 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Field Investigations of Emergency Department Syndromic Surveillance Signals --- New York CityLinda Steiner-Sichel, J. Greenko, R. Heffernan, M. Layton, D. Weiss
Corresponding author: Don Weiss, Director of Surveillance, Bureau of Communicable Disease, New York City Department of Health and Mental Hygiene, 125 Worth St, Box 22A, New York, NY 10013. Telephone: 212-442-5398; Fax: 212-676-6091; E-mail: DWeiss@health.nyc.gov. AbstractIntroduction: The New York City (NYC) Department of Health and Mental Hygiene (DOHMH) has operated a syndromic surveillance system based on emergency department (ED) chief-complaint data since November 2001. This system was created for early detection of infectious-disease outbreaks, either natural or intentional. However, limited documentation exists regarding epidemiologic field investigations conducted in response to syndromic surveillance signals. Objective: DOHMH conducted field investigations to characterize syndromic surveillance signals by person, place, and time and to determine whether signals represented true infectious-disease outbreaks. Methods: A DOHMH physician reviews ED-based syndromic surveillance results daily to look for signals. When necessary, field investigations are conducted and consist of a review of the patient line list, telephone interviews with hospital staff, chart reviews, interviews with patients, and collection and testing of specimens. Results: In November 2002, a series of citywide signals for diarrhea and vomiting syndromes, which coincided with institutional outbreaks consistent with viral gastroenteritis, prompted DOHMH to send mass e-mail notification to NYC ED directors and institute collection of stool specimens. Three of four specimens collected were positive for norovirus. In December 2002, DOHMH investigated why an ED syndromic signal was not generated after 15 ill patients were transferred to a participating ED during a gastrointestinal outbreak at a nursing home. Field investigation revealed varying chief complaints, multiple dates of ED visits, and a coding error in a complementary DOHMH syndromic system, and confirmed a seasonal norovirus outbreak. During March 2003, the system generated a 4-day citywide respiratory signal and a simultaneous 1-day hospital-level fever signal in a predominantly Asian community. In those instances, epidemiologic investigation provided reassurance that severe acute respiratory syndrome was not present. Conclusion: Detailed field investigations of syndromic signals can identify the etiology of signals and determine why a given syndromic surveillance system failed to detect an outbreak captured through traditional surveillance. Validation of the utility of syndromic surveillance to detect infectious-disease outbreaks is necessary to justify allocating resources for this new public health tool. IntroductionThe New York City (NYC) Department of Health and Mental Hygiene (DOHMH) has operated a syndromic surveillance system based on emergency department (ED) chief-complaint data since November 2001. By November 2003, 44 of NYC's 67 EDs participated in this system, thereby capturing 80% of all NYC ED patient visits. This paper describes three investigations of ED syndromic signals that required in-depth fieldwork to characterize the syndromic signals by person, place, and time and to determine whether the signals represented true infectious-disease outbreaks. MethodsOverview of the DOHMH ED Syndromic Surveillance SystemThe methods used for obtaining ED data for syndromic surveillance are described in detail elsewhere (1). Briefly, the DOHMH syndromic surveillance system receives ED data through daily electronic transmission of files containing free-text chief complaint, age, sex, residential zip code, and date and time of ED admission. A computer algorithm codes the free-text chief complaint into one of four syndromes: respiratory, fever (includes influenza-like illness), diarrhea, and vomiting. Daily statistical analyses evaluate citywide temporal trends and spatial clustering, by hospital and residential zip code, for respiratory and fever syndromes in persons aged >13 years and for diarrhea and vomiting syndromes in patients of all ages. A signal is defined as a statistically significant increase in ED visits for a syndrome over a predetermined baseline. The temporal scan statistic (2), which compares