 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Measles Eradication: Experience in the AmericasC.A. de Quadros,* B.S. Hersh,** A.C. Nogueira,** P.A. Carrasco,** & C.M. da Silveira** In 1994, the Ministers of Health from the Region of the Americas targeted measles for eradication from the Western Hemisphere by the year 2000. To achieve this goal, the Pan American Health Organization (PAHO) developed an enhanced measles eradication strategy. First, a one-time-only "catch-up" measles vaccination campaign is conducted among children aged 9 months to 14 years. Efforts are then made to vaccinate through routine health services ("keep-up") at least 95% of each newborn cohort at 12 months of age. Finally, to assure high population immunity among preschool-aged children, indiscriminate "follow-up" measles vaccination campaigns are conducted approximately every 4 years. These vaccination activities are accompanied by improvements in measles surveillance, including the laboratory testing of suspected measles cases. The implementation of the PAHO strategy has resulted in a marked reduction in measles incidence in all countries of the Americas. Indeed, in 1996 the all-time regional record low of 2109 measles cases was reported. There was a relative resurgence of measles in 1997 with over 20,000 cases, due to a large measles outbreak among infants, preschool-aged children and young adults in Sao Paulo, Brazil. Contributing factors for this outbreak included: low routine infant vaccination coverage, failure to conduct a "follow-up" campaign, presence of susceptible young adults, and the importation of measles virus, apparently from Europe. PAHO's strategy has been effective in interrupting measles virus circulation. This experience demonstrates that global measles eradication is an achievable goal using currently available measles vaccines. Introduction In 1994, the countries of the Region of the Americas established the goal of eliminating measles from the Western Hemisphere by the year 2000 (1). Measles is one of the most highly infectious diseases, and in the prevaccine era, essentially everyone eventually acquired measles infection, usually as a very young child. Humans are the only reservoir for measles infection, although some other primates, such as monkeys, can be infected. The patient is most infectious during the prodromal phase of the disease before the onset of symptoms such as fever and rash. Communicability decreases rapidly after the appearance of rash (2). Live attenuated measles vaccine, first licensed for use in the USA in 1963, was in widespread use by the late 1970s (3). Immunization with this vaccine has been demonstrated to be protective for over 20 years, but immunity following vaccination is thought to be life-long (4). Vaccine efficacy has been shown to be 90-95%. Because of interference of maternal antibodies, vaccine efficacy increases steadily after 6 months of age, reaching its maximum plateau of 95-98% at 12-15 months of age. By 1982, virtually all countries in the world had incorporated measles vaccine into their routine vaccination schedules and, since then, coverage has increased substantially. By 1990, the estimated overall global coverage for children by 2 years of age was approximately 70%. Before the introduction of measles vaccine, epidemics characteristically tended to recur every 2-3 years in most densely populous areas, but with the widespread use of measles vaccine, the interval between outbreaks has lengthened (5,6) and an increase in the average age of infection is observed. In the developing countries which recently introduced the vaccine and have not yet achieved high immunization coverage, measles remains endemic with most cases occurring in young children and infants (7). WHO has estimated that 40 million measles cases, with 1 million deaths, are still occurring annually in the world. PAHO Measles Eradication Strategy The Pan American Health Organization (PAHO) recommends a strategy that aims to interrupt rapidly measles transmission by initially conducting a one-time-only mass campaign targeting all children aged 9 months to 14 years and to maintain interruption of transmission by sustaining high population immunity through vaccination of infants at routine health services facilities, supplemented by periodic mass campaigns conducted approximately every 4 years, targeting all 1-4-year-olds, regardless of previous vaccination status. "Fever and rash" surveillance and measles virus surveillance are other key elements of the strategy (8). The initial "catch-up" measles vaccination campaign is conducted during periods of low measles transmission. All children aged 9 months to 14 years, irrespective of vaccination history or reported history of measles infection, are immunized with measles vaccine within a very short period of time, usually one week to one month. These campaigns result in a rapid increase in population immunity and, if high enough coverage is achieved, measles transmission is interrupted. After a catch-up campaign has been conducted, there may still remain pockets of susceptible children. To detect these, a post-catch-up campaign evaluation is conducted and special vaccination (mop-up) activities are carried out in such areas to increase their level of coverage. After the initial catch-up campaign and mop-up operations, routine immunization services (keep-up) should ensure that all new birth cohorts of children are vaccinated with a dose of measles vaccine at 12-15 months of age. However, there will inevitably be an accumulation of susceptible preschool-aged children over time. Two major factors contribute to the accumulation of susceptibles. First, measles vaccine is not 100% effective, thus leaving some children unprotected despite vaccination. Second, measles vaccination coverage for each birth cohort will fall short of 100%, however effective the programme. Thus, the PAHO strategy calls for periodic vaccination campaigns to be conducted among preschool-aged children (children less than 5 years of age). This is recommended whenever the estimated number of susceptible preschool-aged children approaches the size of an average birth cohort. In the Americas it is recommended that such follow-up campaigns be conducted every 4 years. A sensitive surveillance system is essential for a measles elimination programme. This includes the notification and timely investigation of infants and children with suspected measles. Serological testing for anti-measles IgM antibodies in blood specimens obtained from suspected cases is used to confirm or rule out measles virus infection. A confirmed measles case must either have serological confirmation or an epidemiological link to another laboratory-confirmed measles case. Laboratory sequencing of the measles virus genome from