

|

|

Volume 6: No. 3, July 2009
EDITORIAL
A Systems-Oriented
Multilevel Framework for Addressing Obesity in the 21st Century
Terry T. Huang, PhD, MPH; Adam Drewnowski, PhD; Shiriki K. Kumanyika,
PhD, MPH; Thomas A. Glass, PhD
Suggested citation for this article: Huang TT,
Drewnowski A, Kumanyika SK, Glass TA. A systems-oriented multilevel framework
for addressing obesity in the 21st century. Prev Chronic Dis 2009;6(3):A82.
http://www.cdc.gov/pcd/issues/2009/
jul/09_0013.htm. Accessed [date].
PEER REVIEWED
Effective or sustainable prevention strategies for obesity, particularly in
youths, have been elusive since the recognition of obesity as a major public
health issue 2 decades ago. Although many advances have been made with regard to
the basic biology of adiposity and behavioral modifications at the individual
level, little success has been achieved in either preventing further weight gain
or maintaining weight loss on a population level (1). To a great extent, this is
the result of the complex task of trying to change the way people
eat, move, and live, and sustaining those changes over time.
The most immediate cause of obesity is an imbalance of energy intake and
energy expenditure in the body. This energy imbalance, on the magnitude seen in
today’s population, arises from the complex interactions of biological
susceptibilities and socioenvironmental changes (2). Evidence in behavioral economics suggests that these
powerful biological and contextual forces often place eating and exercise
behavior beyond an individual’s rational control (3). Therefore, the solution to
the obesity epidemic lies in policies and interventions that alter those
contextual features, taking individual biology and preferences into account.
Historically, obesity research has been conducted within individual disciplines.
Now, for both scientific inquiry and for public policies, obesity should be
framed as a complex system in which behavior is affected by multiple
individual-level factors and socioenvironmental factors (ie, factors related to
the food, physical, cultural, or economic environment that enable or constrain
human behavior, or both). These factors are heterogeneous and interdependent,
and they interact dynamically (4).
Because of the complex system that affects obesity, researchers need to use a
systems-oriented approach to address the multiple factors and levels. Whereas
multidisciplinary research consists of teams with different expertise that can
contribute to the understanding of particular aspects of a larger research
question, truly cross-disciplinary research asks a priori questions and poses
hypotheses that cut across disciplines and across levels of influence. For
example, how do biological mechanisms of energy metabolism react to or how are
they affected by different features of the built, social, or economic
environment to produce a given distribution of eating or physical activity? How
do these conditions enable or constrain eating and physical activity, and how are
they embodied in biological systems to affect these behaviors?
In October 2007, the Eunice Kennedy Shriver National Institute of Child
Health and Human Development (NICHD) convened the international conference
Beyond Individual Behavior: Multidimensional Research in Obesity Linking Biology
to Society. The goal was to create a climate of training, funding, and academic
and institutional support for obesity research that will offer sustainable
solutions to the obesity problem. Participants hoped to bridge the factors that influence
obesity-related behaviors at the macro level (typically policies that shape and
govern the food, physical, social, and economic environments in which we live)
and the micro level (typically variables within people or their
immediate surroundings that influence health outcomes). The conference was
supported by the National Institutes of Health (National Cancer Institute;
National Institute of Diabetes and Digestive and Kidney Diseases; National
Heart, Lung, and Blood Institute; Division of Nutrition Research Coordination, Office of Behavioral and Social Sciences
Research; and Office of Disease Prevention), the Canadian Institutes of Health
Research (Institute of Nutrition, Metabolism, and Diabetes), and the Centers for
Disease Control and Prevention. The content of this 3-day conference was
designed to explicate the scientific foundation of this multilevel approach,
generate research questions that apply to all disciplines, consider different
intervention models, and discuss methods needed for the design and
analysis of systems-oriented, multilevel studies (5). The
essential elements of this multilevel agenda are framing obesity as a complex
systems problem; encouraging cross-disciplinary questions and hypotheses;
focusing on structural interventions (ie, modifications to the environment or policies); building capacity for multilevel
research and action; and taking a global perspective.
Back to top
Theoretical Framework of the Multilevel Model to
Address Obesity
Multilevel models are not new in public health; the concept stems from
socioecological theories (6) that emphasize the importance of social and
environmental factors in determining human behavior and health outcomes.
