

|

|

Volume
2:
No. 1, January 2005
COMMUNITY CASE STUDY
Diabetes Is a Community Issue: The Critical Elements of
a Successful Outreach and Education Model on the U.S.-Mexico Border
Maia Ingram, MPH, Gwen Gallegos, MS, JoJean Elenes
Suggested citation for this article: Ingram M, Gallegos G, Elenes J.
Diabetes is a community issue: the critical elements of a successful outreach
and education model on the U.S.-Mexico border. Prev Chronic Dis [serial
online] 2005 Jan [date cited]. Available from: URL:
http://www.cdc.gov/pcd/issues/2005/
jan/04_0078.htm.
PEER REVIEWED
Abstract
Background
Diabetes is reaching epidemic proportions on the U.S.-Mexico Border, and
culturally competent diabetes education is not available in many
communities.
Context
People with diabetes often do not have access to regular
medical care, cannot afford medication, and lack the community
infrastructure that supports self-management practices. Self-management
education and support have great
potential to impact diabetes control in this environment.
Methods
To address this need, partners of the Border Health Strategic Initiative (Border Health ¡SI!) collaboratively developed a
culturally relevant diabetes outreach and education program. The model
included a five-week series of free diabetes education classes that
assisted participants in gaining the knowledge and skills necessary to be
physically active, control diet, monitor blood sugar, take medications, and be
aware of complications. Central to the model was the use of community health
workers — or promotores de salud — to conduct outreach, participate in
patient education, and provide individual support.
Consequences
Program participants
achieved significant improvements in self-management behaviors and HbA1c,
random blood glucose, and blood pressure levels.
Interpretation
Quantitative and qualitative
evaluation helped to identify the essential elements of a successful program,
including partnership of providers, community diabetes classes, promotores
outreach and support, linkage between diabetes education and clinical care,
and program evaluation.
Back to top
Background
The impact of diabetes is devastating along the U.S.-Mexico Border. The
rate of diabetes mortality in the border region is nearly 50% higher than in
the rest of the country (1), and Hispanics are two to three times more likely
to suffer from serious secondary complications (2,3). Self-management
behaviors, such as diet, physical activity, and glucose self-monitoring are
fundamental to avoiding the long-term complications of diabetes (4). For many
individuals, however, self-management behaviors constitute drastic lifestyle
changes for which there is little external support. In a managed-care setting,
Hispanics were shown to exhibit poor diabetes control when compared with
non-Hispanic whites (5).
Diabetes education can have a positive impact on self-management behaviors
and glycemic control, particularly when accompanied by intensive follow-up
support (6). Diabetes classes delivered in a community setting have been shown
to be effective in achieving glycemic control among adults with type 2
diabetes, and this mode of delivery is likely to increase the cultural
relevancy and appropriateness of educational techniques in addition to providing
greater access to hard-to-reach populations (7). Community
partnerships also have the potential to enhance cultural relevance and
positively impact self-management and clinical outcomes (8).
There are overwhelming challenges to providing formal diabetes education in
border communities. Individuals without insurance do not have access to
diabetes education services. For individuals with insurance, few certified
diabetes educators (CDEs) live and work in border communities and they may
not speak Spanish. Programs that provide interpretation or translation are
often not culturally relevant to Hispanics.
This paper describes the patient component of the Border Health Strategic
Initiative (Border Health ¡SI!) funded by the Centers for Disease
Control and Prevention (CDC), which used the community health worker model to provide culturally competent diabetes education
in two Arizona border communities in Yuma and Santa Cruz counties. A detailed
description of Border Health ¡SI! is included in this issue of
Preventing Chronic Disease (9) along with several companion papers
addressing other components of the model (10-18). More information on
the rationale and effectiveness of the community health worker model in
addressing diabetes can be found in the CDC Division of Diabetes Translation’s
position statement (available from
http://www.cdc.gov/diabetes/projects/comm.htm).
Back to top
Context
Individual ability to manage diabetes cannot be separated from community
context and support for diabetes care (19). Both Yuma and Santa Cruz Counties
are rural and more than 90% Hispanic; Yuma County has a large migrant/farmworker
community. The region is medically underserved. Lack of insurance, seasonal
employment of farmworkers, and fear and discrimination related to immigration
present challenges to establishing a regular source of care (20). Patients
with diabetes often cross the border to Mexico for medical care, making it
difficult to maintain continuity of care.
