

|

|

Volume 5:
No. 4, October 2008
SPECIAL TOPIC
Internet-Based Morbidity and Mortality Surveillance Among Hurricane Katrina Evacuees in Georgia
Susan T. Cookson, MD, MPH, Karl Soetebier, MAPW, Erin L. Murray, MSPH, Geroncio C. Fajardo, MD, MBA, MS, Randy Hanzlick, MD, Alex Cowell, Cherie Drenzek, DVM, MS
Suggested citation for this article: Cookson ST, Soetebier K, Murray EL, Fajardo GC, Hanzlick R, Cowell A, et al. Internet-based morbidity and mortality surveillance among Hurricane Katrina evacuees in Georgia. Prev Chronic Dis 2008;5(4).
http://www.cdc.gov/pcd/issues/2008/
oct/07_0239.htm. Accessed [date].
PEER REVIEWED
Abstract
Introduction
The Internet has revolutionized the way public health surveillance is conducted. Georgia has used it for notifiable disease reporting, electronic outbreak management, and early event detection. We used it in our public health response to the 125,000 Hurricane Katrina evacuees who came to Georgia.
Methods
We developed Internet-based surveillance forms for evacuation shelters and an
Internet-based death registry. District epidemiologists, hospital-based physicians, and medical examiners/coroners electronically completed the forms. We analyzed these data and data from emergency departments used by the evacuees.
Results
Shelter residents and patients who visited emergency departments reported primarily chronic diseases. Among 33 evacuee deaths, only 2 were from infectious diseases, and 1 was indirectly related to the hurricane.
Conclusion
The Internet was essential to collect health data from multiple locations, by many different people, and for multiple types of health encounters during Georgia’s Hurricane Katrina public health response.
Back to top
Introduction
Initiatives for electronic disease surveillance
The Internet has revolutionized the way government institutions function (1). As part of this revolution, in March 2001, the Centers for Disease Control and Prevention (CDC) developed the
National Electronic Disease Surveillance System initiative to provide a standard, integrated approach to notifiable disease surveillance by connecting public health to clinical information systems (2). Another CDC development has
been the Public Health Information Network (PHIN) preparedness initiative (3); 2 functional areas of this initiative are outbreak management (OM) and early event detection (EED). OM supports investigations of health events by providing a module for questionnaire development and data entry, and EED speeds the response to potential public health emergencies by collecting and analyzing prediagnostic and nonclinical disease indicator data (4).
Before these CDC initiatives were developed, the Georgia Division of Public Health (DPH) began developing its own notifiable disease system known as SendSS (State Electronic Notifiable Disease Surveillance System). As CDC standards and recommendations emerged, Georgia incorporated them into SendSS, which developed into a Web-based system that has been widely
used since 2002. SendSS uses a range of Internet technologies to collect, analyze, and manage reports of notifiable diseases
in Georgia. All district and DPH Notifiable Diseases Section/Epidemiology Branch epidemiologists and many hospitals, laboratories, and private health care providers throughout Georgia use SendSS. Because SendSS has demonstrated flexibility and technical strength and is familiar to the health care community, and because of the development and requirements of PHIN, in early 2005, DPH chose it as the foundation for Georgia’s implementation of the EED and OM modules.
Hurricane Katrina evacuees in Georgia
On August 29, 2005, Hurricane Katrina struck the Gulf Coast (5). Outside of the affected areas of Louisiana, Mississippi, and Alabama, Georgia received the second largest number of evacuees from Hurricane Katrina. The Federal Emergency Management Agency registered 47,440 evacuee households in Georgia (6). Because Mississippi and Louisiana had an average household size of 2.6
people (7), this number equates to almost 125,000 evacuees.
Within days, Georgia established 13 American Red Cross– or Salvation Army–sponsored shelters for evacuees in 11 of its 18 public health districts (Figure 1). Crowded shelters can increase the risk for communicable diseases. In addition, many evacuees had to leave needed medications behind, which increased their risk for chronic disease exacerbations. Therefore, in response to the arrival in Georgia of Hurricane Katrina evacuees, we implemented the OM and EED modules of
SendSS.
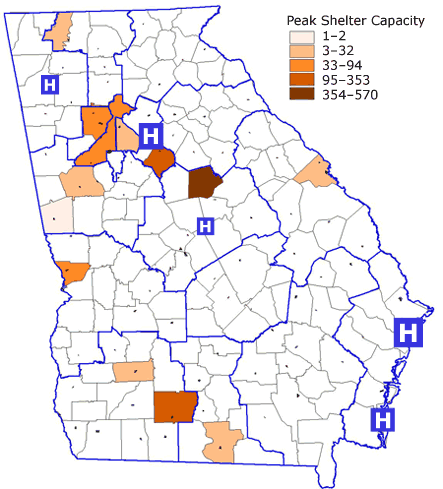
Figure 1. Locations and Occupancy of Hurricane Katrina Evacuee Shelters. Blue Line Indicates Boundaries of 18 Health Districts;
“H” Indicates Location and Relative
Number of Hospitals That Participated in Early Event Detection in Georgia, September 2005.