However, the model has been interpreted to describe ecologic layers without
elaborating on multiple sectors operating at multiple levels or including
bidirectional interactions of factors (7). Glass
and McAtee (8) present a multilevel model that is useful to address the complex,
interacting contexts for obesity prevention. This model (Figure 1), which was a
key focal point for the international conference, integrates biological (genes,
cells, and organs) and socioenvironmental (economics, culture, social networks, and
features of the physical environment) influences on behaviors such as eating and
physical activity. Time, on the horizontal axis, is in the context of life
course (conception to death) at the individual level or social change at the
population level. The vertical axis depicts
a nested hierarchy of systems including biological, social, and environmental
influences (8). This model shows that the behaviors leading to health outcomes,
not just health outcomes per se, are influenced by biological or
socioenvironmental factors.
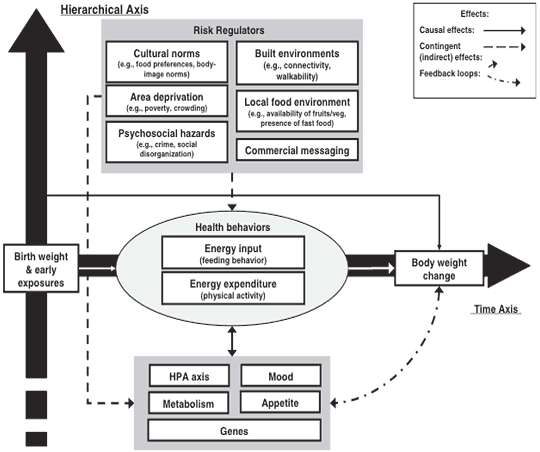
Figure 1. A systems-oriented, multilevel model applied
to the study of obesity. The contingent effects of risk regulators (ie,
embodiment, opportunity, and constraint) are shown with dotted arrows. “Causal”
effects of biological and behavioral variables are shown with solid arrows.
Feedback loops existing within grouped variables are not shown. Specific effects
and multiple, time-ordered feedback loops between variables are not shown in
order to reduce diagram complexity. Reprinted with permission from Elsevier (8).
[A text description of this figure is also
available.]
The model is consistent with economics and psychology in that
people are assumed to engage in behaviors based on preferences and attitudes. It
becomes multilevel in that a person is constrained by factors that exert
regulatory control on those behaviors. For example, food choices are made not
just on the basis of preferences but also on the basis of the price of food, the
cultural meaning of food, the availability of food, and the biological
responses to the reward value of food. The distribution of
these parameters constitutes a behavioral niche or landscape, to which the
person must adapt and respond according to particular goals and intentions.
The movement in time of higher or lower rates of obesity is, therefore, the
result of multiply-dependent and interlocking systems. There are 4 possible
implications. First, a single cause of the obesity epidemic is unlikely. Second,
the processes that give rise to increasing average body size probably involve combinations of factors at multiple levels of influence.
Third, small changes in 1 or more key factors may have large
and potentially nonlinear influences on distribution
of body weight. Finally, both socioenvironmental factors and biological
processes are involved in the expression of human behavior.
One problem with building a systems-oriented, multilevel framework for
obesity is that key influences in the physical or economic environment may not
fit conventional definitions of causes. Glass and McAtee contend that social
factors, such as social inequity and poverty, are difficult to study from a
traditional epidemiologic standpoint, in part because they do not fit the
definition of a causal risk factor (8). An alternative view of these variables is to define
them as risk regulators, or dynamic components of interconnected systems that
influence obesity-related behaviors from the personal level to the public policy
level (8). Systems of food distribution alter the probabilities at a population
level that these causes will align in ways that lead to different rates of
obesity (9). The search for a set of key risk regulators provides greater room
to consider the social, physical, cultural, and economic environments that
influence obesity.
The concept of risk regulators also may help overcome some of the
disadvantages of conventional socio-ecological models, namely the lack of
clarity on what is most important, where the key drivers are located, or what
the optimal intervention points are. The multiple levels
(individual vs community) require a bridging structure,
which act as conduits between macro-level forces and the factors in the local
environment that govern eating and activity. The temporally and
spatially distal forces that operate at the macro level cascade through
organizations, through systems of food distribution, through policies and
pricing, and eventually shape the reality that people perceive in
their lives. Examples of the bridging in the case of obesity could be cultural
norms, social networks, local food availability, food prices and taxes, physical
activity amenities, psychosocial stress, or economic insecurity. These might act
through neurologic or epigenetic regulatory pathways to affect behavior and to generate
feedback loops higher in the system. Epigenetic pathways are phenotypic
differences between individuals that are not a result of genetic composition per
se but a result of alterations in genetic expression through the silencing of
genes or interference with genetic transcription.
