|

|

Volume
6: No. 2, April 2009
TOOLS AND TECHNIQUES
An Emergency Medical Services Toolkit for Improving Systems of Care for Stroke in North Carolina
Ishmael Williams, Greg Mears, MD, FACEP, Cindy Raisor, BSN, MA, Jenny Wilson
Suggested citation for this article: Williams I, Mears G, Raisor C, Wilson J. An emergency medical services toolkit for improving systems of care for stroke in North Carolina. Prev Chronic Dis 2009;6(2):A67.
http://www.cdc.gov/pcd/issues/2009/
apr/08_0175.htm. Accessed [date].
Abstract
The Centers for Disease Control and Prevention is partnering with the National Association of Chronic Disease Directors and the North Carolina Office of EMS to design, develop, and implement an emergency medical services (EMS) performance improvement toolkit to evaluate opportunities to improve the emergency identification and treatment of acute stroke. The EMS Acute Stroke Care Toolkit is being developed, tested, and implemented in all 100 counties in the state by the EMS Performance
Improvement Center, the agency that provides technical assistance for EMS in North Carolina. The
toolkit helps each EMS system in defining, measuring, and analyzing their system of care and promotes collaboration through public education, regional stroke planning with hospitals, EMS service configuration, EMS staffing patterns, EMS education, and timely care delivery. We outline the issues surrounding acute stroke care, the role of emergency medical systems in stroke
care, and the components of the EMS Acute Stroke Care Toolkit designed to improve EMS systems and outcomes for stroke patients.
Back to top
Background
Stroke is the third leading cause of death in the United States. Each year, approximately 700,000 people suffer a first-time or recurrent stroke, approximately 25%
of whom die from stroke-related causes, and another 15% to 30% of whom remain permanently disabled (1).
The Centers for Disease Control and Prevention (CDC) reported that
in 1999, approximately 48% of stroke deaths occurred pretransport (before transport to a hospital emergency department) (2). The percentage of pretransport deaths by state
ranged from 23% to 67%, and 8 states had proportions greater than 60%. The study found that ischemic strokes, those strokes caused by a blockage in an artery that supplies blood to the brain, accounted for 68% of all
out-of-hospital stroke deaths (2). A follow-up study by CDC found that, although the stroke death rate decreased from 61.6 per 100,000 in 1999 to 56.2 per 100,000 in 2002, the percentage of out-of-hospital deaths was unchanged. In 2002, of 162,672 deaths from
stroke, 49% of the patients died before being transported to a hospital (3).
This high rate of death due to stroke before arrival at the hospital is
troubling, considering the promising stroke treatment options that exist. One
treatment for ischemic stroke, thrombolytic (“clot-busting”) therapy, was
approved for use in the United States by the Food and Drug Administration in
1996 and works well if administered within the first 3 hours of the onset of
symptoms. However, in 2004, only 3% to 8.5% of stroke victims received this
treatment (4). Reasons most frequently cited for not receiving treatment were
delays in 1) calling 9-1-1, 2) transporting patients to a hospital capable of handling stroke patients, and
3) diagnosing and treating patients after they arrive at the hospital (4).
Retrospective studies have found that the biggest portion of the delay between onset of symptoms and emergency treatment is the time it takes for a patient to recognize the signs of stroke and decide to seek medical care (5-8). Between
one-half and three-quarters of ischemic stroke patients do not arrive at the hospital within the 3-hour window of treatment that is needed to make an assessment and begin therapy. Some of the factors in the delays include lack of knowledge regarding 1) stroke
symptoms, 2) treatment options, and 3) the need for quick therapy (5-8).
Delays in treating stroke also occur because of poor recognition of stroke by 9-1-1 dispatchers and misdiagnosis of stroke by emergency medical services (EMS) personnel. Dispatch is a crucial link in the chain of care, yet dispatchers miss as many as 70% of stroke cases because they do not have the understanding or tools to properly assess the symptoms reported by callers. A similarly high misdiagnosis rate (61%) was documented for the responding EMS personnel when diagnosing stroke in
the field (9).