the ratio of visits for one of the four syndromes to visits for other reasons (i.e., those that do not fall into an infectious-disease syndrome category) during the previous 1, 2, or 3 days to a 14-day baseline (2), is used for citywide analysis. A modified spatial scan statistic and a 14-day baseline are used for spatial analyses, adjusting for both purely temporal (e.g., a citywide increase in syndrome visits) and purely spatial variation (e.g., consistently higher syndrome visits within a particular zip code) (3). Significance is set at p<0.01, a level selected to manage the number of epidemiologic investigations while minimizing the probability of missing a real event. The extent of an investigation depends on the syndrome, the size and geography of the signal, its overlap with other syndromes, signals generated by complementary systems, and the current level of concern (e.g., during certain high profile events). Steps in Spatial Signal InvestigationsAn analyst and a medical epidemiologist review the output daily and note any statistically significant citywide or spatial signals. Signal investigations are conducted according to the following priority: 1) spatial signals for fever and respiratory, 2) citywide signals for fever and respiratory, 3) spatial signals for diarrhea and vomiting, and 4) citywide signals for diarrhea and vomiting. Compared with a citywide signal, a spatial signal has limited geographic dimensions (i.e., >1 neighboring hospitals or zip codes) and a focused epidemiologic investigation. All spatial signals are investigated to varying degrees, depending on factors mentioned previously. A line list of ED visits captured in the signal is reviewed for duplicate entries and for typographic or coding errors. Descriptive statistics are generated on age, sex, residential zip code, and time of admission to examine patterns among the patients. Chief-complaint data are subcategorized to further uncover similarities among the patients. Hospitals involved in the signal are then called to request interim data and to assess the volume and severity of patients visiting the ED during that time. ED staff are asked about the syndrome of interest and about any other severe or unusual clusters or similarities among patients. Speaking with hospital staff is a valuable component of a signal investigation; it provides a direct assessment of current ED activity and heightens the clinician's awareness of the specified syndrome. Speaking with physicians who worked the previous day is often helpful because they are usually more familiar with the ED visits responsible for the signal. Data from complementary surveillance systems (e.g., ambulance calls and pharmaceutical sales) are reviewed for any signals occurring within the same syndrome category. Certain hospitals also provide an interim 12-hour ED chief-complaint log for the current day's data, which is coded and reviewed to evaluate whether the syndrome trend is continuing. If ongoing illness exists, DOHMH might ask ED physicians to lower their threshold for ordering certain diagnostic tests (e.g., blood cultures, stool cultures, chest radiographs, or rapid influenza tests). When necessary, patients are called at home to inquire about their condition. If evidence indicates that the outbreak is continuing, DOHMH staff are sent to EDs to interview patients (or their families), review charts of ED visits and hospital admissions by using a standardized chart-abstraction tool, and assist with collection and transport of specimens to the DOHMH public health laboratories (PHL). ResultsDuring November 15, 2001--November 14, 2003, a total of 142 citywide signals occurred on 111 surveillance days, including 22 respiratory syndrome signals and 33 fever syndrome signals during peak influenza season, and 25 diarrhea syndrome signals and 28 vomiting syndrome signals during the autumn and winter viral gastroenteritis seasons. Hospital-level signals included 51 signals for respiratory and fever syndromes and 58 signals for diarrhea and vomiting syndromes. At the zip-code level, 39 signals for respiratory and fever syndromes and 50 for diarrhea and vomiting syndromes occurred. The following section describes three in-depth epidemiologic field investigations conducted in response either to a syndromic surveillance signal or to the lack of a signal during an otherwise reported outbreak. Investigation 1Background. In October 