Back to top
Forming Cross-Disciplinary Questions and Hypotheses
for Research
Diverse sectors of society operate at different levels to influence
population energy balance (Figure 2) (2,10). Factors can range from the individual
level to the international level, and the sectors of influence include
education, agriculture, transportation, urban developments, and media, among
others, in addition to the
health sector. Research
that cuts across these different levels and sectors can be undertaken (Figure 2).
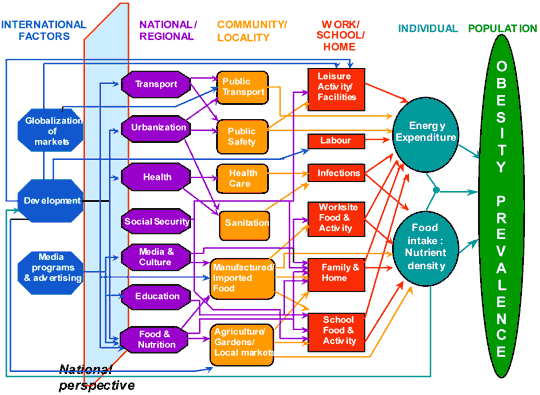
Figure 2. Levels of determinants and sectors of society
implicated in the complex systems of obesity. Reprinted with permission (2). [A
text description of this figure is also available.]
Obesity as a function of biology
The simplest biological view of obesity is that energy
intake (increased) and expenditure (decreased) became discordant over time. A decreased
sensitivity to metabolic signals that inhibit overeating is highly adaptive for
survival in circumstances where food availability is limited or cyclic, by
permitting storage of excess energy, when available, as body fat. However, when
an abundance of cheap, readily available, and palatable (eg, high-fat,
high-sugar) food is in the environment, this raised threshold of metabolic
tolerance promotes obesity (11). Failures in weight loss attempts are, in part,
the result of powerful biological drives to store and maintain energy in the
body.
An obesogenic prenatal environment can also increase the likelihood of
obesity in the offspring through epigenetic effects (12). These epigenetic
factors can be seen as biological risk regulators that might help explain, in
part, how the environment is embodied in metabolic systems to affect behavior
and health.
In animal studies, many prenatal
manipulations appear to promote offspring obesity by permanently altering
the development of central neural pathways that regulate food intake, energy
expenditure, and energy storage (13). Human imaging studies suggest that the
brain has automatic approach responses to food compared with nonfood objects
(14) and that these responses can be influenced by product advertising (15)
and pricing (16). The reward and executive control patterns in the brain can
be induced and modulated by palatable, energy-dense foods in a way similar
to addictive substances (17). These neural systems are powerful in defending
the body from undernutrition but have little capacity to defend against
overnutrition and upper limits of body weight and adiposity (18). So, what
other factors in the environment trigger or alter people’s biological
response to food to make them eat in a way that promotes weight gain? Recent research
points to elements of the social and physical
environment, and emerging evidence also suggests that the economic and policy environment
plays an important role. However, this area of research remains in its
infancy. Furthermore, almost no research explores how macro-level
variables influence biological processes to result in differential behavioral
phenotypes or how biological drivers of obesity are affected by different
socioenvironmental conditions.
Haemer et al (19) in this issue of Preventing Chronic Disease, explore in greater detail the
biological risk regulators of obesity. In addition, Esposito et al (20) offer a
developmental perspective to understanding how additional biopsychological
factors interact with the family and school context to shape food preferences in
children.
Obesity as a function of the built environment
The availability, accessibility, and marketing of foods all contribute to our
consumption patterns, either directly by enabling or constraining food choices
or indirectly by modulating biological processes to affect eating.
In the United States, the availability and accessibility of healthy foods, such
as fresh produce, are often limited, particularly in poor or rural communities
(21). Marketing of high-calorie foods via packaging, retail, and media to
children has increased purchase and consumption of those foods (22).
Many features of the built physical environment may also affect energy
expenditure. The lack of perceived safety, lack of facilities, and low access to
key destinations (eg, inconvenient transportation) are some of the factors that
inhibit or decrease physical activity levels (23). Physical activity improves insulin
sensitivity, glucose homeostasis, and other metabolic profiles (24), which in
turn can have an impact on adiposity (25). Reducing sedentary activity (eg,
television viewing, computer usage) in children reduces obesity, but this effect
appears to be mediated via a reduction in energy intake rather than an increase
in physical activity (26). If so, neurologic responses may also act as mediators
between sedentary activity and obesity.
