based program might involve components of policy, such as establishing school guidelines, in tandem with implementation of one-on-one didactic and interactive sessions regarding adapting sun-protective behaviors. Although sun-protective behaviors were increased by school-based programs, the specific effect could not be attributed to one specific intervention characteristic. In selecting and implementing interventions, the potential for an unintended increase in the duration and intensity of UV exposure must be considered. Also, communities should strive to develop comprehensive programs that include a wide range of activities suitable for their local resources, population characteristics, and settings. The other interventions reviewed, for which evidence was insufficient to determine effectiveness, could also prove useful. They provide a broader taxonomy of interventions that deserve further testing and evaluation, and the documentation of research gaps in these reviews could potentially help to improve the next generation of research. Additional information on research gaps will be provided in the report in the American Journal of Preventive Medicine. Choosing interventions that are well matched to local needs and capabilities, and then carefully implementing those interventions, are vital steps for increasing UV protection. Several factors can affect the attitudes, ability, and behaviors of a community regarding taking sun safety precautions. Some of the most important are program priorities, location of the community, and population. Establishing skin cancer prevention as a priority might be difficult because skin cancer is but one of many health topics, and for certain communities, may not be as high a priority as other cancers or diseases. Although it might be a higher priority in areas where UV radiation is more intense, even in areas with lower UV intensity, education about UV exposure during times of episodic exposure (e.g., during winter sports, when the sun comes out, and when traveling to higher UV intensity regions) could be helpful. Likewise, although skin cancer prevention might be a higher priority for populations at an increased risk (e.g., light-skinned, sun-sensitive), even darker-skinned or less sun-sensitive persons need to take precautions when exposed to UV radiation. To meet local objectives, recommendations and other evidence provided in the Community Guide should be supplemented with local information such as skin cancer incidence, skin cancer mortality, prevalence of sun-protective behaviors, latitude, UV index, resource availability, administrative structures, and economic and social environments of organizations and practitioners. These reviews by themselves do not provide advice regarding implementation of effective programs; the referenced articles, however, provide additional detail. Implementation advice is also available elsewhere (24--28). References