These findings underscore the challenges facing emergency systems of care. The lack of close coordination of stroke care among health care providers has resulted in a fragmented system for stroke prevention, emergency care, treatment, and rehabilitation. Several key stroke care stakeholders have made recommendations to address these problems (10-19). Their recommendations call for better integration of the facilities, agencies, and professionals that provide stroke care. These recommendations
include rapid access to EMS, use of diagnostic algorithms and EMS protocols that reflect the most current stroke treatment recommendations and dispatch EMS with the most rapid emergency response possible, direct involvement of emergency physicians and stroke experts in designing protocols and training, stroke assessment and thrombolytic screening, and rapid transport to a stroke center (16).
To address the recommendations from these organizations, CDC, the National Association of Chronic Disease Directors, and the North Carolina Office of EMS are developing and implementing an EMS performance improvement toolkit (a statistical analysis report on EMS patient data) to evaluate opportunities for improvement in the emergency identification and treatment of acute stroke. This toolkit is being implemented
by using an evidence-based approach established by the National EMS Information
System (NEMSIS) to define, document, and evaluate EMS service delivery.
Back to top
National EMS Information System
NEMSIS is a standardized data set and data transmission standard for service delivery and patient care. It has been endorsed by all 56 states and territories and has been implemented in 42 states (20). NEMSIS was initially created through an
industry-wide consensus process. The goal was to establish an electronic EMS data system at the local level that would collect and maintain EMS service delivery and patient care data. These data represent an EMS patient care event
beginning with the 9-1-1 call to activate EMS through the transport or disposition of the patient by EMS. A subset of these data is electronically submitted to a state EMS database. The state data are used to support the state EMS infrastructure and to drive policy, funding, and other EMS needs. A subset of the state EMS database is submitted to a national EMS database. This national database describes the EMS industry, service delivery, and patient care from a national perspective. Data from
the national database are used to support EMS policy, advocacy, funding, and education (21).
Twelve states, including North Carolina, provide data for the national EMS database
as of January 2009 (20).
NEMSIS uses a standardized data dictionary, which permits data-driven analyses and assessment of an EMS system’s performance, procedures, personnel, and patient outcomes. Standardized data also enable comparison or benchmarking across jurisdictional and state boundaries and describe national trends. As trends and performance benchmarks are identified, we can identify and define EMS needs, develop evidence-based EMS treatment protocols, support and justify EMS funding, establish EMS
policy, and target EMS research.
EMS toolkits are designed to improve the quality of EMS care by providing
tools to measure and analyze key processes or components of using a “systems
of care” approach. By defining, measuring, analyzing, and recommending
adjustments to the key processes associated with EMS service delivery,
personnel performance, and patient care, an EMS system can make changes to
optimize performance over time. Toolkits identify best practices that can be
shared anonymously to allow comparisons and benchmarking of service delivery
and patient care among similar EMS systems across the state.
The EMS toolkits are one component of a statewide program for EMS quality
improvement using the data-driven quality control strategy Six Sigma. First
used in manufacturing by Motorola, Six Sigma has been tested and adapted to
areas including health care delivery. It promotes incremental quality
improvement through processes for defining, measuring, analyzing, improving,
and controlling performance (22).
Back to top
The North Carolina EMS Acute Stroke Care Toolkit
The North Carolina Office of EMS created the NEMSIS-based North Carolina Prehospital Medical Information System (PreMIS), which is maintained by the EMS Performance Improvement Center (EMSPIC) at the University of North Carolina
at Chapel Hill. All 100 North Carolina counties are required by law to provide data to the North Carolina Office of EMS through the PreMIS data system. More than 1 million EMS calls each year occur within North Carolina and are recorded in the database.
