 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Varicella Outbreak Among Primary School Students --- Beijing, China, 2004Huilai Ma,1 R. Fontaine2
Corresponding author: Huilai Ma, Chinese Field Epidemiology Training Program, Chinese Center for Disease Control and Prevention, 27 Nanwei Road, Beijing, China, 100050. Telephone: 86-10-63022556; Fax: 86-10-83171509; E-mail: huilaima@sohu.com. Disclosure of relationship: The contributors of this report have disclosed that they have no financial interest, relationship, affiliation, or other association with any organization that might represent a conflict of interest. In addition, this report does not contain any discussion of unlabeled use of commercial products or products for investigational use. AbstractIntroduction: On June 9, 2004, a varicella outbreak was reported in a Beijing primary school affecting approximately 80% of children in one preschool classroom. An outbreak investigation was initiated to identify factors contributing to the high rate of transmission and to assess the effectiveness of control measures. Methods: A varicella case was defined as onset of a generalized, vesicular pruritic rash lasting >4 days in a student at the school during January 1--June 26, 2004. Parents of all students in the four lowest grades (K--2) were questioned concerning varicella illness before January 1, 2004. Exposure and vaccination histories of 111 ill students and 120 control students with no history of varicella were compared. Results: During January 1--June 26, 2004, of 1,407 students, 138 (9.8%) had varicella; 488 (35%) K--2 students had no history of varicella before the outbreak. In five classrooms in which attack rates (ARs) were high (>40%), a primary-case student had remained in school 2 days while ill with a rash. The secondary attack rate (SAR) in these classrooms was 21%, compared with 1.7% in classrooms in which the first ill student was sent home immediately (risk ratio [RR] = 10; 95% confidence interval [CI] = 3.7--29.0). A total of 111 (70%) ill students rode the school bus daily, compared with 120 (33%) control students (odds ratio [OR] =4.9; CI = 2.7--9.0). A total of 73 (33%) ill students had a history of varicella vaccination before January 1, 2004, compared with 32 (69%) control-students (OR = 0.22; CI = 0.08--0.59). Conclusion: Students who were not excluded from school on the first day of rash were key contributors to the spread of varicella in their classrooms. High susceptibility to varicella at school entry indicates that vaccination of susceptible students might be the only effective measure to control this recurrent problem. IntroductionVaricella has been a nearly universal disease of childhood. In temperate climates, nearly 90% of children had varicella by age 15 years before vaccine became available (1). Before 1995, when vaccine was licensed, an estimated 4 million cases of varicella occurred each year in the United States; approximately 100 patients died and 10,000 persons were hospitalized annually because of varicella and related complications (2). Because varicella is not a notifiable disease in China, statistics concerning hospitalization and death attributable to varicella are not available. However, since January 1, 2004, varicella outbreaks have been reported to the public health emergency reporting system. During January--June 2004, a total of 64 varicella outbreaks were reported, accounting for 20% of all communicable disease outbreaks reported in China; 58 (91%) varicella outbreaks occurred in schools. Varicella vaccine has been available commercially since 2003, but China has no programs to support routine varicella vaccination. On June 9, the Chinese Center for Disease Control and Prevention (China CDC) was notified of a varicella outbreak in a primary school in a suburb of Beijing, affecting approximately 80% of children in certain classes. Since the school opened in 1999, varicella outbreaks have disrupted activities every year, despite a school policy to isolate students with a rash at home for 7 days. An outbreak investigation was initiated to identify factors contributing to the high rate of transmission and assess the effectiveness of control measures. MethodsA varicella case was defined as a generalized, vesicular pruritic rash in a school student lasting >4 days with onset during January 1--June 26, 2004. To identify cases, investigators reviewed records kept by the school doctor and absentee records kept by teachers, and teachers and doctors were questioned concerning rash illness among students. A questionnaire was sent to the parents of any student identified as having a rash illness to collect information concerning the student's symptoms and the results of any physician consultation. Case determination was based on the results of all three sources. A primary case was defined as the first varicella case in a student with onset of rash to appear in a classroom. A secondary case was defined as any varicella case in a student with onset of rash 11--19 days after the onset of a primary case in the same classroom. A coprimary case was defined as a varicella case in a student with onset of rash <10 days after occurrence of a primary case in the same classroom. Secondary attack rates (SARs) were calculated by dividing the number of secondary cases by all students with no history of current or previous varicella minus those with primary and coprimary cases. SARs for classrooms in which the student with the primary case had been isolated immediately were compared with SARs for classrooms in which the student with the primary case had not been promptly isolated. A case-control study was conducted; participants included all 123 students with varicella in grades K--2 and 123 controls selected randomly from all 365 students in grades K--2 