2002, a series of citywide signals for diarrhea and vomiting syndromes coincided with institutional outbreaks clinically consistent with acute viral gastroenteritis. A hospital-level spatial signal for diarrhea syndrome involving two hospitals (A and B) occurred on both October 29 and 30 for both hospitals (Table 1). Response. DOHMH sent an e-mail message to ED directors of hospitals participating in syndromic surveillance, alerting them to the citywide increase in gastrointestinal illness (GI) and asking them to lower their threshold for diagnostic testing, collect viral stool specimens, and identify common exposures or unusual circumstances among ED patients. Hospitals A and B were involved in both days of this hospital-level spatial signal. Infection-control nurses at both hospitals were contacted and patient line lists examined. Further analyses determined that the citywide increase in GI primarily affected young children (Figure). Staff were sent to Hospital A's pediatric ED to interview patients and collect stool specimens (for bacterial, ova and parasite, and viral testing) to determine an etiology. In addition, a health alert (http://www.nyc.gov/html/doh/html/cd/02md37.html) was sent to hospitals and schools citywide via broadcast fax and e-mail. Findings. At Hospital A, two stool specimens were obtained on site and two collection kits were sent home with parents of ED patients and later retrieved and delivered to PHL through pre-arranged transportation. Three of the four specimens collected were positive for norovirus. Norovirus was widespread throughout multiple parts of the United States, including New York City, during the winter of 2002. During November 2002--mid-January 2003, DOHMH received reports of 66 outbreaks of gastroenteritis epidemiologically consistent with norovirus infection affecting approximately 1,700 persons. Outbreak settings were primarily nursing homes and long-term care and rehabilitation facilities but also included hospitals, restaurants, a homeless shelter, and a school. In all, 29 stool specimens were tested, of which 19 (66%) were positive for norovirus (4). No epidemiologic links among patients presenting to Hospitals A and B were uncovered during the investigation. Thus, syndromic surveillance was an early indicator of citywide GI consistent with seasonal trends of norovirus. Investigation 2Background. In December 2002, the DOHMH epidemiologist for foodborne illness received a call from a nursing-home director reporting 80 (of 320) residents with GI. On December 1, 2002, 25 nursing-home residents were transported by ambulance to four local hospital EDs. Although two of the four hospitals were participants in NYC's ED syndromic surveillance system, one of which (Hospital G) received 15 of the nursing home patients, NYC's ED syndromic surveillance system did not detect this GI cluster at Hospital G. To investigate the system's failure to signal, DOHMH conducted a retrospective, age-specific (persons aged >60) spatial analysis, which did detect a GI cluster. Five hospitals, including Hospital G, were included in the cluster; however, none of the 15 cases transferred to Hospital G had been captured (Table 2). Response. Hospital charts for the 15 patients reportedly transferred to Hospital G by ambulance on December 1, 2002, were requested for review, of which 13 (87%) were available. According to ED records, only nine of these 13 patients were treated at Hospital G's ED on December 1, 2002; the other four patients were brought in on December 2 or 3, 2002. Chief complaints for two of the nine patients were not for a gastrointestinal illness but for atrial fibrillation and syncope, which were either the primary or only reason for the ED visits. Chief complaints noted in the medical records of the remaining seven patients were consistent with gastroenteritis. Because the nursing-home residents were transferred by ambulance to the EDs, DOHMH reviewed the emergency medical services (EMS) ambulance-dispatch log, a complementary syndromic surveillance system. The data provided by the ambulance-dispatch log includes job number, date and time of call, call type, and the EMS chief complaint. This information was obtained from the ambulance call report, a copy of which was found in patient ED charts. A detailed review of the EMS database indicated that eight of the nine patients were transferred by EMS from the nursing home to