[A text description of this figure is also
available.]
Back to top
Methods
One day after Hurricane Katrina made landfall in Louisiana, DPH began developing 1-page forms for disease surveillance in evacuation shelters and a death registry for hospital-based physicians, medical examiners, and coroners. On September 3, these were available electronically in SendSS for all district and DPH epidemiologists to use. The disease surveillance form captured census data, symptoms of infectious diseases with outbreak potential, chronic conditions, mental health
conditions (such as overt
anxious or depressed behavior, substance or alcohol intoxication or withdrawal, or erratic behavior), injuries, and numbers of medical referrals. The district epidemiologists and other district personnel (district disease surveillance team) conducted the shelter surveillance. We calculated mean and median number of people in shelters; demographic information, such as age and sex, as percentages; and rates of conditions (cases per resident-days). The 1-page death registry, used by medical
examiners and coroners, captured demographic information, manner and cause of death, and whether the death was related to Hurricane Katrina. Direct referred to a death that was related to environmental forces of Hurricane Katrina, and indirect referred to an exacerbation
related to the hurricane of a preexisting medical condition.
We calculated simple means, medians, and percentages of characteristics among the deceased.
At that time, 7 hospital-based emergency departments in 2 health districts (East Metro-Atlanta and Coastal) participated in SendSS EED;
subsequently, 2 additional emergency departments and health districts (Macon and
Rome) provided retrospective data. We retrospectively used chief complaint,
physician diagnosis, and demographic information, including zip code of
residence before the hurricane, to characterize the Hurricane Katrina evacuees
who used any of the 9 enrolled emergency departments
for health care. We compared Louisiana and Mississippi residents — on the basis of the zip code captured by SendSS EED — who visited these emergency departments during the 8 months before (January 1 through August 28, 2005) Hurricane Katrina with those who visited during the 1 month after (August 29 through September 28, 2005). We then compared differences in the demographic characteristics and reasons for visiting the emergency department by using the z test for 2
proportions.
Back to top
Results
Shelters were opened for Hurricane Katrina evacuees on August 29, 2005,
eventually in 11 of the 18 health districts in Georgia. District epidemiologists and other public health staff conducted disease surveillance in the shelters from September 1 through 21, 2005; however, because the district epidemiologists had to return to their regular jobs after 2 weeks, the most complete data were from September 1 through 17. Epidemiologists daily entered into SendSS data from an average of 6 shelters (median 5,
range 1-10); shelters had a mean daily occupancy of 122 people (median 114, range 25-278). For those days when demographic data were available (September 3-17), the numbers of male and female evacuees were approximately equal (50.3% male and 49.7% female), and 29.5% were
aged less than 19 years. Except for adult acute chest pain, chronic disease conditions and mental health problems were reported at least as frequently as infectious disease symptoms
(Table 1). The district epidemiologist
detected only 1 confirmed outbreak of norovirus (Figure 2).
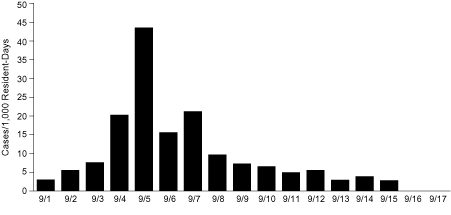
Figure 2. Rate of Diarrhea or Vomiting Among Hurricane Katrina Evacuees in Georgia Shelters, September 1-17, 2005. An Outbreak of Norovirus Was Detected in 1 Shelter on September 5 (75% of Specimens Were Positive for Norovirus). The Overall Rate of Diarrhea/Vomiting for the Period
Was 9.35 cases per 1,000 Resident-Days.
[A tabular version of this figure is also
available.]
Georgia medical examiners and coroners entered into the death
registry 33 deaths among Hurricane Katrina evacuees from 7 different counties in Metro-Atlanta and
Southwest and Coastal Georgia.
These deaths occurred an average of 33 days (median 31, range 0-113 days) after August 29, 2005. The average age of the deceased was 61 years (median 66, range 0-89 years), 42.3% were female, and 91% were from Louisiana, of whom 77.3% were from New Orleans. Deaths were mainly from natural causes
(90.9%); however, 1 person each died from homicide, suicide (self-inflicted gunshot wound), and accident (fall resulting in subdural hematoma). The causes of death were noninfectious except in 2 people who were septic
(Table 2). Most (78.8%) evacuees died in a hospital. No deaths were registered as directly related to the hurricane; only 1 death was coded as indirectly related to the hurricane because of preexisting cerebrovascular disease.