With the emergence of geographic information systems technology, studying the built environment with objective measures in relation
to obesity is now more feasible. Mechanisms of the association between the built environment and
obesity remain poorly understood, particularly in terms of how the built
environment interacts with biology to influence obesity-related behaviors. As
Figure 1 illustrates, one should not assume that the
relationships between environmental factors and health behavior are direct or
linear.
Obesity as a function of the social environment
Norms of food and physical activity behaviors and body image ideals vary by
culture. Overweight in a child, for example, is viewed as a symbol of health by
some cultures (27). In a simple computational experiment, Hammond (28) showed
that changing norms of body weight, as the population becomes increasingly obese
over time, could in themselves propagate obesity.
Cultural forces can
also be barriers to obesity prevention. For instance, the American culture
places a strong emphasis on individual responsibility over one’s own lifestyle
or the lifestyle of one’s child. This cultural underpinning, in part, led to the
conventional emphasis on research and programs to educate or train people how to
behave in healthier ways. However, such individual-oriented approaches, which
usually do not take into account biological and socioenvironmental drivers of
behaviors, have rarely worked over the long term (29). Overcoming this
fundamental aspect of our sociopolitical culture must be considered in a
long-term solution to obesity.
Although many harmful social conditions (eg, poverty, pollution)
can end lives prematurely, they are not susceptible to change by those most
affected (ie, minority ethnic groups and children). Therefore, interventions
that rely on individual health promotion alone will bias outcomes toward the
more advantaged segments of the population, who have more choices about changing
their environments. Examining health disparities through the lens of social
disadvantage (eg, deprivation, discrimination-exclusion) rather than
epidemiologic trends alone will influence research questions, comparisons,
variables, and subgroups. Braveman discusses these concerns in this issue of Preventing Chronic Disease (30).
An increase in chronic stress (31) may be a way
through which social conditions interact with biological processes to affect
obesity-related behavior. Stress stimulates opioid release in the reward center
of the brain, which is a defense mechanism for the body to attenuate the
detrimental effects of stress. Chronic stress can repeatedly stimulate the
reward pathways and further enhance the reward value of food, possibly
contributing to increased energy intake and fat accumulation over time (32).
Obesity as a function of economics
In the United States, data suggest that poverty is associated
with higher obesity rates (33), whereas in many developing countries, higher
rates of obesity are found in higher-income groups as a result of economic
growth and improved standards of living (34). One explanation for these
observations is that low-income groups in the United States and high-income
groups in developing countries either are better able to afford or have greater
access to energy-dense but nutrient-poor foods (35). These foods have high
proportions of dietary fats, sugar, and refined grains, the cost of which has
steadily decreased while the supply has steadily increased over the
last 40 years (36). Nutrient-rich and energy-poor diets have much higher
costs per calorie (37). Therefore, a testable hypothesis linking macro-level
economics to obesity is that the higher cost of healthy foods may lead to
financial stress. This, coupled with the higher availability, accessibility, and
marketing of unhealthy foods in poorer neighborhoods, may lead to increased
purchase and consumption of unhealthy foods, which over time results in increased
obesity. Subsequently, increased obesity in the population can perpetuate itself
through intergenerational epigenetic programming.
The food
industry determines agricultural production, food manufacturing, processing,
packaging, transport, retail, and marketing to influence the eating patterns of
populations (38). The supply side of the food chain can be influenced by
agricultural policies on farm output, while the demand side can be influenced by
variables such as income, availability, and pricing. Furthermore, the foods that
farmers choose to grow are influenced by policies that support some foods more
than others; for example, corn and soybeans have, in general, more support than
fruits and vegetables. It remains to be investigated how the different
economic facets of food cause obesity variation across countries and people, how
much can be attributed to the role of policy in affecting producer and consumer
behavior, and how food production chains can be modified to shape future
consumer demand for healthier food options.
Back to top
Structural Modifications to Multilevel
Interventions
The next-generation interventions for obesity should start at the community
level
or higher, with multiple stakeholders that connect people, families,
schools, government, and the private sector. Intervention activities should
include not only educational schemes but also environmental changes to shift
norms and enable the adoption of healthy behaviors within everyday life. The
family, schools, primary care settings, and municipalities can be targeted
simultaneously as catchment sites to interface with children and parents. Media
organizations and businesses (eg, food manufacturers, retailers, supermarkets,
the transportation industry) can also help shift norms, effectively contributing
to both the supply and demand sides of the energy balance equation.
