 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Disease Eradication and Health Systems DevelopmentB. Melgaard,* A. Creese,** B. Aylward,* J.-M. Olive,* C. Maher,*** J.-M. Okwo-Bele,**** & J.W. Lee* This article provides a framework for the design of future eradication programmes so that the greatest benefit accrues to health systems development from the implementation of such programmes. The framework focuses on weak and fragile health systems and assumes that eradication leads to the cessation of the intervention required to eradicate the disease. Five major components of health systems are identified and key elements which are of particular relevance to eradication initiatives are defined. The dearth of documentation which can provide "lessons learned" in this area is illustrated with a brief review of the literature. Opportunities and threats, which can be addressed during the design of eradication programmes, are described and a number of recommendations are outlined. It is emphasized that this framework pertains to eradication programmes but may be useful in attempts to coordinate vertical and horizontal disease control activities for maximum mutual benefits. Introduction Strategies for disease control, elimination and eradication are derived primarily from the epidemiological characteristics of the disease, the intervention available, the logistical requirements, and the resource needs. While control measures usually depend on routine services being instituted and maintained in a long-term perspective, eradication activities are characterized as time-limited, often intensive, targeted, and organized in circumscribed programmes with campaign elements as prominent features. Eradication/elimination programmes (EP) have therefore been considered to be dominated by nonsustainable activities that may bypass or, at worst, even compromise the development of the health sector, especially in the poorer developing countries. Experience from ongoing eradication programmes calls this assessment into question and indicates that they may have positive impacts on health services and systems that stretch beyond the narrow benefits of eradication of a single disease. Taylor & Waldman (1) have stressed that "past polarization between proponents of primary health care and eradication represents an exaggerated example of continuing controversies between vertical and horizontal programs. It is time to admit that this is a false polarization which has become unnecessarily emotional and irrational". The challenge that arises is to design current and future eradication and elimination programmes in such a way that they provide maximum benefits to national health systems without jeopardizing the eradication efforts. Eradication and elimination activities can make substantial contributions to sustainable health development. This article addresses that challenge. We describe major elements of health systems, the areas most relevant to eradication and elimination programmes, and identify the key issues that relate to such programmes. Selected major opportunities and threats to health systems are identified in a framework for the design of future eradication initiatives. The focus is on developing health systems and services in developing countries with weak or fragile health systems, assuming that in countries with strong systems the potential negative effects of eradication efforts are less pronounced. Health Systems and Eradication Programmes A national health system can be defined as the set of activities in a country which provide health services to the population and health results. The following are commonly recognized components of health systems (2):
This framework provides a basis for identifying and examining elements of the health systems that pertain to eradication strategies and they offer particular opportunities and/or threats (see Table 1). Eradication can be defined as "permanent reduction to zero of the worldwide incidence of infection caused by a specific agent as a result of deliberate efforts, intervention measures are no longer needed" (3). The cessation of control measures is important and distinguishes eradication from elimination. It has been argued that this makes eradication particularly favourable in cost-benefit terms. Such savings could be channelled to benefit other areas of health services. The benefits from poliomyelitis eradication in terms of savings on the global health budget has been estimated at US$ 1700 million per year for direct costs only (4). The indirect benefits are considered to be substantially higher. The sustainability of health systems can be defined as the ability to deliver an appropriate level of benefits for an extended period of time after major financial and technical donor assistance has been terminated. Sustainable health development thus relates to countries where donor assistance is available to the health sector. Since eradication programmes, by definition, aim at being terminated when successful, it follows that the question of sustainability is relevant to health system elements which are not dedicated to eradication initiatives. Eradication programmes must be implemented even in situations where health systems are weak or absent. The implementation of poliomyelitis eradication in countries afflicted by war has been achieved by negotiating between warring factions, so that immunization campaigns could be carried out on days of tranquillity. In such situations, eradication activities may contribute to the initiation of new efforts in health system strengthening. Major Issues in Health Systems Development and Eradication and Elimination Programmes Overall Health Policy and Strategic Planning Central to all national health systems is an overall health policy and the strategic planning required to implement that policy. The policy should reflect the national health priorities based on the proportional burden of disease and available resources, both human and financial, to address those priorities. Ideally, the strategic planning to reach those goals includes the delineation of specific objectives with detailed strategies, the implementation of which can be monitored through both health outcomes and process indicators. Unfortunately, in many countries, particularly those in the most difficult circumstances, health policies are often vague or