Of Louisiana and Mississippi residents who visited participating Georgia emergency departments, 174 visited during the 8 months before and 151 visited during the 1 month after Hurricane Katrina. This number represented a 7-fold increase in monthly visits, but patients’ age, sex, and racial distribution did not differ between the 2 periods. Of the evacuees, those from Louisiana were more likely to visit Atlanta emergency departments (72.4%) than
emergency departments in the other 3 health districts (Coastal,
Macon, and Rome) combined (P ≤ .01). Mississippi residents (40%) were more likely to go to the Coastal district than were Louisiana residents (22%, P = .03). Only cardiopulmonary complaints significantly increased (P = .03) after Hurricane Katrina; nonsignificant increases were seen with medication refill requests and complaints of rash/skin infection
(Table 3).
Back to top
Discussion
Natural disasters require a rapid public health response to minimize the devastating effects that these events can have on the health infrastructure and the health of affected people. Because so many Hurricane Katrina evacuees came to Georgia and could not return home, we realized the need for public health surveillance at multiple levels: conducting disease surveillance in shelters, assessing evacuees’ use of the health care system, and documenting any deaths.
Traditionally, public health response during a natural disaster focuses on
preventing communicable disease epidemics (8). However, public health
authorities are increasingly aware that people with chronic diseases have
special needs during such an event (9,10). This was the case in Georgia
shelters, where most of the conditions that required medical referrals were
chronic diseases, such as hypertension and diabetes. In addition, only
cardiopulmonary complaints increased significantly after the hurricane as
reasons for visiting the emergency department.
The shelter disease surveillance identified only 1 infectious disease outbreak of norovirus. During the same time, epidemiologists identified a much larger norovirus outbreak in multiple shelters in Houston, Texas (11). In spite of concerns about the potential for outbreaks, most conditions identified inside and outside the hurricane-affected areas were chronic diseases (12), and rates of hypertension and diabetes among evacuees (13) in Louisiana
shelters were comparable to those we observed in
Georgia.
Limitations of the shelter surveillance data are that epidemiologists could not enter all data every day and
that only shelters sponsored by the American Red Cross or Salvation Army were included; however, nonsponsored shelters were probably smaller than these were, so the potential for infectious disease outbreaks was probably lower. We similarly could not assess chronic conditions and need for medical care referrals in nonsponsored shelters. The EED data are limited because of the location and
number of emergency departments we were able to survey and the retrospective nature of the analysis. As of the 2008 hurricane season, 30 emergency departments in 14 of the 18 health districts are participating in EED, and we are prepared to examine EED data as we receive it to assess needs among hurricane evacuees who access health care from all participating emergency departments.
Because evacuees were distributed throughout Georgia — as seen by the locations of shelters (11 of the 18 health districts), emergency departments used
(Figure 1), and deaths reported — the state’s Internet-based SendSS platform was essential to collect health data from multiple locations, by many different people, and for multiple types of health encounters. Georgia already had OM and EED
modules in SendSS.
The SendSS OM module has a dynamic survey capacity that allowed for different forms, from disease surveillance in shelters for public health epidemiologists to death registry for medical examiners and coroners. In addition, the import/export feature enabled epidemiologists and physicians throughout Georgia to enter data and
enabled us to analyze the data collected in a timely manner. In future disasters, we will prospectively track evacuees who visit emergency departments by using the
zip codes of where the disaster occurred; doing so will increase our knowledge of health care utilization patterns and medical needs. Use of the Internet-based SendSS system simplified the rapid and systematic collection, analysis, and interpretation of surveillance data from shelters, hospitals, and medical examiners/coroners
in Georgia. Collaboration facilitated by SendSS was valuable, and we will use
SendSS during future public health emergencies that require the collection and analysis of
data from various locations and venues.
Finally, the Internet can revolutionize the way public health professionals respond to a disaster. Our district epidemiologists, medical examiners, and coroners demonstrated the utility of the Internet-based SendSS system during the Hurricane Katrina emergency response in Georgia. DPH understood the need for minimal data elements and used only a 1-page form. CDC has developed and deployed the Rapid Data Collector (RDC), a secure, Web-based system, similar in focus to the system used in
Georgia, which is available for all state and local health departments. (For instructions on how to register and use RDC, call Michael Miller at 770-488-7542 or
send e-mail to mjmiller@cdc.gov.) With RDC, the user can create an electronic survey, deploy it on personal digital assistants, and rapidly collect electronic data. After collection, data are uploaded to a central, Web-accessible database that facilitates their management, analysis, and distribution. As an example of its use, CDC recommends that
officials involved in disaster response use RDC to electronically capture and transmit disaster-related mortality data (14). Although other states may not have the same capacity as Georgia to use a dynamic survey in an electronic notifiable disease surveillance system, all states have access to the CDC RDC. Therefore, all states can use this electronic tool to better monitor and protect the health of the populations they serve, especially in the context of a disaster or other public health
emergency.