Much can be learned from the North Karelia Project in Finland from the 1970s
through the 1990s, where that country’s public health agency transformed the
lifestyle pattern of Finnish communities to reduce smoking rates and improve
dietary practices. The Finland project did not rely exclusively on
individually focused educational interventions. The government
created incentives for farmers to switch from meat to fruit and vegetable
production, and worked through social networks by using community organizations.
There were also efforts to use regulatory changes to influence the nutrient
content of food (eg, requiring sausage makers to lower the fat content of their
products across the entire market). The result was a greater than 50% reduction
in coronary heart disease mortality, as well as reductions in stroke, cancer,
and other diseases, in the entire country within 20 years (39).
Although research on multilevel interventions advances slowly, actions are
already being taken in many US and international communities. This parallel movement at the
grassroots level needs to be taken advantage of with rigorous evaluations to
determine the effect of community-initiated interventions (40). There is little
research on the dissemination and diffusion requirements of multilevel
interventions. As intervention and evaluation research continue, dissemination must be part of the strategic effort.
Back to top
Capacity Building for Multilevel Research and Action
Multilevel research and interventions cannot be conducted or sustained if the
agenda does not include a strong focus on building coalitions across societal
sectors and increasing the capacity to tackle obesity (41). Specifically,
public-private partnerships, leadership of national governments, and training of
future multilevel researchers and policy makers are warranted.
Public-private partnerships
Every person and every sector in society are important in a multilevel
approach to obesity. The food industry and industries that shape our built
environment have a role to play and should be invited to this research forum as
partners (see Huang and Yaroch [42]). Industry not only shapes the physical landscape of our environment but
also shapes values and norms. There is a need to agree on a public-private
partnership framework that outlines the rules of these collaborations.
Specifically, this framework must affirm that trade and health are not mutually
exclusive. It should articulate issues related to trust-building, information
sharing and technical cooperation, transparency of individual and collaborative
efforts, and pooling of resources. Successful partnerships must be constructed
through open, honest, and regular dialogues. As with any relationship, the
partners must be willing to take risks and to compromise to find common ground.
In addition, there must be leaders to champion the partnership and the cause the
partnership represents. Finally, sufficient resources must be made available to
implement any actions jointly developed by the partnership.
Role of national governments
The experience in North Karelia and experiences in tackling tobacco use in
the United States and other countries (43) suggest that top-down strategies must
accompany bottom-up approaches to sustain the necessary environmental and
behavioral changes to prevent obesity. Although individual-level interventions
have been effective in reducing smoking, their effect never could have been
sustained or scaled up to the population level in the absence of regulatory and
economic interventions by the government (44). Many policy options have been
proposed elsewhere (45), but few have been tested or evaluated to ascertain the
evidence of cost-effectiveness.
National governments also play a critical role in facilitating and
coordinating research and then translating research into programs and policies.
Coordination is essential among government and nongovernment agencies as well
as among different sectors in society. Leadership at the national level often is
necessary to move a multilevel agenda forward. For example, since 2005 the
Institute of Medicine has called for a national strategy on childhood obesity
that cuts across government agencies and societal sectors (46), but such a
national mandate has yet to be established (47).
Training
Training of future scientists is an indispensable component of the long-term
viability of any multilevel research agenda. Medical and public health training
contain little to no curriculum on systems science. A coordinated effort is
needed to develop training in a “multilevel science” in public health.
Training should include not only the knowledge base of obesity and chronic
disease prevention in general but also methodologic expertise for the design and
analysis of multilevel studies, including novel statistical and computational
approaches. Hammond discusses this training need in this issue (48). Training
should be integrated at the predoctoral, postdoctoral, and midcareer levels.
Back to top
Obesity From a Global Perspective
In the world, approximately 22 million children younger than age 5 years are
overweight. By 2015, an estimated 2.3 billion people aged 15 or older will
be overweight and 700 million will be obese worldwide (49). By 2010,
cardiovascular disease will be the leading cause of death in developing
countries, and by 2030 more than 280 million people in developing countries will have
type 2 diabetes (49). Key drivers of these numbers are transnational
(globalization of markets and media, urbanization, trade, economic growth, food
availability, marketing) (Figure 2), requiring a global perspective to address
obesity. The increasing health effects related to obesity will pose
substantial economic challenges as a result of cost and insufficient
infrastructure in the world’s health care systems (50). An unhealthy population
leads to reduced economic productivity, which further exacerbates morbidity and
mortality.
Experiences in the United States and other developed nations may serve as a
starting point for understanding and combating obesity in developing countries.