A focal point of EMSPIC has been to provide ongoing technical support to
local EMS systems by developing and implementing EMS performance improvement
toolkits. These toolkits are data analysis programs that enable statistical
analysis of an EMS system’s care for a specific patient population. The toolkits
use SAS software (SAS Institute, Cary, North Carolina) and create graphic reports on a Web browse-based interface accessible by authorized EMS managers. The toolkits
help
local and state EMS systems evaluate and improve EMS service delivery, personnel performance, and patient care.
Development of toolkits for EMS systems was initiated in 2004 under a 3-year
grant provided by The Duke Endowment. Five EMS system toolkits were initially
developed and implemented; they addressed system response time, acute trauma
care, cardiac arrest care, acute pediatric care, and acute cardiac care. The EMS
Acute Stroke Care Toolkit, funded by CDC, was an additional EMS toolkit
developed and implemented by EMSPIC in 2007 (22).
The design of the EMS Acute Stroke Care Toolkit included industry standards when possible. If there were no accepted industry standards, a consensus process was used. Two expert panels convened to identify and agree on emergency stroke care indicators and to convert the indicators into performance measures and a basic design for the toolkit. The panel members represented a broad spectrum of stroke and EMS expertise (23).
The EMS Acute Stroke Care Toolkit reports on many broad indicators of systems of care for stroke, including stroke incidence and death rates from CDC, demographic characteristics of stroke patients, and the socioeconomic background of the service area of the EMS system
from US Census Bureau statistics. The toolkit tracks EMS involvement in local community education and stroke prevention programs and EMS participation in the North Carolina Stroke Initiative — a statewide effort to engage EMS
systems and hospitals to optimize care for stroke patients focusing on critical time intervals and interventions. To promote cardiovascular health in the EMS workforce, the toolkit recommends implementing an EMS workforce health and safety plan in each EMS system (24).
The EMS Acute Stroke Care Toolkit uses approximately 60 data elements to describe and measure the performance and effectiveness of an EMS system, beginning with the initial 9-1-1 call through the treatment and disposition of the stroke patient. Data collected during an EMS event is closely monitored by the EMSPIC staff for accuracy and completeness at the local level. This monitoring ensures decisions are made with the best possible information. Data quality, completeness, and
validity are analyzed and reported as a component of each toolkit.
From the perspective of patient outcome, the EMS Acute Stroke Care Toolkit focuses on 5 key patient care interventions:
- Prompt recognition of stroke through the use of stroke screening.
- Documentation of stroke symptom onset.
- Screening the blood glucose of the patient for hypoglycemia.
- Maintaining EMS scene times of 10 minutes or less.
- Rapid transport (with early notification) to a stroke center.
An extensive set of observations is collected for each EMS event. These data are used to measure and analyze the EMS service delivery and stroke care interventions. The observations include time intervals for each stage of response, treatment, and transport
(Table 1). The time fractions collected can be divided as follows: 1) the time to dispatch an ambulance
after the 9-1-1 call, 2) the time to get the ambulance moving after dispatch, 3) the time to get to the scene, 4) time spent at
the scene, and 5) the time to get the patient to the hospital after leaving the scene.
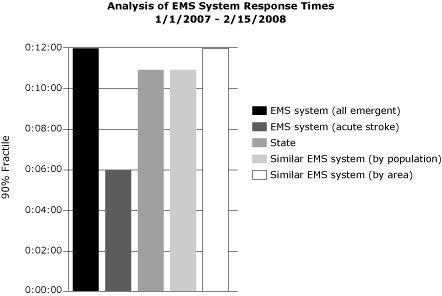
The EMS Acute Stroke Care Toolkit calculates (within a user-specified range of dates) EMS system time intervals for all EMS events in the database. These intervals
present in hours, minutes, and seconds
the minimum, maximum, and average time to respond to a call; the 90% fractile (the
maximum response time for 90% of events); and the standard deviation. Each of these calculations are made with 5 levels of comparison: 1) the EMS system’s emergency calls
(lights and sirens used), 2)
the EMS system’s stroke events (stroke patients), 3) the entire state’s stroke events, 4) stroke events for EMS systems in the state that serve similar population sizes, and 5) stroke events for EMS systems in the state that serve similarly sized areas
(Figure) (24).
