

|

|

Volume
6: No. 3, July 2009
SPECIAL TOPIC
Adolescent Obesity and Social Networks
Laura M. Koehly, PhD; Aunchalee Loscalzo, PhD
Suggested citation for this article: Koehly LM,
Loscalzo A. Adolescent obesity and social networks. Prev Chronic Dis 2009;6(3):A99. http://www.cdc.gov/pcd/issues/2009/
jul/08_0265.htm. Accessed [date].
PEER REVIEWED
Abstract
The prevalence of overweight among children worldwide is growing at an alarming rate.
Social relationships may contribute to the development of obesity through the interaction of biological, behavioral, and environmental factors. Although there is evidence that early environment influences the expression of obesity, very little research elucidates the social context of obesity among children or adolescents. Social network approaches can contribute to research on the
role of social environments in overweight and obesity and strengthen interventions to prevent disease and promote health. By capitalizing on the structure of the network system, a targeted intervention that uses social relationships in families, schools, neighborhoods, and communities
may be successful in encouraging healthful behaviors among children and their families.
Back to top
Introduction
The prevalence of overweight among children has tripled in the last 40 years. Although recent data suggest that childhood overweight rates have begun to plateau, 32% of youth aged 2 to 19 years are overweight or at risk of becoming overweight (1,2). Furthermore, childhood overweight contributes to type 2 diabetes, adult obesity, and heart disease, along with impaired self-esteem and depression (3).
Adolescent overweight is largely a product of familial obesity risk (4), but environmental influences can augment the expression of overweight in children with a family history of obesity, continuing into adulthood. A social network approach to research and intervention design accounts for social contexts such as family, schools, neighborhoods, or communities, revealing how people are interconnected and influence
one another. A social network approach is a relational
perspective that frames research involving individuals and their families and communities, in addition to the methodologic tools that
are used in social network analysis. We discuss the use of a social network approach in interventions for adolescent overweight by considering 1) recent developments in the science of obesity genetics, 2) the importance of social context, 3) communal coping as a mechanism for behavior change within social networks, and 4) specific recommendations for using
social networks to prevent overweight.
Back to top
Obesity and Family History
A recent study estimates that more than 70% of adiposity in 10-year-olds is
due to genetic factors, and approximately 20% is due to socioenvironmental
contributions (4). Genome-wide association studies have located common genetic
variants associated with fat mass, weight, and susceptibility to obesity.
Several genes isolated through these studies, including FTO (5) and MC4R (6),
may eventually help scientists to explain the global scale of the obesity
epidemic and the biological mechanism for the heritability of obesity in
families.
Other research has identified factors associated with the behavioral
transmission of obesity risk from parents to their children (7). Eating disinhibition, susceptibility to hunger, and eating in the absence of hunger all
appear to be biologically heritable traits. Thus, a child’s family health
history, along with shared behaviors and familial environments, must be
considered in efforts to prevent and treat obesity (8).
Back to top
Early Social Environments and Overweight
Excessive caloric intake and a lack of physical activity are 2 major
environmental causes of adolescent overweight. Both structural and behavioral
environments in which adolescent social networks operate are inextricably linked
to their eating behaviors and physical activity levels.
Early childhood feeding practices are usually established in the home and
often translate into eating patterns during adolescence. Variations in food
preferences and portions among preschool children are associated with the extent
to which parents introduce new foods and encourage healthful eating habits (9).
Moreover, maternal feeding practices appear to influence the dietary patterns of
girls, suggesting that the relational significance of parental influence on
their children may be sex-specific (10).
Likewise, early childhood activity levels translate into similar patterns of
physical activity during adulthood (11). Physical activity among adolescents is
a social behavior, which is partly dependent on neighborhoods and recreational spaces.
Built environments can limit or facilitate levels of adolescent physical
activity. Playgrounds that are accessible via sidewalks and safe intersections
have been associated with higher levels of physical activity among youth (12).
Back to top
Adolescent Overweight and Social Networks
Mutual friendship ties, not merely biological family or relationships found
within the household, can contribute to an adult’s risk of obesity (13), but
little is known about whether the social mechanisms associated with weight gain
in adults pertain to adolescents. Studies of adolescent social networks have
identified the extent to which clique formation, the tendency for
people to form social ties with others who are similar (14), are associated with
weight status and physical activity. One study found that adolescent friendships
tended to cluster on the basis of weight status (15). The boys who were friends
engaged in similar levels of physical activity; however, this finding was not
noted within girl friendship networks (16). Another study found similarities in
the consumption of sweet foods and fast foods and types of physical activities
among male friends, and female friends were similar in the time spent on
computer-based leisure activities (17).