Residents not eligible for Medicaid programs can rarely afford diabetes
medication. Individuals with insurance often do not have pharmaceutical
coverage and must decide whether to buy food or medicine. Patients share
medication or resort to taking it only when they are feeling badly. While
diabetes programs may make glucose monitors available, few resources cover the
cost of glucose-monitoring strips.
The border environment does not support good nutrition and physical
activity. Few recreational areas, parks, or sidewalks exist in these rural
areas to facilitate walking. Summer heat, inadequate lighting, dangerous
walking surfaces, and wild dogs pose additional challenges. Although southern
Yuma County is a farming community, and the city of Nogales (in
Santa Cruz County) is a throughway for produce from Mexico, healthy foods such
as fresh fruits and vegetables are high-priced and often unavailable.
Furthermore, the health messages taken for granted in urban areas rarely reach farmworkers who work 12-hour days in isolated areas.
The social network that can potentially support self-management is often
not in place. The elderly may have family members who migrate to follow the
harvesting season or move to urban areas. Many extended family members live in
Mexico. Diabetes patients may become isolated and depressed as they experience
increasing health problems.
Because of these barriers, education programs must be culturally competent.
Vital to the diabetes education program was the use of promotores de salud.
Promotores are indigenous to the communities in which they work and
provide a bridge between the health care delivery system and the community. In
addition to health information, they provide social support and advocate for
patients to gain access to health and social services (21). In one diabetes
education program, the use of promotores in a Hispanic community was
shown to increase the rate of completion (22).
The program
The diabetes outreach and education program was created in Santa Cruz
County under a Health Resources and Services Administration Rural Health
Outreach Grant (RHOG) in 1997 and adapted by the Yuma community in 2000 under
its own RHOG. The programs were supported logistically under the comprehensive
framework of Border Health ¡SI! over a three-year period, although Yuma
County had additional resources. An investigation of both programs allowed us
to define the essential elements of the outreach and education model, which
are described below and illustrated conceptually (Figure).
Partnership
of providers. Both the Yuma and Santa Cruz programs relied upon a
consortium of community providers to implement the patient education
component. The community health centers (CHCs) administered the programs and
provided a program coordinator. Both programs involved first-time
collaboration between the health center and local hospital. The hospital in
each county provided a CDE to facilitate classes, train promotoras in
diabetes care, and work individually with participants. In Yuma, a grassroots
farmworker advocacy organization provided the promotoras, while in
Santa Cruz, the promotoras were provided by the CHC. Each program had
an academic partner who provided evaluation and technical assistance. The
collaborative aspect of the program was crucial in building broader community
support for diabetes care.
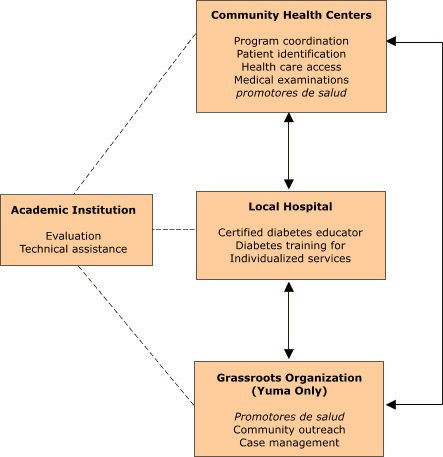
Figure.
The roles and responsibilities of partners in the diabetes outreach and
education program, Border Health ¡SI!, Yuma and Santa Cruz
counties, Arizona.
Promotores de salud are community health workers.
Community diabetes classes. Very few participants had prior
diabetes education, although many had had diabetes for years. The programs
used a culturally competent curriculum that employed a variety of teaching
methods to educate participants on how diabetes affects the body and how
self-management controls the disease. The curriculum was developed prior to
the initiation of the programs by the CDE working in Santa Cruz County using
the American Diabetes Association (ADA) Standards of Care. The curriculum
followed the content areas set by the ADA and adapted them to the border
communities. The curriculum included five two-hour classes held once a week
over a five-week period. The sessions included the following topics: 1)
understanding diabetes; 2) meal planning; 3) monitoring, medications, and
movement; 4) avoiding complications and maintaining health; and 5) foot/eye
clinics. In both sites, participants were encouraged to bring family members.