| System |
Events (n) |
Minimum Value |
Maximum Value |
Average Value |
90% Fractile |
Standard Deviation |
| EMS system (all emergent) |
593 |
0:00:00 |
0:29:00 |
0:06:28 |
0:12:00 |
0:04:19 |
| EMS system (acute stroke) |
2 |
0:00:00 |
0:06:00 |
0:02:20 |
0:06:00 |
0:03:13 |
| State |
41,430 |
0:00:00 |
1:35:00 |
0:06:17 |
0:11:00 |
0:04:09 |
| Similar EMS system (by population) |
15,073 |
0:00:00 |
1:09:00 |
0:06:07 |
0:11:00 |
0:04:00 |
| Similar EMS system (by area) |
16,182 |
0:00:00 |
1:35:00 |
0:06:19 |
0:12:00 |
0:04:32 |
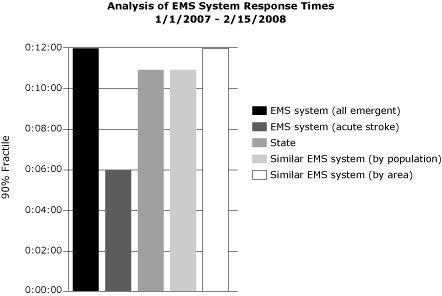
Figure. An example analysis of an emergency medical
services (EMS) system’s response time in hours, minutes, and seconds (time beginning with the dispatch of
an EMS vehicle and ending with the arrival of the EMS vehicle at the scene
of an EMS event) for January 1, 2007, through February 15, 2008. Only
emergent events when lights and sirens were used are included in the
calculations. All of the EMS system’s events are compared with acute
stroke events, the entire state’s emergent events, and the response times
for stroke events for similar EMS agencies (by population and by area).
Uncontrollable factors that affect the reported time intervals by causing delays are weather, traffic or crowds, safety concerns, vehicle failure, vehicle crash, language barriers, distance, problems with directions, and hazardous materials. Such factors are reported for the acute stroke calls only for response, scene, and transport. The toolkit reports the total number of delays by type and the percent of total EMS responses each delay type represents.
EMS treatment protocols for stroke care are reported in depth, and protocol compliance is tracked at the individual EMS professional and at the stroke patient level
(Table 2). North Carolina’s EMS protocols
are a set of best practices determined by the North Carolina College of Emergency Physicians (25) and other stroke experts. The stroke protocol requires documentation of onset time of symptoms, completion of stroke
screen, blood glucose (for hypoglycemia) and thrombolytic screening (to identify
patients who would benefit from clot-busting drug treatment),
an EMS scene time of 10 minutes or less, and documentation of the patient’s cardiac rhythm
for to check for arrhythmias.
The EMS Acute Stroke Care Toolkit summarizes all of the EMS data elements stored in the PreMIS database for a period of time determined by the user. The EMS system’s administrator compares his or her system’s results for a selected time period with the state’s results and results from other EMS systems that cover similarly sized areas and populations. The toolkit also allows EMS administrators to make historic comparisons to evaluate the effects of any change or
intervention. The EMS Acute Stroke Care Toolkit has 28 interventions or recommendations for improvement (Table 3). Each of these interventions is specific to a performance measure or finding in the toolkit. Each time a toolkit report is generated, the EMS system receives 12 to 15 recommendations or suggestions for improvement.
Toolkit-based interventions also serve as a built-in evaluation for any EMS system changes implemented to improve EMS service delivery, personnel performance, or patient care. Once an intervention has been implemented in an EMS system, all data collected will reflect this change.
After enough data on EMS events or patient records have been collected, the toolkit can be regenerated to assess the performance improvement since the previous toolkit report and the progress achieved in meeting the
benchmarks.