* Nevi are lesions of pigment-forming skin cells that can be a risk factor for melanoma. † Members of the coordination team were Rosalind Breslow, Ph.D., National Institutes of Health, Bethesda, Maryland; Peter Briss, M.D., CDC, Atlanta, Georgia; Patricia Buffler, Ph.D., University of California, Berkeley, Berkeley, California; Ralph J. Coates, Ph.D., CDC, Atlanta, Georgia; Steve Coughlin, Ph.D., CDC, Atlanta, Georgia; Debjani Das, M.P.H., New York City Department of Health and Mental Hygiene, New York, New York; Amy Degroff, M.P.H., CDC, Atlanta, Georgia; Diane Duñet M.P.A., CDC, Atlanta, Georgia; Nisha Gandhi, M.P.H., California Department of Health Services, Berkeley, California; Karen Glanz, Ph.D., University of Hawaii, Honolulu, Hawaii; Robert A. Hiatt, M.D., Ph.D., National Cancer Institute, Rockville, Maryland; Jon F. Kerner, Ph.D., National Cancer Institute, Bethesda, Maryland; Nancy C. Lee, M.D., CDC, Atlanta, Georgia; Patricia Dolan Mullen, Dr.P.H., University of Texas-Houston, Houston, Texas; Phyllis Nichols, M.P.H., CDC, Atlanta, Georgia; Barbara A. Reilley, Ph.D., Health Program Development, Houston, Texas; Barbara K. Rimer, Dr.P.H., University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Mona Saraiya, M.D., CDC, Atlanta, Georgia; Bernice Tannor, M.P.H., CDC, Atlanta, Georgia; S. Jay Smith, M.H.P.A., CDC, Atlanta, Georgia; Cornelia White, M.S.P.H., CDC, Atlanta, Georgia; Katherine M. Wilson, Ph.D., CDC, Atlanta, Georgia. § Members of the consultation team were Ross Brownson, Ph.D., St. Louis University School of Public Health, Saint Louis, Missouri; Robert Burack, M.D., Wayne State University, Detroit, Michigan; Linda Burhansstipanov, Dr.P.H., Native American Cancer Research, Pine, Colorado; Allen Dietrich, M.D., Dartmouth Medical School, Hanover, New Hampshire; Russell Harris, M.D., University of North Carolina School of Medicine, Chapel Hill, North Carolina; Tomas Koepsell, M.D., University of Washington, Seattle, Washington; Howard Koh, M.D., Massachusetts Department of Public Health, Boston, Massachusetts; Peter Layde, M.D., Medical College of Wisconsin, Milwaukee, Wisconsin; Al Marcus, Ph.D., AMC Cancer Center, Denver, Colorado; Margaret C. Mendez, M.P.A, Texas Department of Health, Austin, Texas; Amilie Ramirez, Ph.D., Baylor College of Medicine, San