The class formats included presentation and discussion and used
handouts, videos, and other teaching aids, such as food models. Participants engaged in activities such as creating a
balanced plate of food to achieve dietary goals and dancing to achieve
physical activity goals. Each class began with a review of the previous
session. In addition, program staff measured blood glucose, weight, and blood
pressure at each class to demonstrate to participants the progress they were
making over the course of the program.
In Santa Cruz, a bicultural CDE based in the local hospital taught the
classes. In Yuma, classes were taught by a health educator and eventually by
the promotoras under the supervision of a non-Spanish–speaking CDE
located in the hospital. Class structure varied between communities. The
Santa Cruz community embraced the importance of an open-door program so that
classes were available on a rotating basis and class size was maintained at
about 20 participants. Participants attended them in any sequence and as often
as they wished. In Yuma, the partners recruited a group for each round of
classes and encouraged them to complete the program during this time period.
Growing interest in the Yuma program resulted in class sizes of up to 40
people.
Promotores outreach and support. The role of the promotoras
was to provide outreach, assist participants in incorporating self-management
behaviors into their lifestyles, and offer ongoing support and follow-up.
There was some disparity in resources between the two programs, and the Yuma
community had the advantage of being able to fully implement the promotora
model. Four promotoras took responsibility for recruitment, support,
and follow-up for a caseload of participants. Potential participants were
identified through the health center database. The promotoras
personally invited potential participants to the program, provided support to
the learning process both during and outside of the classes, and followed up
with participants for a six-month period following completion of the classes.
The promotoras assisted patients in accessing health insurance,
medications, and other social services.
In Santa Cruz, one promotora was available on the day of class to
provide telephone follow-up. However, because this program had been initiated
several years prior to the initiation of the Border Health ¡SI! patient
education component, local providers were aware of the benefits of the program
and regularly referred their patients to the classes.
Linkage between diabetes education and clinical care. In both
communities, the program was based in a CHC, increasing opportunities for
patient-provider communication on patient care. During the program, providers
in both programs increased referrals as they recognized the benefits of
patient participation. In Santa Cruz, the program added a patient diabetes
“empowerment card” to track clinical care and increase patient-provider
communication. The trifold card included a form to track the last five
physician visits, current medications, participation in diabetes classes, and
personal goals.
Many participants did not have access to regular care, and many could not
recall a past eye examination. The programs assisted participants in
identifying insurance options. A foot exam was included in both programs, and
in Yuma, ophthalmologists volunteered their time for eye clinics on Saturdays.
Regardless of insurance status, many participants could not afford
medication. While program resources to provide medication were not available,
participants were linked to insurance or special programs when possible. Both
programs accessed samples from pharmaceutical companies.
Program Evaluation. Program partners engaged in a
participatory model of evaluation under the guidance of the academic
institution. Under the participatory model, all stakeholders are involved in
each phase of evaluation, ensuring a continuous exchange of knowledge, skills,
and resources (23). Partners collaboratively developed quantitative and
qualitative instruments and shared responsibility for data collection. The
academic partner was responsible for analyzing and compiling program data on a
cyclical basis to allow for integration of program findings over time.
Evaluation efforts were hindered, however, by a lack of resources, which
resulted in gaps in data and at times forced promotoras to choose
between serving clients (always the first priority) and collecting evaluation
information.
Self-management practices were assessed through pre- and follow-up questionnaires administered
by the promotoras prior to initiation in the program and six months
after graduation. The academic partners trained promotoras
in administering
the questionnaire, which asked participants if they engaged in self-management
practices, including diet, physical activity, foot care, and regular
glucose monitoring. The questionnaire also asked participants about their most
recent visit with their doctor and whether they had received diabetes health
exams in the past year. The initial questionnaire included information on
demographics and health history.
Health outcomes included random blood glucose, blood pressure, weight, and
HbA1c. Program staff took measurements at three points: initiation of classes, upon
graduation from the program, and six months afterwards. HbA1c was measured
only twice: before classes and at six-month follow up. In Yuma, the data set
is much more complete than in Santa Cruz, and all post-measures were made six
to 12 weeks after participants entered the program. In Santa Cruz,
the timing of post-measures varied because participants graduated at different points, and attempts to collect HbA1c data
at follow-up were unsuccessful because of a lack of staff and financial resources.