Back to top
Acknowledgments
We thank the members of the district disease surveillance team, including
students from Rollins School of Public Health — Silvia Arrue, Sara Burghardt, Joyce Casper, Debra Crowley, Kristin Cunningham, Helen Ellis, Jennifer Emalianchik, Susan Frankenberg, Sheritta Frazier, Tracy Gilmer, German Gonzalez, Keri Griffin, Jacqueline Jenkins, Kim Kennedy, Annette Neu, Mary Patrick, Quyen Phan, Marcia Rodriguez, Jonathan Spangler, Nancy Sprauve, Larry Staton, Danielle Thomas, Eileen Usman, Amanda Walpole, Crystal Witherspoon, and Joy Wells —
for tireless efforts to ensure the best possible public health response for the
people who came to Georgia to flee the devastation of Hurricane Katrina.
Back to top
Author Information
Corresponding Author: Susan T. Cookson, MD, MPH, Centers for Disease Control and Prevention, 1600 Clifton Rd, MS E97, Atlanta, GA 30333. Telephone: 404-498-0338. E-mail:
scookson@cdc.gov. Dr Cookson is also
affiliated with the Georgia Division of Public Health.
Author Affiliations: Karl Soetebier, Erin L. Murray, Geroncio C. Fajardo, Alex Cowell, Cherie Drenzek, Georgia Division of Public Health,
Atlanta, Georgia; Geroncio C. Fajardo, Randy Hanzlick,
Fulton County Medical Examiner’s Office, Atlanta, Georgia.
Back to top
References
- Wilcox LS. Revolution. Prev Chronic Dis 2004;1(4).
http://www.cdc.gov/pcd/issues/2004/oct/04_0092.htm. Accessed March 27,
2007.
- Description of the NEDSS base system, March 28, 2001. Atlanta (GA):
Centers for Disease Control and Prevention. http://www.cdc.gov/nedss/BaseSystem/NEDSSBaseSysDescription.pdf.
Accessed March 26, 2007.
- PHIN: preparedness. Atlanta (GA): Centers for Disease Control and
Prevention. http://www.cdc.gov/phin/about.html. Accessed June 3, 2008.
- Sosin DM.
Syndromic surveillance: a case for skillful investment. Biosecur Bioterror 2003;1(4):247-53.
- Hurricane Katrina forecast timeline. Washington (DC): National Oceanic and
Atmospheric Administration. http://commerce.senate.gov/pdf/Katrina_NOAA_Timeline.pdf.
Accessed May 22, 2006.
- City of Atlanta’s Hurricane Katrina relief efforts. Atlanta (GA): City of
Atlanta. http://www.atlantaga.gov/mayor/katrinarelief_091505.aspx. Accessed April 3,
2007.
- U.S. Census 2000. Washington (DC): U.S. Census Bureau. http://www.census.gov/main/www/cen2000.html. Accessed May 10,
2006.
- Waring SC, Brown BJ.
The threat of communicable diseases following natural disasters: a public health response. Disaster Manag Response 2005;3(2):41-7.
- Weir E.
Hurricanes: lessons from Charley and the gang. CMAJ 2005;173(6):597.
- Ford ES, Mokdad AH, Link MW, Garvin WS, McGuire LC, Jiles RB, et al.
Chronic disease in health emergencies: in the eye of the hurricane. Prev Chronic Dis
2006;3(2).
http://www.cdc.gov/pcd/issues/2006/apr/05_0235.htm. Accessed March 27,
2007.
- Centers for Disease Control and Prevention.
Norovirus outbreak among evacuees from Hurricane Katrina — Houston, Texas, September 2005. MMWR Morb Mortal Wkly Rep 2005;54(40):1016-8.
- Centers for Disease Control and Prevention.
Illness surveillance and rapid needs assessment among Hurricane Katrina evacuees — Colorado, September 1-23, 2005. MMWR Morb Mortal Wkly Rep 2006;55(9):244-7.
- Centers for Disease Control and Prevention.
Surveillance in hurricane evacuation centers — Louisiana, September-October 2005. MMWR Morb Mortal Wkly Rep 2006;55(2):32-5.
- Natural disaster surveillance resources. Atlanta (GA): Centers for Disease
Control and Prevention. http://www.bt.cdc.gov/disasters/surveillance/resources.asp.
Accessed July 20, 2007.
Back to top
|
|