outdated, if they exist at all. These same countries are frequently the last reservoirs of organisms targeted for eradication. Since donor agencies may exert a substantial influence on the policy development in such countries, stakeholders in eradication initiatives can temporarily exert a strong effect on this process. Eradication/elimination programmes are characterized by clearly defined policies and strategies. As a result, the adoption and implementation of an eradication programme can facilitate the need for a country to establish defined health goals with specific strategies and indicators for evaluation and monitoring. Basic eradication policies are often generated from the experience of countries and regions with good health systems. These policies are then adopted by the global community when the feasibility of the EP target has been demonstrated. Subsequent adoption in poor countries can be influenced by the strong promotion of the global policy as its implementation is a prerequisite for the successful achievement of targets. Eradication strategies are generally standardized with limited leeway for national adaptation and interpretation. Despite endorsing the goal of poliomyelitis eradication, some countries are reluctant to implement the WHO-recommended strategies, especially countries in Africa. For example, Ghana initially resisted vertical disease control initiatives including eradication because they were considered detrimental to overall health systems development (5). Opportunities to strengthen the national health policy process may be missed when eradication strategies are advocated for their own sake. Organization of Health Systems: Structures and Processes National health systems require an established structure with well-defined lines of authority, responsibility and accountability. Eradication programmes give an emphasis to the need for strong management capacity and processes. Countries with a good health management structure can exploit the eradication initiative to further strengthen that structure. In countries where this structure is fragile or particularly weak, an EP could undermine pre-existing lines of management authority if a separate system is established in parallel. The management demands of an EP may divert staff time away from routine programmes, as in Mozambique where a large share of the EPI management time was used to plan NIDs. However, a negative effect is by no means universal. In Cambodia, the planning and implementation of the first NIDs in the early 1990s provided a mechanism by which a recently revitalized Ministry of Health could demonstrate its capacity to conduct nationwide health initiatives while strengthening the weak lines of responsibility. Historically, EPs required the creation of new health management structures in many countries, because of the lack of an existing capacity. More recent initiatives have been implemented within the existing health management set-up even though it may be less developed. This may contribute to overall strengthening of the management capacity beyond the programme. The management of EPs is centrally driven and often leaves limited scope for change and adaptation by district authorities. Innovation at the peripheral level to successfully achieve nationally established performance indicators remains possible. These efforts can, and do, exploit the commitment and energy that develops among health staff and in the community for other health activities. To capitalize on the opportunities for health systems development the eradication strategies must concentrate on existing organizational arrangements, assess their strengths and weaknesses, and ensure that the management of the EP is designed to strengthen established structures. Financial Resources: Mobilization and Use Health systems require substantial resources, the majority of which must be identified locally, for both capital and recurrent costs. Eradication programmes utilize relatively less funds (in comparison to overall health systems development), primarily from external sources in the poorest countries, and for a time-limited period. The relationship is illustrated in Figure 1 for poliomyelitis. There is a widespread perception that the funds used for eradication programmes divert resources that would be available for health systems development in a country. There is a paucity of hard data with which to evaluate this point, but both recent and previous eradication initiatives have been capable of raising substantial additional resources compared with the underfunded routine health services. Although the capacity to raise substantial resources for eradication is partly due to the inherent nature of such initiatives, these programmes may provide lessons in resource mobilization for the health sector, since they are more efficient in both the raising and use of resources. Gyldmark & Alban (6) emphasize the need for economic evaluations of eradication programmes, with particular attention paid to the potential opportunity costs of using resources on eradication than on other more urgent health care problems. However, a sizable proportion of the resources that go to EPs might not be available for development aid at all, much less for the health sector. Striking examples of this are Rotary International's US$ 450 million for poliomyelitis eradication and SmithKline Beecham's recent donation of drug supplies worth more than US$ 2000 million for lymphatic filariasis eradication. The actual public spending from national sources on eradication activities in poor countries is small; in the poorest countries it is estimated that the maximum public sector spending on poliomyelitis eradication in a year will be US$ 0.025 to US$ 0.05 per capita. It can be argued that the cost for the poorest countries should be covered by the donor community, especially since they will benefit from successful eradication (7). Private sector involvement and volunteer contributions in-kind are much more common in eradication programmes and remain an undertapped source for the health sector. These programmes may be a model to both central and peripheral level health authorities for promoting public-private sector cooperation to achieve health goals. Human Resources: Number, Mix and Quality Even in those countries where human resource planning provides for the proper number