Qualitative evaluation took place in Yuma and consisted of in-depth
interviews with a random sample of participants in the second and third years
of the program. Program partners developed the questionnaire, and academic
partners who were not engaged in service delivery conducted the interviews.
The interviews explored perceptions of diabetes before and after the program,
the role of the family in self-management, changes in self-management
practices, and ongoing barriers to diabetes control.
Back to top
Consequences
The process of implementing the Border Health ¡SI! patient education
component over three years in two communities provided a rich opportunity to
learn from successes and challenges. In spite of diminishing resources, both
programs maintained a strong commitment to providing diabetes education to the
underserved. Both communities expressed increased demand for the classes,
which was difficult to manage in Yuma because the program moved one group of
participants through one series of classes before starting another. At times,
classes in Yuma had more than 40 people. Santa Cruz began offering classes in
the evening to respond to those who worked during the day.
Santa Cruz had the advantage of a CDE who had worked in the community for
years. The Yuma health educator left halfway through the program. The
promotores then took responsibility for teaching the classes under the
supervision of the hospital CDE. Participant outcomes were maintained when the
promotores began teaching.
Evaluation results
Evaluation results generated by the Border Health ¡SI! patient
education component are extensive; this paper attempts only to highlight key
findings. Table 1 describes the characteristics of individuals who enrolled in
the diabetes education classes. In Yuma, 376 individuals enrolled in classes
and 306 (81%) graduated. Of graduates, 243 (79%) were reached for the follow-up
interview.
In Santa Cruz, 406 people enrolled in classes, and 135 (33%) graduated. Of
graduates, 40 (30%) were reached for follow-up. Demographic information
revealed that the programs did reach the targeted populations. In both
counties, participants were more likely to be female and older than 50 years. The
majority did not graduate from high school, and approximately two thirds had
family members with diabetes. In Yuma, participants were slightly older and
experienced more diabetes-related illness; however, they had better access to
insurance through Medicare. Few participants had received prior diabetes
education, and many had never had an eye exam. Approximately one half reported
having high blood pressure and, in Yuma, 59% experienced numbness and burning in
their feet.
Health outcomes
Health measures were taken pre- and post-class and at six-month
follow-up. Paired t-tests performed on pre- and post-data revealed a
significant decrease in the average random blood glucose measurement among
participants in both programs (Table 2). In Yuma, levels dropped from 224 mg/dL
to 201 mg/dL, and, in Santa Cruz, levels dropped from 197 mg/dL to 151 mg/dL.
Both programs also achieved modest but significant decreases in diastolic
blood pressure among all participants. Among high-risk participants in Yuma,
systolic blood pressure fell from 151 mg/dL to 137 mg/dL, and
diastolic blood pressure fell from 100 mg/dL to 84 mg/dL. Among-high risk
participants in Santa Cruz, systolic blood pressure fell from 153
mg/dL to 139 mg/dL, and diastolic blood pressure fell from 102 mg/dL to 91 mg/dL.
There were no significant changes in health outcomes at the six-month
follow-up measure. In Yuma, follow-up results demonstrated a significant 0.7
decrease in HbA1c from 9.4 to 8.7 among those who initiated the program with
HbA1c >6.9.
Self-management outcomes
Self-management practices were evaluated in the six-month follow-up
interview. Paired t-tests were used to determine significant
changes in self-management behaviors. As seen in
Table 3, a significant
proportion of participants in both counties reported increasing
self-management behaviors, including diet, foot care, and glucose monitoring.
In Santa Cruz, the percentage of individuals following a diabetes diet
increased significantly. In Yuma, where HbA1c and eye exams were provided as
part of the Border Health ¡SI! patient education component, the
percentage of individuals who had ever received these examinations increased
significantly from 53% to 96% (HbA1c) and 57% to 91% (eye exam).
In-depth interviews
Quality of life is as important as clinical outcomes, and in-depth
interviews in Yuma demonstrated the impact of the program on program
participants. Participant attitude toward diabetes changed from ignorance and
fear to acceptance and control, which seemed pivotal in improving their
emotional well-being, regardless of self-management practices. Comments
included:
- “I take care of myself better. I know what is bad for me. I don’t feel
angry now.”
- “They tell you how to care for yourself. You can adapt and live a normal
life.”