Nevertheless, factors may not all be equally relevant in different countries,
and environmental, cultural, and sociopolitical influences within countries
determine what types of solutions will be feasible and effective. More
international research is needed to understand these differences. For example,
the Seven Countries Study (51) on cardiovascular health provided great insight
into the role of population-level variations in diet in heart disease risk.
Although ecologic correlations are weak for supporting causal inference, this
study was groundbreaking in showing population-level influences on disease rates
and on preventive strategies. Obesity research can carry on these lessons.
International research that capitalizes on the contrast on either differing
obesity rates or differing socioenvironmental characteristics across contexts
can be especially illuminating.
Back to top
Conclusions
Current levels of obesity reflect complex social changes and
biological susceptibilities, and their interactions, during the last 40 years.
Individual behaviors such as eating and physical activity do not occur in a
vacuum; rather, they are influenced by socioenvironmental factors and by
powerful biological processes. Behavior change cannot be sustained if these
drivers of behavior are not considered. A systems-oriented, multilevel framework
encompassing science and research capacity-building is the way to generate
solutions that deal with the complex system in which obesity arises. A
multilevel research agenda is cross-disciplinary, bringing together expertise in
traditionally disparate fields to pose cross-disciplinary hypotheses and to test
those hypotheses collectively. The agenda also would extend conventional
research boundaries by tackling structural aspects of the social, physical, and
policy environment that affect obesity. Capacity building for global research is
critical for sustaining a multilevel research agenda for obesity and chronic
disease prevention.
Ultimately, interventions should strive to make healthy eating and physical
activity a natural and easy way of life. Using the framework discussed here, one
approaches the problem by first looking at the whole picture rather than
immediately zeroing in on a detail. Having a view, even if not a full
understanding, of the relations among factors that regulate energy balance,
across individuals as well as populations, allows one to simultaneously consider
multiple leverage points in the system within which obesity occurs that can or
need to be modified to yield the desired outcomes (52). Focused studies can then
be designed to confirm and quantify these relationships and to test their
effects. By nature, this systems-oriented, multilevel approach is
solution-oriented, underlining the philosophy that mechanistic and intervention
studies are worthy only if they can improve population health in a sustainable
way. Given where we are today, faced with the continued lack of effective and
sustainable prevention strategies, there is a critical need to
implement this multilevel approach. We can do this by extending the boundaries
of biomedical research to fill the gaps across all the disciplines relevant to
obesity, from biological and behavioral sciences to social and policy research.
Back to top
Acknowledgments
This article resulted from the conference Beyond Individual Behavior:
Multidimensional Research in Obesity Linking Biology to Society, hosted by NICHD,
October 10-12, 2007, in Arlington, Virginia. The conference was co-chaired by Drs
Huang and Glass.
We acknowledge the support of the co-sponsoring organizations
for the conference, the National Institutes of Health (National Cancer
Institute; Office of Behavioral and Social Sciences Research; Office of Disease
Prevention; National Heart, Lung, and Blood Institute; National Institute of
Diabetes and Digestive and Kidney Diseases; and Division of Nutrition Research
Coordination) and the Canadian Institutes of Health Research (Institute of
Nutrition, Metabolism, and Diabetes).
In addition, we gratefully acknowledge 2 strategic partners for the
conference: Centers for Disease Control and Prevention and the McGill University
Health Challenge Think Tank.
Back to top
Author Information
Corresponding Author: Terry T. Huang, PhD, MPH, Eunice Kennedy Shriver
National Institute of Child Health and Human Development, 6100 Executive
Boulevard, 4B11, Bethesda, MD 20892-7510. Telephone: 301-594-1846. Fax:
301-480-9791. E-mail: huangter@mail.nih.gov.
Author Affiliations: Adam Drewnowski, University of Washington School of
Public Health, Seattle, Washington; Shiriki K. Kumanyika, University of
Pennsylvania School of Medicine, Philadelphia, Pennsylvania; Thomas A. Glass,
The Johns Hopkins University Bloomberg School of Public Health, Baltimore,
Maryland.
Back to top
References
- Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ.
Interventions for preventing obesity in children. Cochrane Database Syst Rev
2005(3):CD001871.
- Kumanyika S, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ, Public
Health Approaches to the Prevention of Obesity (PHAPO) Working Group of the
International Obesity Task Force (IOTF).
Obesity prevention: the case for action. Int J Obes Relat Metab Disord 2002;26(3):425-36.
- Kahneman D. A perspective on judgment and choice: mapping bounded
rationality. Am Psychol 2003;58(9):697-720.