Back to top
Conclusions
The EMS Acute Stroke Care Toolkit is a component of a larger nationwide movement to improve stroke outcomes by integrating and improving the entire chain of medical care for stroke from the recognition of signs and symptoms to recovery and rehabilitation.
The toolkit addresses the first level of emergency care — response time,
diagnosis, collection of medical history and symptom onset times, stabilization,
thrombolytic screening, and quick transport to a hospital capable of handling
stroke care. All these elements are critical if stroke patients are to obtain
the best chance for positive outcomes from definitive treatment. The EMS Acute Stroke Care Toolkit and NEMSIS represent a major step in identifying the evidence-based EMS practices needed to improve emergency stroke treatment. Each toolkit identifies interventions to improve EMS, gauges the success of the interventions, and helps identify other areas that need incremental improvement.
The next phase of the EMS Acute Stroke Care Toolkit, which has been funded
for 2 years starting in 2009, will include a toolkit usability study that will gather input from EMS managers, evaluate the effectiveness of the toolkit for incremental improvement, and implement the toolkit in South Carolina and West Virginia, which have recently started using PreMIS. CDC is also working in North Carolina with the EMSPIC and the Coverdell Stroke Registry for hospitals to link EMS and hospital data sets so that patient outcomes
can be assessed across the spectrum of care. This effort involves linking the patient records in the 2 databases and evaluating EMS protocols with respect to emergency care and hospital care. Plans also include a version of the toolkit that could be used by other states and local EMS systems
that use the NEMSIS standard.
An EMS Acute Stroke Care Toolkit with real data (blinded to patient and EMS
system identity) is available at www.emspic.org/?q=node/27. Additional information on this and other EMS toolkit projects and the EMSPIC is available at www.emspic.org.
Back to top
Author Information
Corresponding Author: Ishmael Williams, Epidemiology and Surveillance Branch, Division for Heart Disease and Stroke Prevention, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Mail Stop K-47, 4770 Buford Hwy, NE, Atlanta, GA 30341-3717. Telephone: 770-488-8060. E-mail:
Ishmael.Williams@cdc.hhs.gov.
Author Affiliations: Greg Mears, Jenny Wilson, University of North Carolina
at Chapel Hill, Chapel Hill, North Carolina; Cindy Raisor, EMS Performance LLC, Chapel Hill, North Carolina.
Back to top
References
- American Heart Association. Heart and stroke statistics — 2007 update
at-a-glance. Dallas (TX): American Heart Association; 2007.
http://www.americanheart.org/downloadable/heart/
1166712318459HS_StatsInsideText.pdf. Accessed February 26, 2008.
- Centers for Disease Control and Prevention.
State-specific mortality from stroke and distribution of place of death —
United States, 1999. MMWR Morb Mortal Wkly Rep 2002:51(20);429-33.
- Centers for Disease Control and Prevention.
Place of death after stroke — United States, 1999-2002. MMWR Morb Mortal Wkly Rep 2006;55(19):529-32.
- Reeves MJ, Arora S, Broderick JP, Frankel M, Heinrich JP, Hickenbottom S,
et al. Acute stroke care in the US: results from four pilot prototypes of the Paul Coverdell National Acute Stroke Registry.
[Published erratum in: Stroke 2005;36(8):1820]. Stroke 2005;36(6):1232-40.
- Smith MA, Doliszny KM, Shahar E, McGovern PG, Arnett DK, Luepker RV.
Delayed hospital arrival for acute stroke: the Minnesota Stroke Survey. Ann Intern Med 1998;129(3):190-6.
- Rosamond WD, Gorton RA, Hinn AR, Hohenhaus SM, Morris DL.
Rapid response to stroke symptoms: the
Delay in Accessing Stroke Healthcare (DASH) study. Acad Emerg Med 1998;5(1):45-51.
- Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S.
Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke 2000;31(11):2585-90.
- Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR.
Determinants of use of emergency medical services in a population with stroke symptoms: the Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke 2000;31(11):2591-6.