Hospital G's ED on December 1, 2003; the other patient was transported by private ambulance. Three EMS call types were documented for these eight patients: sick, unconscious, and multiple casualty incident. A single multiple casualty incident call accounted for five of the patients transported to the hospital. None of the EMS call types were related to GI. Findings. The ED at Hospital G had incorrectly entered the nonspecific EMS call types indicated on the ambulance call report as the chief complaints instead of as the patients' subjective complaints given to EMS providers. Thus, these nonspecific call types, none of which indicated acute gastroenteritis, were received electronically by syndromic surveillance, instead of the chief complaints noted in the medical records. Therefore, critical information that would typically be captured and coded into a key syndrome was lost. Meanwhile, a concurrent foodborne-outbreak investigation determined that 10 of 11 stool specimens collected from ill nursing-home residents were positive for norovirus. Investigation 3Background. During March 2003, simultaneous citywide respiratory (4 days) and fever (3 days) signals occurred (Table 3). These signals coincided with the World Health Organization's global alert on March 12, 2003, about cases of atypical pneumonia, an outbreak later determined to be severe acute respiratory syndrome (SARS). On March 16, 2003, a spatial signal for fever syndrome occurred in a predominantly Asian community for both the hospital (observed n = 23/expected n = 7.4; p = 0.001) and zip code (observed n = 9/expected n = 0.9; p = 0.002) analyses. Within the hospital signal, Hospital L (observed n = 20/expected n = 6.7) appeared to be driving the cluster, with 13 excess cases compared with Hospital M (observed n = 3/expected n = 0.7) (Table 4). Response. DOHMH initiated an epidemiologic investigation on March 17, 2003. Patient line lists revealed that illness was distributed among all adult age groups and that chief complaints were consistent with influenza-like illness. ED staff were interviewed about concerning cases, unusual trends or clusters, and any travel histories, none of which were reported. The hospital infection-control practitioner collected contact information for patients with chief complaints consistent with fever and respiratory syndromes and identified patients admitted to the hospital. Patients treated in the ED for respiratory or fever syndromes on March 16, 2003, were contacted by telephone by a DOHMH physician on March 17, 2003. Sixteen patients were called and five patients were interviewed. All five reported improvement; one patient reported having traveled through Frankfurt Airport but denied having traveled to Asia, and one patient had visited the ED because of increased media reports on SARS. The remaining 11 patients either had incorrect or disconnected telephone numbers or did not respond after three attempts. DOHMH staff visited Hospital L's ED on March 17 and 18, 2003, to review medical records and to interview staff and any patients (or their families) remaining in the ED who complained of fever or respiratory problems. Hospital staff reported no unusual clusters of illness or increase in patients complaining of fever or influenza-like illness. Two ED patients' families were interviewed, none of which reported recent travel to Asia. Sixteen medical records were reviewed, including those of patients admitted to the hospital. Findings. This investigation of a hospital-level spatial signal for fever syndrome and concurrent citywide 3-day fever and 4-day respiratory syndrome signals did not uncover any features indicative of an outbreak or importation of SARS. No similarities in disease presentation, epidemiologic links, or etiologic agents were identified. These negative findings reassured the health department that no communitywide outbreak of febrile or respiratory illness related to SARS existed, particularly because the trend did not continue. Whether these signals represented an unusual statistical anomaly or focal community illness caused by one or more agents remains unknown. DiscussionThese field investigations illustrated both the difficulties of and resources required in identifying the cause of temporal and spatial aberrations in syndromic surveillance data. Syndromic data are nonspecific by nature. For illnesses that are self-limited and of short duration, resolving