and mix of personnel, the effectiveness is often compromised by the low performance common to the underfunded public sector. This affects the productivity of the health labour force. The impact of introducing an eradication programme, with its substantial human resource requirements, into such a setting must be considered. Increased staff resources (in time if not in actual personnel) are required at both the central and peripheral levels for eradication activities. Whether these extra resources are met by expanding staff at the central level or increasing the work load for all existing staff, there remains a concern that this could in turn divert staff time from routine tasks. Unfortunately, there is only anecdotal information on this issue. There are no data to determine whether the introduction and implementation of an eradication programme increases the productivity of the health sector as opposed to diverting energies to the detriment of other programmes. Evaluating the opportunity costs of any new programme in a developing country setting is complicated by the generally low productivity of the public sector. The Taylor Commission (8) highlighted both the commitment and positive attitude of staff during poliomyelitis eradication in the Americas but also the frustration over the prioritization of staff time to this disease. The incentives which are sometimes introduced for certain eradication functions, such as surveillance, seldom if ever exist in the routine services. Such rewards have attracted staff to eradication and increased their commitment, while discouraging staff who are not involved. In the more recent programmes, however, rewards are usually foregone in preference to reimbursement of actual costs -- possibly a feasible model for improving the productivity of the health sector in general. Training for eradication is very target oriented and generally dedicated, but often carried out with little attention to other health training activities. These, similarly, tend to be uncoordinated, thereby compromising the delivery of routine services. Service Management and Delivery The equity problem of ensuring access to services for all population groups is particularly acute in countries where curative services in major population centres receive priority. Countries with fragile civil institutions and with limited financial resources are especially susceptible. Eradication strategies must be designed to increase access to and utilization of services beyond that normally achieved by routine services. To achieve this goal, eradication efforts often include campaign elements. While the interventions are usually specific to the eradication initiative, the campaigns may offer opportunities for the addition of other interventions. Although such strategies can deliver health interventions to the entire population, the impact on other health priorities must be considered. Routine coverage has been reported to drop immediately following national immunization days in some countries, but subsequently has usually climbed back to similar if not higher levels. Routine information systems are often fragmented and unreliable and improvements can be compromised by the development and consolidation of surveillance for eradication, if it is initiated as a parallel and specific activity. This was a concern when of the surveillance system for poliomyelitis eradication was established in Cambodia (9), but the system was gradually expanded to include other diseases. Similarly the poliomyelitis surveillance system played an important role in the cholera epidemic in Latin America in the late 1980s. The surveillance approach to disease control has significant potential for integration and expansion to other priority diseases, as exemplified by the integrated disease surveillance system being promoted in the African region with poliomyelitis surveillance as one of a number of central functions. Performance monitoring is rare in the health sector but common in eradication programmes. A broader adaptation of performance indicators may enhance the quality of other health services. Conclusions and Recommendations Eradication and elimination programmes offer both opportunities and threats to health systems development. While early eradication efforts were implemented as vertical operations -- often in the absence of a service delivery system -- more recent programmes have increasingly utilized and worked within the frame of the existing health system (10,11). This has sometimes led to diversion of resources and disputes over the priority accorded to eradication when a global objective is pursued in countries which do not share this prioritization. Increasingly, evidence is being collected on the beneficial impacts of eradication efforts on the health sector and it has become apparent that carefully designed programmes may produce benefits beyond the eradication goal (8,12). The framework presented in this article provides guidance for the design of future programmes to maximize the support to national health systems development and thus increase the impact on the health status of the populations. The framework is applicable primarily to eradication initiatives but may be adapted to other targeted ("vertical") health programmes in order to strengthen the coordination of health systems development and disease control efforts for mutual benefit. The following main recommendations are put forward:
References
* Global Programme on Vaccines and Immunization, World Health Organization, 1211 Geneva 27, Switzerland. ** Division of Analysis, Research and Assessment, World Health Organization, 1211 Geneva 27, Switzerland. *** Expanded Programme on Immunization, World Health Organization, Regional Office for the Western Pacific, Manila, Philippines. **** Expanded Programme on Immunization, World Health Organization, Harare, Zimbabwe. Table 1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size. TABLE 1. Key elements of health systems and examples of the opportunites and threats presented by the implementation of disease eradication or elimination programmes
Return to top. Figure 1 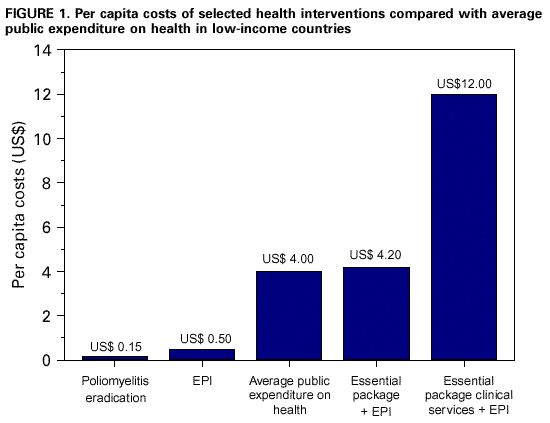 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/3/2000 |
||||||||||||||||||||||||||||||||||||||||||||||||||
This page last reviewed 5/2/01
| ||||||||||||||||||||||||||||||||||||||||||||||||||