- Huang TT, Horlick MN.
Trends in childhood obesity research: a brief
analysis of NIH-supported efforts. J Law Med Ethics 2007;35(1):148-53.
- Huang TT, Glass TA.
Transforming research strategies for understanding and
preventing obesity. JAMA 2008;300(15):1811-3.
- McLeroy KR, Bibeau D, Steckler A, Glanz K.
An ecological perspective on
health promotion programs. Health Educ Q 1988;15(4):351-77.
- Diez Roux AV.
Integrating social and biologic factors in health research:
a systems view. Ann Epidemiol 2007;17(7):569-74.
- Glass TA, McAtee MJ.
Behavioral science at the crossroads in public
health: extending horizons, envisioning the future. Soc Sci Med
2006;62(7):1650-71.
- Schwartz S, Diez-Roux AV.
Commentary: causes of incidence and causes of
cases — a Durkheimian perspective on Rose. Int J Epidemiol 2001;30(3):435-9.
- Kumanyika SK.
Minisymposium on obesity: overview and some strategic
considerations. Annu Rev Public Health 2001;22:293-308.
- Levin BE.
Factors promoting and ameliorating the development of obesity. Physiol Behav 2005;86(5):633-9.
- Whitaker RC.
Predicting preschooler obesity at birth: the role of maternal
obesity in early pregnancy. Pediatrics 2004;114(1):e29-36.
- Levin BE.
Metabolic imprinting: critical impact of the perinatal environment on the
regulation of energy homeostasis. Philos Trans R Soc Lond B Biol Sci
2006;361(1471):1107-21.
- Killgore WD, Young AD, Femia LA, Bogorodzki P, Rogowska J, Yurgelun-Todd
DA.
Cortical and limbic activation during viewing of high- versus low-calorie
foods. Neuroimage 2003;19(4):1381-94.
- McClure SM, Li J, Tomlin D, Cypert KS, Montague LM, Montague PR.
Neural
correlates of behavioral preference for culturally familiar drinks.
Neuron 2004;44(2):379-87.
- Plassmann H, O’Doherty J, Shiv B, Rangel A.
Marketing actions can modulate neural representations of experienced
pleasantness. Proc Natl Acad Sci U S A 2008;105(3):1050-4.
- Volkow ND, O’Brien CP.
Issues
for DSM-V: should obesity be included as a brain disorder? Am J
Psychiatry 2007;164(5):708-10.
- Morrison CD, Berthoud HR.
Neurobiology of nutrition and obesity. Nutr
Rev 2007;65(12 Pt 1):517-34.
- Haemer MA, Huang TT, Daniels SR. The effect of neurohormonal factors,
epigenetic factors, and gut microbiota on risk of obesity. Prev Chronic Dis 2009;6(3).
http://www.cdc.gov/pcd/issues/2009/jul/09_0011.htm.
- Esposito L, Fisher JO, Menella JA, Hoelscher DM, Huang TT. Developmental
perspectives on nutrition and obesity from gestation to adolescence. Prev
Chronic Dis 2009;6(3).
http://www.cdc.gov/pcd/issues/2009/jul/09_0014.htm.
- White M.
Food access and obesity. Obes Rev 2007;8 Suppl 1:99-107.
- Committee on Food Marketing and the Diets of Children and Youth, McGinnis
JM, Gootman JA, Kraak VI, editors. Food marketing to children and youth:
threat or opportunity? Washington (DC): National Academies Press; 2006.
- Jones A, Bentham G, Foster C, Hillsdon M, Panter J. Tackling obesities:
future choices — obesogenic environments — evidence review. London (GB):
Government Office for Science, Foresight Programme; 2007. http://www.foresight.gov.uk/Obesity/03.pdf.
Accessed March 21, 2008.
- Maffeis C, Castellani M.
Physical activity: an effective way to control
weight in children? Nutr Metab Cardiovasc Dis 2007;17(5):394-408.
- Johnson MS, Figueroa-Colon R, Huang TT, Dwyer JH, Goran MI.
Longitudinal
changes in body fat in African American and Caucasian children: influence of
fasting insulin and insulin sensitivity. J Clin Endocrinol Metab
2001;86(7):3182-7.
- Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH,
et al. A randomized trial of the effects of reducing television viewing and
computer use on body mass index in young children. Arch Pediatr Adolesc Med
2008;162(3):239-45.
- Adams AK, Quinn RA, Prince RJ.
Low recognition of childhood overweight and
disease risk among Native-American caregivers. Obes Res 2005;13(1):146-52.