Antonio, Texas; Linda Randolph, M.D., National Center for Education on Maternal and Child Health, Arlington, Virginia; Lisa Schwartz, M.D., Department of Veterans Affairs Medical Center, White River Junction, Vermont; Robert Smith, Ph.D., American Cancer Society, Atlanta, Georgia; Jonathan Slater, Ph.D., Minnesota State Health Department, Minneapolis, Minnesota; Stephen Taplin, M.D., Group Health Cooperative, Seattle, Washington; Sally Vernon, Ph.D., University of Texas School of Public Health, Houston, Texas; Fran Wheeler, Ph.D., School of Public Health, University of South Carolina, Columbia, South Carolina; Daniel B. Wolfson, M.H.S.A., Alliance of Community Health Plans, New Brunswick, New Jersey; Steve Woloshin, M.D., Department of Veterans Affairs Medical Center, White River Junction, Vermont; John K. Worden, Ph.D., University of Vermont, Burlington, Vermont; Jane Zapka, Ph.D., University of Massachusetts Medical Center, Worchester, Massachusetts. ¶ Established market economies as defined by the World Bank are Andorra, Australia, Austria, Belgium, Bermuda, Canada, Channel Islands, Denmark, Faeroe Islands, Finland, France, Germany, Gibraltar, Greece, Greenland, Holy See, Iceland, Ireland, Isle of Man, Italy, Japan, Liechtenstein, Luxembourg, Monaco, the Netherlands, New Zealand, Norway, Portugal, San Marino, Spain, St. Pierre and Miquelon, Sweden, Switzerland, the United Kingdom, and the United States. ** These databases can be accessed as follows: MEDLINE: http://www.ncbi.nlm.nih.gov/PubMed; PsycINFO: DIALOG http://www.dialogclassic.com (requires id/password account), http://www.apa.org/psycinfo/products/psycinfo.html; CINAHL: DIALOG http://www.dialogclassic.com (requires id/password account), http://www.cinahl.com/wpages/login.htm. †† When information for both intervention and control groups was provided for times both before and after the intervention, net intervention effect was calculated as follows: ([Ipost -- Ipre]/Ipre) -- ([Cpost -- Cpre]/Cpre) where:Ipost = last reported outcome rate in the intervention group after the intervention; Ipre = reported outcome rate in the intervention group before the intervention; Cpost = last reported outcome rate in the comparison group after the intervention; Cpre = reported outcome rate in the comparison group before the intervention. If there was no concurrent comparison group, the net intervention effect was (Ipost -- Ipre)/Ipre and if there were no baseline measurements, the net intervention effect was calculated as (Ipost -- Cpost)/Cpost. Task Force on Community Preventive Services* Chair: Jonathan E. Fielding, M.D., Los