The promotoras were also vital to the process because participants
felt that the promotoras cared for them and were willing to do whatever
they could to help them.
- “They are concerned about me. I am motivated because they are worried
about me and helped me. ”
- “My promotora is marvelous. I have a
thousand good things to say about her.”
Both programs used findings to pursue and secure additional funding to
sustain services.
Back to top
Interpretation
This program responded to a need for accessible, culturally competent
diabetes education and demonstrated how communities can galvanize local
capacity to respond to an overwhelming lack of resources. Local providers
contributed free eye and foot exams and promotoras took over the
diabetes education classes when the health educator left the community.
Partnership of providers. Crucial to success was the partnership of
diverse organizations that enabled the programs to confront challenges of the
border environment on multiple levels. The CHCs had access to the target
population, but they would not have been able to recruit and retain
participants without the promotores. In both communities, the hospital
was critical in providing expertise and in accessing resources.
Community diabetes classes. Holding classes at a community site in a
series with a specific group of participants appears to contribute to program
completion.
This may be because participants have a greater sense of commitment and enjoy
belonging to a group. Santa Cruz was extremely fortunate to have a committed,
culturally competent and expert CDE. In rural communities where CDEs are not
available, promotoras can be trained to provide diabetes education. It
is vital, however, that they have backup and support from a qualified person.
Promotores outreach and support. Program outcomes would not have
been achieved without promotores.
Promotores are fundamental in
ensuring that participants initiate and complete classes, gain access to
resources, and adopt self-management practices.
Linkage between diabetes education and clinical care. Providing
access to health care, examinations, and medications is a challenge that
should be addressed early on. For this reason alone, community collaboration
is essential. Creating formal relationships with clinical providers may
enhance health outcomes. The patient empowerment card was one attempt to
establish a formal relationship, and the card was popular with program
participants. Strategies to ensure that providers use the card need to be
implemented and the impact on care needs to be evaluated.
Program evaluation. Conducting meaningful program evaluation —
especially with limited resources — was a challenging but key element of the
patient education component. Consistent with the participatory model of
evaluation, the academic partner was not an outsider to but rather an integral
member of the team and a stakeholder in its success. Within this framework,
evaluation became a tool of program development, encouraging partners to
define concretely the desired outcomes of the program, to make the effort to
collect the necessary information, and to integrate feedback into program
strategies. The influence of evaluation on Border Health ¡SI! included
1) designing a series of diabetes education classes (rather than an
open-door policy) to create group cohesion and support, 2) establishing a
greater focus on including family members in the education and care process,
and 3) developing strategies to increase patient-provider communication. Both
Border Health ¡SI! communities used evaluation results to sustain
program activities beyond the funding period, one through institutional
support and the other through other grant funding.
In these two marginalized border communities, the Border Health ¡SI!
diabetes education and outreach program had a positive influence on the
ability of individuals to adopt self-management practices and improve health
outcomes. It is important to note that as a component of the comprehensive
Border Health ¡SI!, the education and outreach program was linked to a
policy action group that addressed challenging environmental issues related to
diabetes (15,16). Participation in a policy-focused group enabled program
partners and community leaders to discuss systemic problems, leverage
additional resources, and address prevention on a community level.
Back to top
Acknowledgments
The authors thank Sunset Community Health Center, Mariposa Community Health
Center, and Carondelet Health Network.
Back to top
Author Information
Corresponding author: Maia Ingram, MPH, Mel and Enid Zuckerman Arizona
College of Public Health, 2501 E Elm, PO Box 24177, Tucson AZ 85721.
Telephone: 520-626-7946, ext 242. E-mail:
maiai@u.arizona.edu.
Author affiliations: Gwen Gallegos, MS, Carondelet Health Network, Holy
Cross Hospital, Nogales, Ariz; JoJean Elenes, Mariposa Community Health
Center, Nogales, Ariz.
Back to top
References
- American Diabetes Association. Diabetes vital statistics.
Alexandra (VA): American Diabetes Association; 1996.
- Haffner SM, Fong D, Stern MP, Pugh JA, Hazuda HP, Patterson JK, et
al.
Diabetic retinopathy in Mexican Americans and non-Hispanic Whites. Diabetes 1988; 37:878-84.