- Hammond RA. A complex systems approach to understanding and combating the
obesity epidemic. Washington (DC): Brookings Institution; 2008.
- US Preventive Services Task Force. The guide to clinical preventive
services 2006. Washington (DC): Agency for Healthcare Research and Quality, 2006.
- Braveman P. A health disparities perspective on obesity research. Prev
Chronic Dis 2009;6(3).
http://www.cdc.gov/pcd/issues/2009/jul/09_0012.htm.
- Whybrow PC. American mania: when more is not enough. New York (NY): WW
Norton and Company; 2005.
- Adam TC, Epel ES.
Stress, eating and the reward system. Physiol Behav
2007;91(4):449-58.
- Drewnowski A, Rehm CD, Solet D.
Disparities in obesity rates: analysis by
ZIP code area. Soc Sci Med 2007;65(12):2458-63.
- Nguyen MD, Beresford SA, Drewnowski A.
Trends in overweight by
socio-economic status in Vietnam: 1992 to 2002. Public Health Nutr
2007;10(2):115-21.
- Darmon N, Ferguson E, Briend A.
Do economic constraints encourage the
selection of energy dense diets? Appetite 2003;41(3):315-22.
- Drewnowski A, Darmon N.
The economics of obesity: dietary energy density
and energy cost. Am J Clin Nutr 2005;82(1 Suppl):265S-73S.
- Monsivais P, Drewnowski A.
The rising cost of low-energy-density foods. J
Am Diet Assoc 2007;107(12):2071-6.
- Hawkes C.
Uneven dietary development: linking the policies and processes
of globalization with the nutrition transition, obesity and diet-related
chronic diseases. Global Health 2006;2:4.
- Pekka P, Pirjo P, Ulla U.
Influencing public nutrition for
non-communicable disease prevention: from community intervention to national programme — experiences from Finland. Public Health Nutr 2002;5(1A):245-51.
- Diez Roux AV.
Next steps in understanding the multilevel determinants of
health. J Epidemiol Community Health 2008;62(11):957-9.
- Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, et
al. Population-based prevention of obesity: the need for comprehensive
promotion of healthful eating, physical activity, and energy balance: a
scientific statement from American Heart Association Council on Epidemiology
and Prevention, Interdisciplinary Committee for Prevention (formerly the
expert panel on population and prevention science). Circulation
2008;118(4):428-64.
- Huang TT, Yaroch AL. A public-private partnership model for obesity
prevention [letter to the editor]. Prev Chronic Dis 2009;6(3).
http://www.cdc.gov/pcd/issues/2009/jul/09_0034.htm.
- West R.
What lessons can be learned from tobacco control for combating the
growing prevalence of obesity? Obes Rev 2007;8 Suppl 1:145-50.
- Mercer SL, Green LW, Rosenthal AC, Husten CG, Khan LK, Dietz WH.
Possible
lessons from the tobacco experience for obesity control. Am J Clin Nutr
2003;77(4 Suppl):1073S-82S.
- Ashe M, Feldstein LM, Graff S, Kline R, Pinkas D, Zellers L.
Local
venues for change: legal strategies for healthy environments. J Law Med Ethics
2007;35(1):138-47.
- Koplan JP, Liverman CT, Kraak VI, editors. Preventing childhood obesity: health in the
balance. Washington (DC): The National Academies Press; 2005.
- Committee on Progress in Preventing Childhood Obesity. Progress in preventing childhood obesity: How do we
measure up? Washington (DC): The National Academies Press; 2007.
- Hammond RA. Complex systems modeling for obesity research. Prev Chronic
Dis 2009;6(3).
http://www.cdc.gov/pcd/issues/2009/jul/09_0017.htm.
- World Health Organization. Global strategy on diet, physical activity and
health. http://www.who.int/dietphysicalactivity/publications/facts/obesity/en/.
Accessed March 21, 2008.
- Finkelstein EA, Ruhm CJ, Kosa KM.
Economic causes and consequences of
obesity. Annu Rev Public Health 2005;26:239-57.
- Toshima H, Koga Y, Blackburn H, editors. Lessons for science from the
Seven Countries Study: a 35-year collaborative experience in cardiovascular
disease epidemiology. Tokyo (JP): Springer-Verlag Telos; 1995.
- Bar-Yam Y. Complexity rising: from human beings to human civilization, a
complexity profile. http://necsi.org/projects/yaneer/Civilization.html.
Accessed March 21, 2008.
Back to top
|
|