- Brice J, Murdock M, Acker III J. The stroke rapid response project: an interim report. Stroke Clinical Updates
2006;16(4). http://www.stroke.org/site/DocServer/ SRR_SCU_ FINAL_forweb.pdf?docID=2501. Accessed
February 3, 2008.
- Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press; 2001.
- Institute of Medicine. The future of emergency care in the United States health system. Washington (DC): National Academies Press; 2006.
- Alberts MJ, Hademenos G, Latchaw RE, Jagoda A, Marler JR, Mayberg MR, et al.
Recommendations for the establishment of primary stroke centers.
Brain Attack Coalition. JAMA 2000;283(23):3102-9.
- Alberts MJ, Latchaw RE, Selman WR, Shephard T, Hadley MN, Brass LM, et al.
Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke 2005:36(7)1597-616.
- National Institute of Health. Improving the chain of recovery for acute stroke in your community: task force reports. Bethesda (MD): National Institute of Health; 2003. http://www.ninds.nih.gov/news_and_events/proceedings/ acute_stroke_workshop.pdf. Accessed December 22, 2004.
- Adams R, Acker J, Alberts M, Andrews L, Atkinson R, Fenelon K, et al.
Recommendations for improving the quality of care through stroke centers and systems: an examination of stroke center identification options: multidisciplinary consensus recommendations from the Advisory Working Group on Stroke Center Identification Options of the American Stroke Association. Stroke 2002;33(1):e1-7.
- Schwamm LH, Pancioli A, Acker JE 3rd, Goldstein LB, Zorowitz RD, Shephard TJ,
et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association's Task Force on the Development of Stroke Systems. Stroke 2005;36(3):690-703.
- Pancioli A, Cantwell L, Crocco T, Eckstein M, Jauch E, Larrabee H, et al. Stroke journal report 9/24/2007. Communities play critical role in emergency stroke care, panel says. Dallas (TX): American Heart Association; 2007. http://www.americanheart.org/presenter.jhtml?identifier=3050687. Accessed
February 25, 2008.
- EMS implementation guide: agenda for the future. Washington (DC): National Highway Traffic and Safety Administration; 1996. http://www.nhtsa.dot.gov/people/injury/ems/ agenda/index.html. Accessed
February 27, 2008.
- A public health action plan to prevent heart disease and stroke. Atlanta (GA): US Department of Health and Human Services, Centers for Disease Control and Prevention; 2003.
- National EMS Information System (NEMSIS) Technical Assistance Center. States and territory information. Salt Lake City (UT): Intermountain Injury Control Research Center; 2005. http://www.nemsis.org/support/stateProgressReports/index.html. Accessed
February 25, 2008.
- Mears G, Ornato JP, Dawson DE.
Emergency medical services information systems and a future EMS national database. Prehosp Emerg Care 2002;6(1):123-30.
- EMS toolkits. Chapel Hill (NC): EMS Performance Improvement Center;2007.
http://www.emspic.org/?q=node/18/ov_about.htm. Accessed February 23, 2008.
- North Carolina stroke advisory council formed: legislatively mandated council holds first meeting.
[press release]. Raleigh (NC): Public Affairs Office,
North Carolina Department of Health and Human Services; September 22, 2006. http://www.ncdhhs.gov/pressrel/9-22-06.htm. Accessed
February 23, 2008.
- EMS Performance Improvement Center. EMS System Acute Stroke Care Toolkit Draft. Chapel Hill (NC): PreHospital Medical Information System and EMS Toolkits; 2004-2008. http://www.emspic.org/documents/PDF/ TK6AcuteStrokeCareSample.pdf. Accessed
February 3, 2008.
- Suspected stroke. NCCEP protocol 30. Chapel Hill (NC): North Carolina College of Emergency Physicians
(NCCEP); 2005. http://www.nccep.org/content/ems/standards/protocols/ CombinedStroke.pdf. Accessed
February 3, 2008.
Back to top
|
|