- Hanis CL, Ferrell RE, Barton SA,
Aguilar L, Garza-Ibarra A, Tulloch BR, et
al.
Diabetes among Mexican Americans in Starr County, Texas. Am J Epidemiol
1983;118:659-72.
- Diabetes Control and Complications Trial Research Group.
The effect
of intensive treatment of diabetes on the development and progression of
long-term complications in insulin-dependent diabetes mellitus. N Engl J
Med 1993; 329:977–86.
- Brown AF, Gerzoff RB, Karter AJ, Gregg E, Safford M, Waitzfelder B, et al.
Health behaviors and quality of care among
Latinos with diabetes in managed care. Am J Public Health 2003;93(10):1694-8.
- Norris SL, Engelgau MM, Narayan KM.
Effectiveness of self-management training in type 2
diabetes: a systematic review of randomized controlled trials. Diabetes Care
2001 Mar;24(3):561-87.
- Norris SL, Nichols PJ, Caspersen CJ,
Glasgow RE, Engelgau MM, Jack L, et al.
Increasing diabetes self-management education in community
settings: a systematic review. Am J Prev Med 2002 May;22(4 Suppl):39-66.
- Gerber JC, Stewart DL.
Prevention and control of hypertension and
diabetes in an underserved population through community outreach and disease
management: a plan of action. J Assoc Acad
Minor Phys 1998;(3):48-52.
- Cohen SJ, Ingram M. Border heath
strategic initiative: overview and introduction to a community-based model
for diabetes prevention and control. Prev Chronic Dis [serial online] 2005 Jan [2004 Dec 15].
- Abarca J, Ramachandran S.
Using community indicators to assess nutrition in Arizona-Mexico border
communities. Prev Chronic Dis [serial online]
2005 Jan [2004
Dec 15].
- Schacter KA, Cohen SJ.
From research to practice: challenges in implementing national diabetes
guidelines with five community health centers on the border. Prev
Chronic Dis [serial online] 2005 Jan [2004 Dec 15].
-
Teufel-Shone NI, Drummond R, Rawiel U.
Developing and adapting a family-based diabetes program at the U.S.-Mexico
border. Prev Chronic Dis [serial online] 2005 Jan [2004 Dec
15].
- Staten LK, Scheu LL, Bronson D, Peña V, Elenes J.
Pasos adelante:
the effectiveness of a community-based chronic disease prevention program.
Prev Chronic Dis [serial online] 2005 Jan [2004 Dec 15].
- Staten LK, Teufel-Shone NI, Steinfelt VE, Sanchez N, Halverson K, Flores
C, et al. The
School Health Index as an impetus for policy change. Prev Chronic Dis
[serial online] 2005 Jan [2004 Dec 15].
- Meister JS, de Zapien JG.
Bringing health policy issues front and center in the community: expanding
the role of community health coalitions. Prev Chronic Dis [serial
online] 2005 Jan [2004 Dec 15].
- Steinfelt VE.
The Border Health Strategic Initiative from a community perspective.
Prev Chronic Dis [serial online] 2005 Jan [2005 Dec 15].
- Rodríguez-Saldaña J.
Challenges and
opportunities in border health. Prev Chronic Dis [serial online] 2005 Jan [2005 Dec 15].
- Martorell R.
Diabetes and Mexicans: why the two are linked. Prev Chronic Dis [serial
online] 2005 Jan [2005 Dec 15].
- U.S. Department of Health and Human Services.
Healthy People 2010: understanding and improving health. 2nd ed.
Washington (DC): U.S. Government Printing Office; 2000 Nov.
- Ruiz-Beltran M, Kamau JK.
The socio-economic and cultural
impediments to well-being along the US-Mexico border. J Cmty Hlth 2001;26(2):123-32.
- Love MB, Gardner K, Legion V.
Community
health
workers: who they are and what they do. Health Educ Behav 1997;24:510-22.
- Corkery E, Palmer C, Foley ME,
Schechter CB, Frisher L, Roman SH.
Effects of a bicultural community health worker on completion of diabetes
education in a Hispanic population. Diabetes Care 1997;20(3):254-7.
- Springett J. Issues in participatory evaluation.
In: Minkler M, Wallerstein N, editors. Community-based participatory
research for health. Hoboken (NJ): John Wiley & Sons, Inc; 2002
Nov. p. 268-88.
Back to top
|
|