with no history of current or previous varicella. Self-administered questionnaires were sent to parents of all 635 students in grades K--2. Questionnaires requested demographic information, illness characteristics, varicella vaccination history (including dates and place of vaccination), previous varicella disease history, and exposures to varicella. Parents were contacted by telephone to obtain missing information. Responses were obtained for 111 (90%) of 123 students with varicella in grades K--2. The exposure histories of these students were compared with those of 120 control students. The number of controls selected for each classroom was proportionate to the number of varicella cases that occurred in the classroom (i.e., frequency matched). In two classrooms with high attack rates (ARs), an insufficient number of control students was available, and additional control students were selected at random from other classes in the same grade. ResultsDuring January 1--June 26, of 1,407 students, 138 (10%) had a rash illness consistent with the case definition of varicella. Cases were identified in three ways: 1) the school doctor examined 77 students and recorded their temperatures; 2) a doctor in the community examined another 42 students; and 3) 19 students were identified from responses to parent questionnaires. In addition to a characteristic rash, 64 (46%) students had temperature >99.5ºF (<37.5ºC); of these, 36 (56%) had a temperature >100.4ºF (>38ºC). Four (2.9%) students had a secondary skin infection. Cases occurred in all eight grades and in 21 (60%) of 35 classrooms. Higher ARs were reported among students aged 3--8 years in the four lower grades (K--2) (Table). Although cases began to appear in January, the outbreak was not evident until mid-April, peaked in May, and ended with the closing of school on June 30. Distinct peaks of cases occurred at 15-day intervals during April--June (Figure 1). Over the course of this outbreak, teachers' records indicated that 1,090 days of absenteeism resulted from varicella illness, equivalent to 8 days of school missed per ill child. Further analysis was limited to 488 (77%) of 635 K--2 students in 15 classrooms who did not have varicella before January 1, 2004. The AR in this group was 25%; analysis of ARs by classroom identified two distinct groups: 10 classrooms with ARs <15% and five classrooms with ARs that were substantially higher (40%--80%). In all classrooms with ARs >40%, one or more ill students had remained in school >2 days while ill with a rash. These classrooms had new teachers who were not familiar with the school's isolation policy. In each of these five classrooms, outbreaks began with a student who was allowed to stay in school for >2 days while having a vesicular rash. Lax isolation continued during the second generation of cases in these classroom outbreaks, and tertiary cases followed (Figure 2). In the five classrooms in which the student with the primary case was isolated only after >2 days of rash, the SAR was 21% (34 of 163) compared with 1.7% (four of 235) in seven classrooms in which the first student with varicella rash was isolated immediately (in three classrooms, no cases occurred) (risk ratio [RR] = 10; 95% confidence interval [CI] = 3.7--29.0). In three classrooms in which a single student with a primary case was not isolated, the SAR was 26% (29 of 111) (RR = 12; CI = 4.4--34.0) compared with those classes for which cases were isolated immediately. In the two classrooms with several coprimary cases, the SAR was 9.6% (five of 52) compared with the classrooms with only isolated cases (RR = 5.2; CI = 1.5--19). Finally, the five classes in which a single student with a primary case was not isolated did not differ from other classrooms regarding crowding, availability of handwashing, activities involving close personal contact, or the sharing of items that might act as fomites (e.g., towels, eating utensils, and cups). Complete responses were obtained from 111 (90%) students with varicella and from 120 (98%) control students. The case-control study in grades K--2 demonstrated that 78 (70%) ill students used the school bus every day, compared with 39 (33%) control students (odds ratio [OR] = 4.9; CI = 2.7--9.0); 24 (33%) ill students had a history of varicella vaccination before January 1, 2004, compared with 22 (69%) controls (OR = 0.2; CI = 0.1--0.6). This excludes responses for 38 ill students and 88 controls whose parents could not provide the date and place of varicella vaccination or were otherwise uncertain. Stratification of bus riding and vaccination by classrooms or grade resulted in adjusted ORs that were not appreciably different from the crude OR and that indicated no difference in effect between high- and low-incidence classrooms (classroom-adjusted OR = 4.3; CI = 2.3--8.5 for bus riding, and 0.24; CI = 0.1--0.7 for vaccination). Parent questionnaires indicated that only two ill students were known to have had contact with an ill neighbor before onset of varicella rash. DiscussionHigh ARs (40%--80%) in classes from which students with rash were not sent home immediately are characteristic of transmission among siblings in the home setting and in primary schools before availability of vaccination (1). In this outbreak, two factors contributed to high ARs. First, 77% of K--2 students had no evidence of protection by natural immunity. Second, ill students were not isolated promptly, leading to continuing exposure to varicella for several days and ARs >40%. The estimated 77% susceptibility for children aged 3--8 years in this school is consistent with the 30% prevalence of varicella infection in children in Shanghai aged 3--6 years in 1998 (3). A factor that could contribute to high susceptibility for varicella illness is the number of families