The mechanisms of social influence on adolescent overweight vary, but all
depend on social interaction. Parents can serve as role models, especially for
younger children whose health behaviors are completely influenced by their
parents’ habits (18), and older children may look to their friends, teachers,
and community leaders as role models for their own health behaviors (19).
Indirect processes can occur through cultural or group norms and attitudes. For
example, adolescents’ attitudes about body image can be influenced by social and
cultural norms (20).
Back to top
Communal Coping
A social network approach fits within a socioecological model for obesity
interventions, because social networks form and operate within the social contexts that influence health behaviors and
behavior change (21). Capitalizing on these interpersonal relationships may
enhance the effectiveness of health promotion interventions (22).
Communal coping is a process in which interpersonal relationships are the
conduit to behavior change among multiple members within a particular social
network, such as families (23). Its use in obesity prevention is novel, because
it prioritizes relational over individual processes. From a communal coping
perspective, individuals define themselves in terms of their interconnectedness
and relationships with their family, friends, neighbors, and community. Thus,
when faced with a shared health problem, a cooperative approach to address the
problem that involves family and friends may be particularly effective (23).
Health interventions that use communal coping can target 3 interpersonal
pathways (Figure 1): 1) communication about a health problem, such as shared
risk factors, 2) shared appraisals of the problem, and 3) development of
cooperative strategies to reduce negative impact (23). Interventions can focus
on educating family members about collective risk due to shared family history,
environment, and behaviors, and promoting increased communication about family
risk of overweight and associated diseases. Similar efforts can motivate
communication about shared risk factors among friends in neighborhoods and
communities, leading to shared appraisals among those who are socially
connected. The success of communal coping depends on cooperative support
mechanisms. Support can be directed at emotion-focused coping to address, for
example, low self-esteem or psychological impacts of stigma associated with
overweight and obesity. Cooperative support also can be geared toward problem-focused coping by
addressing dietary behavior and physical activity.
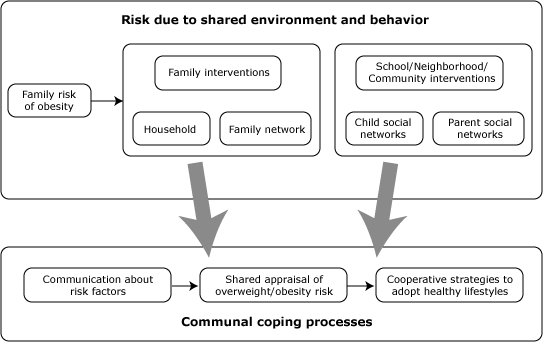
Figure 1. The communal coping framework. This
illustration shows the pathways through which increased risk due to shared
genes, environment, and behavior may lead to the process of communal coping.
Back to top
Using Social Network Approaches to Strengthen Obesity
Prevention
Obesity prevention must account for the complexity of overweight, including
a child’s familial risk of obesity and social relationships. Most previous interventions have focused on a single social sphere,
such as household or school. Furthermore, family-oriented interventions often engage
an affected child and a single caregiver, rather than considering the complex
social environment that might surround children and their families. An
intervention that focuses on the family system will have limited success without
consideration of the social influences on both parents’ and children’s behaviors
outside of the family context. Similarly, a school-based intervention that does
not consider the familial social environment or interpersonal influences within
the neighborhood or community settings would also be limited.
Thus, we recommend that interventions focus on 3 settings simultaneously
(Figure 2,
Table): R1 and R2) the household and the child’s
family outside of the household; R3) the neighborhood and community, to engage
the parents’ social network and social influences on the child outside of the
school setting; and R4) the school, to engage the child’s social network.