Angeles Department of Health Services, Los Angeles, California. Vice-Chair: Patricia Dolan Mullen, Dr.P.H., University of Texas--Houston School of Public Health, Houston, Texas. Members: John Clymer, Partnership for Prevention, Washington, D.C.; Mindy Thompson Fullilove, M.D., New York State Psychiatric Institute and Columbia University, New York, New York; Alan R. Hinman, M.D., Task Force for Child Survival and Development, Atlanta, Georgia; George J. Isham, M.D., HealthPartners, Minneapolis, Minnesota; Robert L. Johnson, M.D., New Jersey Medical School, Department of Pediatrics, Newark, New Jersey; Garland H. Land, M.P.H., Center for Health Information Management and Epidemiology, Missouri Department of Health, Jefferson City, Missouri; Noreen Morrison Clark, Ph.D., University of Michigan School of Public Health, Ann Arbor, Michigan; Patricia A. Nolan, M.D., Rhode Island Department of Health, Providence, Rhode Island; Dennis E. Richling, M.D., Union Pacific Railroad, Omaha, Nebraska; Barbara K. Rimer, Dr.P.H.; School of Public Health, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina; Steven M. Teutsch, M.D., Merck & Company, Inc., West Point, Pennsylvania. Consultants: Robert S. Lawrence, M.D., Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland; J. Michael McGinnis, M.D., Robert Wood Johnson Foundation, Princeton, New Jersey; Lloyd F. Novick, M.D., Onondaga County Department of Health, Syracuse, New York. * Patricia A. Buffler, Ph.D., University of California, Berkeley; Ross Brownson, Ph.D., St. Louis University School of Public Health, St. Louis, Missouri; Mary Jane England, M.D., Regis College, Weston, Massachusetts; Caswell A. Evans, Jr., D.D.S., National Oral Health Initiative, Office of the U.S. Surgeon General, Rockville, Maryland; David W. Fleming, M.D., CDC, Atlanta, Georgia; Fernando A. Guerra, M.D., San Antonio Metropolitan Health District, San Antonio, Texas; Charles S. Mahan, M.D., College of Public Health, University of South Florida, Tampa, Florida; Susan C. Scrimshaw, Ph.D., University of Illinois School of Public Health, Chicago, Illinois; and Robert S. Thompson, M.D., Department of Preventive Care, Group Health Cooperative of Puget Sound, Seattle, Washington also served on the Task Force while the recommendations were being developed. Table 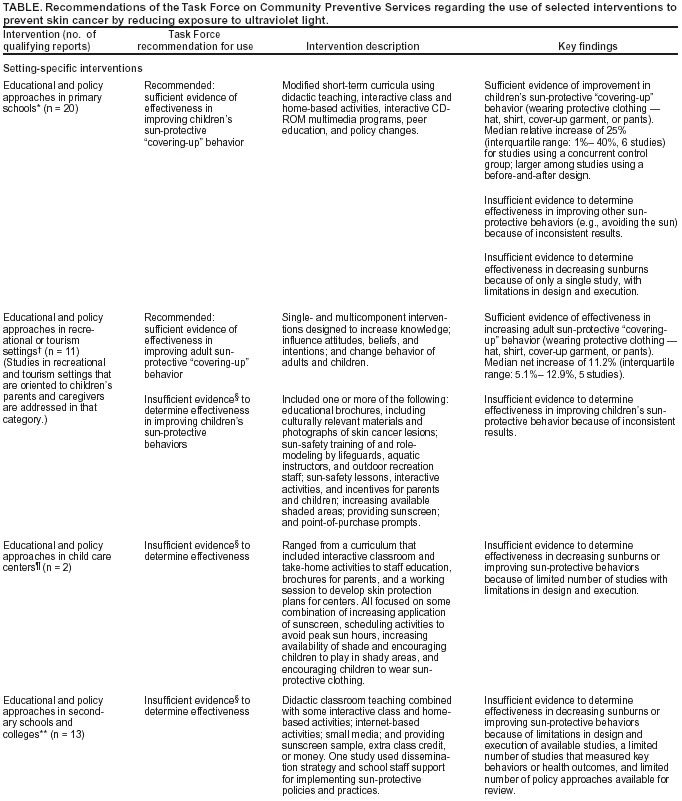 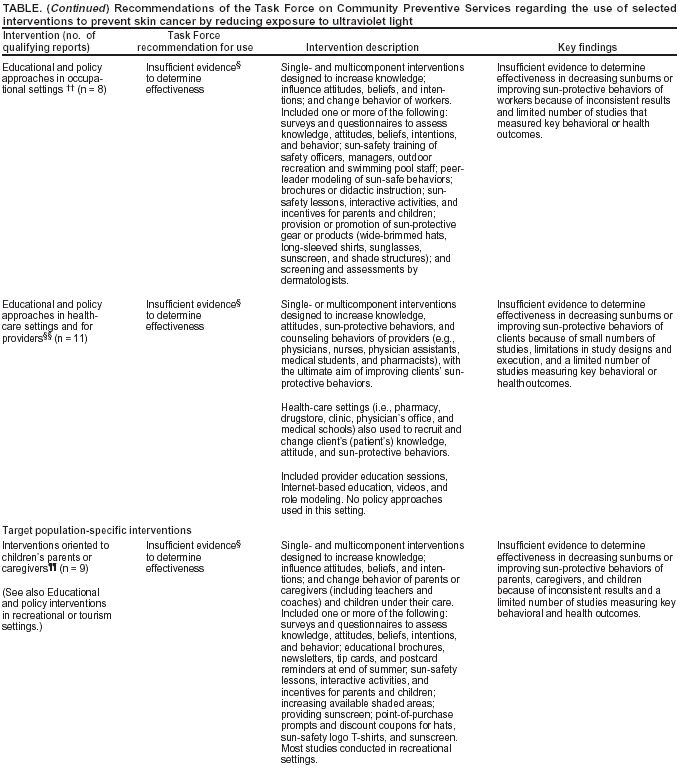 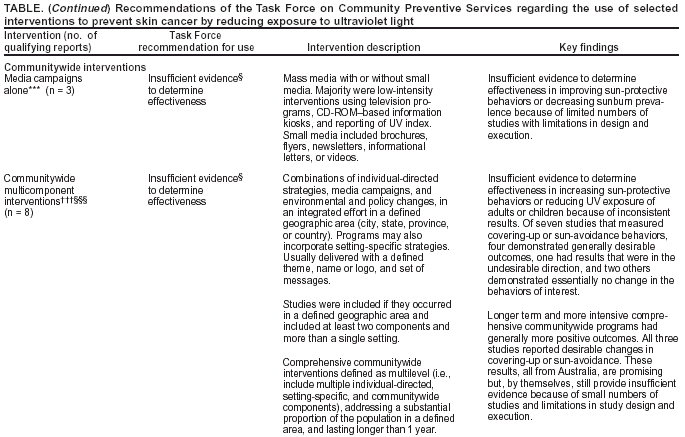 Return to top. Figure 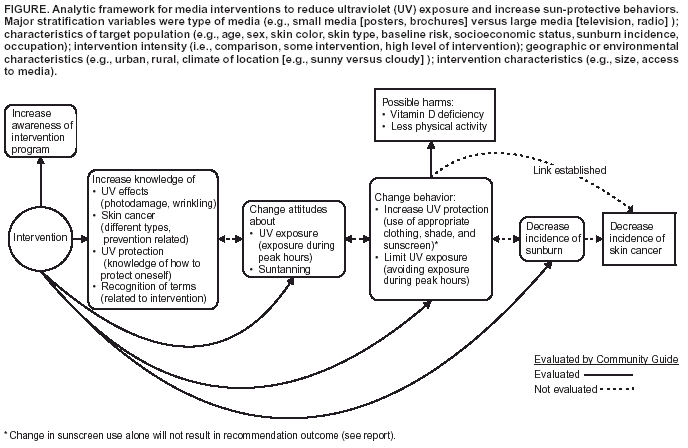 Return to top.
All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/2/2003 |
|||||||||
This page last reviewed 10/2/2003
|