with only one child as a result of China's one-child-per-family policy, which has been in effect since 1979. By 2001, of approximately 291 million families in China, approximately 130 million (44%) had only one child, and 102 million (35%) had two children (4). Preschool children often lack older siblings who could acquire varicella at school or in the community and subsequently infect these more sequestered toddlers and preschoolers at home. Moreover, child care centers and other concentrations of susceptible infants and toddlers are rare in China. Under Chinese law, mothers receive 6 months of paid postmaternity leave to care for their infants. Thereafter, working parents customarily entrust their children to grandparents or other older relatives until age 3 years, when the children are old enough to attend kindergarten. Consequently, the possibility of exposure of preschool children to natural varicella in the home or community is substantially reduced, resulting in high prevalence of susceptibility at school entry. Similar high rates of susceptibility to varicella might be widespread among students in lower grades in China. Vaccinating susceptible students at school entry might be the most effective control method. To be effective, vaccination coverage will need to be >95% because transmission might be sustained in schools with vaccination coverage of 67%--95%. Other recommended measures include home isolation of students with a rash (5,8). In this outbreak, prompt isolation was associated with lower ARs. However, a high SAR has been reported in a school despite universal isolation from class at rash onset; in that investigation, because ill students in all classrooms were isolated promptly, the effect of isolation could not be compared with the absence of isolation (9). Isolation is only a temporary measure that simply delays but does not prevent varicella illness (1). To stop this outbreak, investigators recommended adding vaccination to isolation. However, because the investigation was conducted near the end of the term, the school could not implement this recommendation before the school year ended. Because varicella outbreaks in schools are a common occurrence in China, a more effective plan might be to vaccinate susceptible students when they begin school rather than to isolate them after an outbreak has begun. Beginning in 2005, students at this school will be vaccinated at the beginning of the school year. In 2003, the Chinese Food and Drug Administration licensed the Oka-strain varicella vaccine for children aged >12 months (11). However, varicella vaccine is not included in national or provincial vaccination programs. A major obstacle to widespread varicella vaccination in China is the high cost of this vaccine, which is 10 times more expensive than rubella vaccine and 75 times more expensive than measles vaccine. As of 2002, only 131,730 (23%) children in Shanghai aged <6 years had received varicella vaccine (10). Another possible contributing factor is that parents might not be aware of the availability of vaccine or the need to isolate ill children at home. The findings in this report are subject to at least three limitations. First, information on vaccination and previous history of varicella disease is subject to recall bias and other reporting errors on the part of the parents. Vaccination history in particular suffered from a high nonresponse rate or responses of "can't remember" or "unknown." Accordingly, only the protective effect is discussed and not vaccine effectiveness or effects on classroom-specific ARs. Second, because 94% of controls and all ill students participated in the study, selection bias was likely minimal. Finally, why two classrooms in different grades had multiple coprimary cases is unknown. Exposure in these classrooms might have led to an earlier, mild primary case that was missed by the teachers and thus was not identified. Mild varicella with sparse rashes can occur in vaccinated children; these mild infections can be transmitted to others and have been implicated in transmission in other school outbreaks (5,7). When cases are missed by school staff and parents, isolation measures are not taken. ConclusionAlthough no deaths or severe complications occurred in this outbreak, varicella is a highly contagious disease that can be fatal (11). In this outbreak, the low level of naturally acquired immunity was the principal factor underlying the high ARs recorded. Failure to isolate ill students also contributed to high ARs in five classrooms. Vaccination was available and protective, but the decision to vaccinate was left to parents. Universal vaccination at school entry might be the only reliable method of controlling varicella. In addition to preventing deaths, vaccination might also reduce hospitalizations from other varicella-related complications (12). More parents would be likely to have their children vaccinated if they understood the effectiveness of vaccine and the consequences of varicella illness. A stronger policy to encourage varicella vaccination in schools in China should be developed. Careful assessment of the cost of vaccine compared with the cost of disruption of school activities would be valuable in assisting provinces, educational authorities, and individual schools in developing a vaccination policy. Acknowledgments Xiaodong Sun, MBD, assisted with the initial interviews and data collection. Zhijie An, MBD, assisted with data analysis. James Mendlein, PhD, assisted with revising the text. Jin Zhong Yang facilitated the investigation in the school. References
Figure 1 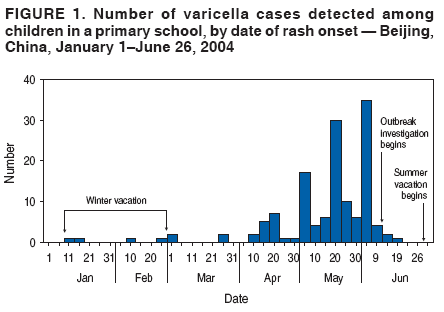 Return to top. Figure 2  Return to top. Table 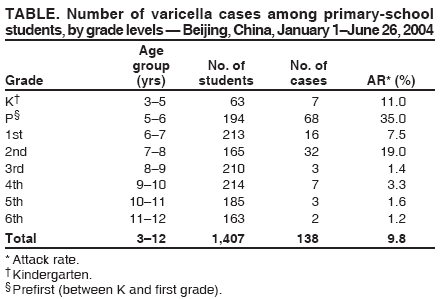 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 4/6/2006 |
|||||||||
|