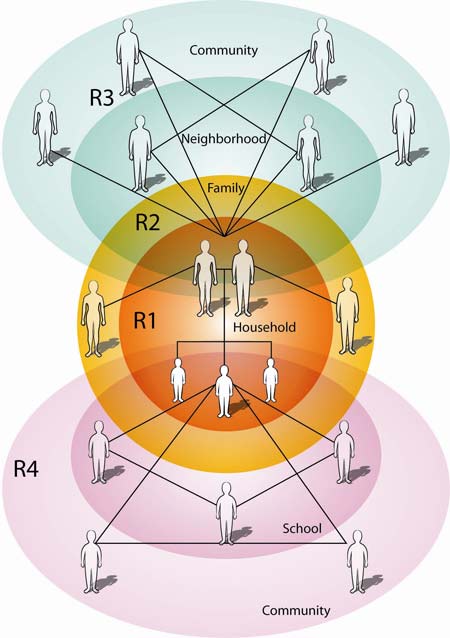
Figure 2. Recommendations (“R1” through “R4”) to
prevent and control adolescent overweight. This illustration shows how social
networks of children and parents interconnect with other social contexts that
are important to obesity prevention in adolescents.
Recommendation 1: Intervene with the family system, rather than with the
individual.
Primary prevention efforts may be more effective if they focus on the home
environment. To date, household-based interventions have been largely focused on
treatment of childhood overweight but not primary prevention. A detailed family
history capturing the constellation of family members who are overweight, and
associated diseases, can identify at-risk families for primary prevention
efforts. Adolescents can be engaged in the process of gathering family health
history of chronic illness and associated risk factors such as overweight, which
will provide an opportunity for families to communicate about their shared risks
(24).
Interventions based on the communal coping model could initially focus on
facilitating communication among household members and educating them about
their shared risk of disease. This process should engage multiple family members
and not be limited to an at-risk child and the primary caregiver. The key to
activating communal coping is to develop common appraisals of a shared health
threat among group members. In the case of a family-based intervention, a risk
assessment based on family history might motivate the perception of risk of
overweight as a household-level problem, warranting a household-level solution.
One model for developing risk assessments based on family risk is Family
Healthware. This software, developed by the Centers for Disease Control and
Prevention, produces an evaluation of an individual’s risk of
disease based on their family health history and recommends
health behaviors that may reduce their risk.
Recommendation 2: Tailor family-based interventions to the structure of the
family.
Because families are complex social systems, family-based interventions must
be flexible enough to adapt to the unique needs of individual families. Social
network approaches can be used to gather information on the existing
configuration of relationships within families, including family members outside
of the household, the composition of the family, the functional significance of
family ties, and the way social influence functions in each family. This
information can be used to determine the key people within the family who might
be able to exert a strong enough influence to change behavior. These optimally
positioned family members may receive training and education and be engaged as
“family leaders” who encourage cooperative strategies to increase physical
activity, prepare healthy meals, and provide moral support that may help to
sustain long-term behavior change within the family.
Cultural and sociodemographic factors are associated with the way families
are organized, the social significance of food, food preferences and eating
behaviors, and the way children are socialized. A formative assessment can
elucidate shared beliefs and behaviors of families that may not be apparent
through structural analysis. Such knowledge can lead to the design of culturally
appropriate intervention materials, which can then be implemented according to
unique family characteristics.
Recommendation 3: Design support mechanisms for parents and adult family
members on the basis of their social ties within the community.
Preventing childhood overweight is likely to have the most sustainability
when it is implemented early in the immediate family environments of young
children and continues through interventions in schools, neighborhoods, and
other community settings. Young children often model the health behaviors of
parents and other adults in their lives (18,19). To be positive role models for
the children in their homes, adult family members may need to change their own
lifestyles.
At the same time, the health of adult family members depends somewhat on
their social ties (13). Social ties and the structure of these ties can affect
behavior and health through social influence, social support, access to
resources, and access to information. Social psychological theories suggest that
a person’s friends are likely to share similar lifestyle behaviors, such as diet
and levels of physical activity, and thus be at similar risk for overweight.
One way to support obesity interventions among influential adults in
adolescents’ lives is to consider the social ties that influence adult eating
and physical activity behaviors. For example, using a social network approach,
cohesive subgroups of friends within neighborhoods and communities could be
identified for health promotion. A central person within the group can be
identified on the basis of the network’s structure and trained to act as the
liaison between the friendship network and the intervention team. The peer
leader can create opportunities for discussing lifestyle risk factors, provide
educational materials developed by the intervention team, and organize group
activities aimed at promoting healthful lifestyles among friends. By using the
naturally occurring structure of a group of friends, the designated leader will
have credibility within the group and be more effective in relaying helpful
information on diet and physical activity.