the syndrome into an etiologic diagnosis is not usually of direct benefit to the patient, not a priority for the clinician, and not always feasible with current technology. The advantage of using syndromic data for outbreak detection is timeliness. Experiences to date indicate that this advantage might only be theoretical. The time required to conduct investigations and retrieve diagnostic and epidemiologic information might negate the advantage of timely data acquisition. The absence of sustained syndromic signals is usually more reassuring that an outbreak does not exist than the information obtained by an immediate investigation. Using ED syndromic surveillance for outbreak detection has certain limitations. Of the >40 spatial syndromic signals investigated by DOHMH during 2002--2003, none have been conclusively determined to be a discrete infectious-disease outbreak. Similarly, none of the localized outbreaks reported and investigated through traditional communicable disease surveillance (e.g., nosocomial- or foodborne-outbreak investigations) have yielded a simultaneous syndromic surveillance signal. This is a factor of both the difficulty of proving causality and the use of a sensitive but nonspecific detection system. Outbreaks reported through traditional means rarely involve sufficient ED visits and geographic localization to yield a syndromic signal. Even when both of these factors are present, the event might not be detected if complaint information is inaccurately recorded in the medical record, as evidenced by the second investigation described in this paper. One advantage demonstrated by NYC's ED syndromic surveillance system has been its early detection of seasonal, widespread disease trends attributed to norovirus and influenza (1). These detections have enabled DOHMH to alert the medical community proactively and distribute prevention information to providers and the public. The effect of these measures has not yet been studied. Syndromic surveillance can also provide reassurance that a large-scale outbreak does not exist, as illustrated by the third investigation presented, in which cases of fever/influenza and respiratory illness were deemed unlikely to be SARS. Using chief-complaint data instead of discharge diagnosis or information from the clinical evaluation might result in a more limited representation of patient illness; however, such clinical information is difficult to code and not timely. NYC's system relies on ED visits, which are uncommon for adults with mild or prodromal illness. More experience is needed with these systems, including an evaluation of the systems' performance in the presence of large outbreaks. Meanwhile, DOHMH has learned useful lessons for conducting future signal investigations (Box). ConclusionsNYC's ED syndromic surveillance system provides rapid health information through timely electronic data collection and automated spatio-temporal analyses. The system receives data on 80% of daily ED visits citywide, which is representative of the population accessing care at city EDs. Syndromic surveillance using ED chief complaint data has proved useful as an adjunct system to enhance traditional disease reporting methods at the DOHMH. It provides timely information on seasonal patterns of illness and disease trends citywide, which will allow for prompt epidemiologic investigation in the event of a significant deviation from baseline or a suspicious signal. After a citywide outbreak is detected, syndromic data might also provide information on the epidemic's pace and magnitude. However, the ability of syndromic surveillance to detect outbreaks that are either limited or result in mild disease is as yet unproven. Given the growing interest and investment in syndromic surveillance systems, continued evaluation of these systems is needed to determine the most useful data sources, analytic methods, and signal-investigation approaches. References
Table 1 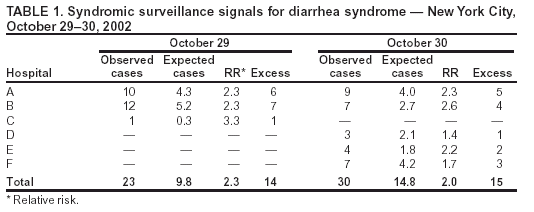 Return to top. Table 2 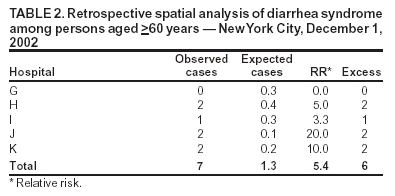 Return to top. Table 3 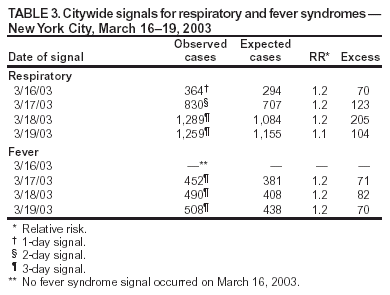 Return to top. Table 4 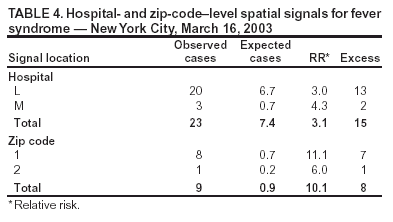 Return to top. Figure 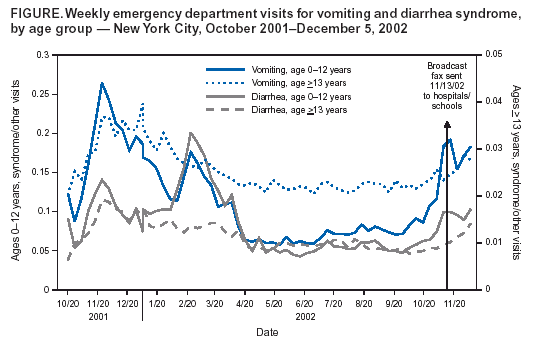 Return to top. Box 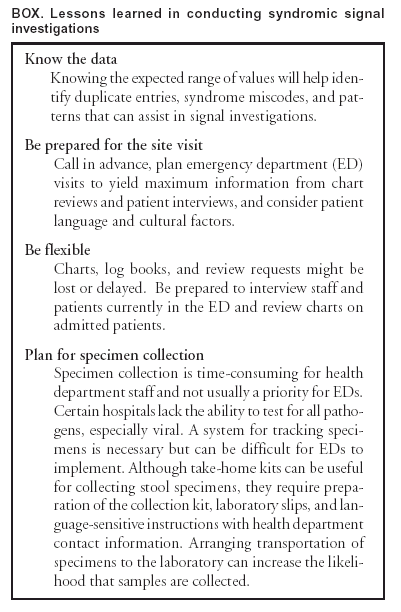 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 9/14/2004 |
|||||||||
This page last reviewed 9/14/2004
|