Neighborhood or community health promotion activities can be designed and
targeted to these friendship networks. For example, neighborhood “house parties”
may provide opportunities for friends to meet monthly, preassemble healthy
meals, and discuss educational materials with tips on how to provide a healthy
diet to their family. A similar approach can be used to increase physical
activity, for example, a coordinated effort within the friendship network to
exercise together several times a week. Targeting intervention activities to the
natural groupings of friends capitalizes on the social influence processes
inherent within friendship networks as well as the continued provision of social
support and encouragement of healthful lifestyles.
Recommendation 4: Use peer networks to encourage increased physical
activity.
Because adolescents seem to cluster according to physical activity levels
(15,17), network-based interventions may be particularly effective in developing
coordinated physical activity efforts among adolescent friends. The most popular
of these interventions encourages change in friendship networks through a peer
leader, a central influential person, or opinion leader selected on the basis of
the structure of social ties among the children within a classroom or community
organization. This approach is easy to implement, has been effective in smoking
prevention interventions (25), and has the potential to increase physical
activity among adolescents.
Overweight adolescents are often socially isolated, which in turn may lead to
“emotional eating” (3). Social network interventions might focus specifically on
helping isolated overweight adolescents form new social ties that have health
benefits. Classrooms and community settings are ideal for such activities. A
buddy system between people who were previously unconnected has been successful
in reducing social isolation; this peer-teaching intervention involved
older-younger schoolchildren pairs (26).
Team-based physical activity has been effective for weight reduction and
lifestyle change when at-risk and overweight youth were members of organized
sports teams (27). Motivating overweight youth to participate in these
team-based activities may require special support, such as school-based policies
and community programs designed specifically to meet the needs of children who
are overweight. One social network approach to encouraging participation in
organized sports could involve assigning team membership based on naturally
occurring friendships and cliques among overweight youth. This strategy would
simultaneously increase physical activity levels, encourage positive peer
influences on weight reduction, and reduce social isolation (3).
Back to top
Conclusion
According to Barabasi, “Growing interest in interconnectedness has brought into focus an often ignored issue: networks pervade all aspects of human health” (28).
Network perspectives will continue to advance the study of childhood and adolescent overweight. We suggest a new and stronger focus on the potential to garner interpersonal processes to address the obesity problem. Consideration of family and social networks may contribute to sustainable behavior change and improve the effectiveness of prevention and treatment interventions. Although challenging, curbing the obesity epidemic will undoubtedly depend on the coordinated efforts of many agencies
and institutions to support culturally sensitive programs that consider both family and peer interactions.
Back to top
Acknowledgments
The authors were supported in part by funding from the Intramural Research Program of the National Human Genome Research Institute and the Robert Wood Johnson Foundation. We thank Thomas Valente, Donna Stroup, Valerie Johnson, and
4 anonymous reviewers for reviewing an earlier version of the manuscript.
Back to top
Author Information
Corresponding Author: Laura M. Koehly, PhD, National Institutes of Health, Building 31, B1B37D, 31 Center Dr, MSC 2073, Bethesda, MD 20892. Telephone: 301-451-3999. E-mail:
koehlyl@mail.nih.gov.
Author Affiliation: Aunchalee Loscalzo Palmquist, National
Human Genome Research Institute, Bethesda, Maryland.
Back to top
References
- Obesity: preventing and managing the global epidemic. Geneva (CH): World Health Organization; 2000.
- Ogden C, Carroll M, Flegal K.
High body mass index for age among US children and adolescents, 2003-2006. JAMA 2008;299(20):2401-5.
- Fisberg M, Baur L, Chen W, Hoppin A, Koletzko B, Lau D.
Obesity in children and adolescents: working group report of the
Second World Congress of Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr 2004;39:S678-87.
- Wardle J, Carnell S, Haworth CMA, Plomin R.
Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am J Clin Nutr 2008;87(2):398-404.
- Haworth CM, Carnell S, Meaburn EL, David OS, Plomin R, Wardle J.
Increasing heritability of BMI and stronger associations with the
FTO gene over childhood. Obesity 2008;16(12):2663-8.
- Loos R, Lindgren C, Li S, Wheeler E, Zhao J, Prokopenko I, et al.
Common variants near
MC4R are associated with fat mass, weight and risk for obesity. Nat Genet 2008;40(6):768-75.
- Breen FM, Plomin R, Wardle J.
Heritability of food preferences in young children. Physiol Behav 2006;88:443-7.
- Kral TVE, Faith MS.
Influences on child eating and weight development from a behavioral genetics perspective. J Pediatr Psychol 2008 April. [Epub ahead of print].
- Russell CG, Worsley A.
A population-based study of preschoolers' food neophobia and its association with food preferences. J Nutr Educ Behav 2008;40:11-9.
- Birch LL, Fisher JO, Davison KK.
Learning to overeat: maternal use of restrictive feeding practices promotes girls' eating in the absence of hunger. Am J Clin Nutr 2003;78:215-20.
- Lau PW, Lee A, Ransdell L.
Parenting style and cultural influences on overweight children's attraction to physical activity. Obesity 2007;15(9):2293-302.
- Davison KK, Lawson CT.
Do attributes in the physical environment influence children’s physical activity? A review of the literature. Int J Behav Nutr Phys Act 2006;3:19.
- Christakis N, Fowler J.
The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357(4):370-9.
- Koehly LM, Shivy VA. Social environments and social contexts: social network applications in person environment psychology. Mahwah (NJ): Lawrence Erlbaum; 2000.
- Valente T, Fujimoto K, Chou C, Spruijt-Metz D. Adolescent affiliations and adiposity: a social network analysis of adolescent friendships and weight status. J Adolesc Health. In press.
- Fujimoto K, Valente T, Chou C, Spruijt-Metz D. Social network influences on adolescent weight and physical activity. Paper presented at: Sunbelt XXVIII International Sunbelt Social Network Conference; 2008; St. Pete Beach, FL.
- de la Haye K, Robins G, Mohr P, Wilson C. Obesity-related behaviors in adolescent friendship networks. Social Networks. In press.
- Scanglioni S, Salvioni M, Galimberti C.
Influence of parental attitudes in the development of children eating behaviour. Br J Nutr 2008;99(Suppl 1):S22-5.
- Cutting T, Fisher J, Grimm-Thomas K, Birch L.
Like mother, like daughter: familial patterns of overweight are mediated by mothers’ dietary disinhibition. Am J Clin Nutr 1999;69:608-13.
- Boyington JE, Carter-Edwards L, Piehl M, Hutson J, Langdon D, McManus S. Cultural attitudes toward weight, diet, and physical activity among overweight African American girls. Prev Chronic Dis 2008;5(2):1-9.
http://www.cdc.gov/pcd/issues/2008/apr/07_0056.htm.
- Sallis JF, Owen N. Ecological models of health behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: theory, research, and practice. 3rd ed. San Francisco (CA): Jossey-Bass; 2002. p. 462-84.
- Koehly LM, McBride C. Genomic risk information for common health conditions: Maximizing kinship-based health promotion. In: Tercyak K, editor. Handbook of genomics and the family. New York (NY): Springer; In press.
- Afifi T, Hutchinson S, Krouse S. Toward a theoretical model of communal coping in postdivorce families and other naturally occurring groups. Commun Theory 2006;16:378-409.
- Williams R, Hunt S, Heiss G, Povince M, Bensen J, Higgins M.
Usefulness of cardiovascular family history data for population-based preventive medicine and medical research (The Health Family Tree Study and the NHLBI Family Heart Study). Am J Cardiol 2001;87:129-35.
- Valente T, Hoffman B, Ritt-Olson A, Lichtman K, Johnson A.
Effects of a social-network method for group assignment strategies on peer-led tobacco prevention programs in schools. Am J Public Health 2003;93(11):1837-43.
- Stock S, Miranda C, Evans S, Plessis S, Ridley J, Yeh S, et al.
Health buddies: a novel, peer-led health promotion program for the prevention of obesity and eating disorders in children in elementary school. Pediatrics 2007;120(4):e1059-68.
- Weintraub D, Tirumalai E, Haydel K, Fujimoto M, Fulton J, Robinson T.
Team sports for overweight children. Arch Pediatr Adolesc Med 2008;162(3):232-7.
- Barabasi A.
Network medicine — from obesity to the “diseasome.” N Engl J Med 2007;357(4):404-7.
Back to top
|
|