isolates can help to determine geographical sources of outbreaks and identify pathways of transmission. Since 1991, all PAHO Member countries, with the exception of the USA, have conducted catch-up measles vaccination campaigns (Table 1) and most countries have already conducted at least one follow-up campaign. Summary of Impact In the Region of the Americas, reported cases have decreased markedly and the majority of countries have reported a 99% reduction in measles incidence compared to the prevaccine era. Several countries have already interrupted transmission. In Cuba, after the catch-up campaign conducted in 1987 and a follow-up campaign conducted in 1991, fewer than 20 confirmed measles cases were reported annually between 1989 and 1992, with the last serologically confirmed case occurring in June 1993 (9). Other countries in the Region of the Americas in which transmission apparently has been interrupted include the English-speaking Caribbean, which conducted its catch-up measles vaccination campaign during May 1991. Between September 1991 and March 1997, only two confirmed measles cases were reported in the English-speaking Caribbean -- in Barbados (one acquired the infection in New York City, and no source of infection could be found for the other). No secondary spread of infection occurred (10). After Chile conducted its catch-up campaign during 1992, only one case was discovered in 1992 (imported from Peru) and one in 1993 (imported from Venezuela). No further spread occurred until a recent importation from Brazil, in 1997. Transmission in this outbreak has now been interrupted. During 1996 the Region of the Americas recorded an all-time low of only 2109 confirmed measles cases (Figure 1). In 1997, however, there was a relative resurgence of the disease in Brazil. Up to 31 January 1998, a total of 78,033 suspected measles cases was reported from the countries of the Americas. One third of these (26 722 (34.2%)) have been confirmed; and 25,559 of these were reported from Brazil alone which, with Canada (580 confirmed cases), accounted for 97.8% of the total confirmed cases in the region. Other countries reporting measles cases in 1997 included Guadeloupe (128 cases), USA (127 cases), Paraguay (124 cases), Argentina (58 cases), Chile (47 cases), and Costa Rica (14 cases). The outbreaks in Argentina, Chile, Costa Rica, Chile and Paraguay originated from importations from Brazil, and the Guadeloupe epidemic was due to an importation from metropolitan France in late 1996 (11). This island had not implemented PAHO's recommended measles eradication strategy. In the USA, over half of the cases originated from importations from Europe and Asia. Spread from importations has been limited and the largest outbreak in 1997 was only 8 cases. In 1995 and 1996, there were no measles importations from Latin America or the Caribbean into the USA (12). In 1997, however, there were 5 confirmed imported cases from Brazil (13) (Figure 2). The majority of cases from Brazil have been reported from Sao Paulo State, the only state in the country which did not conduct a follow-up vaccination campaign in 1995 (13). To date, over 20,000 cases have been confirmed in this outbreak, with most cases in the city of Sao Paulo. Over 50% of cases occurred in young adults aged 20-29 years. The highest age-specific incidences are in infants, young adults aged 20-29 years, and children aged 1-4 years, respectively. To date, 20 measles-related deaths have been reported, most in infants aged less than 1 year. An investigation of measles cases in adults found that the majority were occurring among young adults who were members of certain risk-groups including men who recently migrated to cities from rural areas in the north-east of the country to work in construction projects, other manual labourers, students, health care workers, persons working in the tourist industry, and military recruits (14). Measles virus has been isolated from several patients from this outbreak and the genomic sequencing of these isolates revealed that the virus circulating in Sao Paulo is virtually identical to that currently circulating in Western Europe, which strongly suggests importation from the latter area (14). The Sao Paulo outbreak is waning after implementation of an aggressive outbreak response, which included a follow-up campaign targeting all children aged 1-4 years, selective mop-up vaccination in schools, and vaccination of young adult members of groups at high-risk for measles (14). Until 1997, the English-speaking Caribbean had not reported a single confirmed case of measles in a period of over 5 years (13). However, in 1997 two laboratory-confirmed measles cases were detected. The first was reported from the Bahamas. The patient, a young adult, had rash onset in March 1997. The direct source of transmission was not identified, but it is strongly suspected that the patient contracted measles from a tourist. A search, involving a review of over 80,000 diagnoses from health facilities in the country, was made to identify any additional cases of measles. The second case was reported from Trinidad and Tobago. It occurred in a young adult Italian sailor who had rash onset in April. The patient had acquired measles in Italy. A specimen was collected and found to be positive for measles IgM at the measles laboratory of the Caribbean Epidemiology Centre (CAREC). No spread of cases was identified despite careful investigation. Discussion While the resurgence of measles in the Americas during 1997 represents a major increase compared to cases reported in 1996, these cases represent only about 10% of those reported in 1990. Nevertheless, important lessons can be learned from this experience. First, the lack of a timely follow-up vaccination campaign in Sao Paulo, in 1995, for children aged 1-4 years, combined with low routine measles vaccination coverage (keep-up) among infants using a 2-dose schedule, allowed for a rapid and dangerous accumulation of susceptible children. Second, the presence of large numbers of young adults who escaped both natural measles infection and measles vaccination increased the risk of a measles outbreak. Third, measles virus was imported into Sao Paulo, probably from Europe. Finally, the high population density in Sao Paulo facilitated contact between persons infected with measles and susceptible persons. Measles case surveillance combined with molecular epidemiological data suggest that the countries of the Region of the Americas are constantly being challenged by imported measles virus from other regions of the world where measles remains endemic (15). During 1997, 27 separate importations of measles virus were detected from Europe, 18 from Asia, and 2 from Africa (Figure 3) which resulted in measles transmission (13). These data, however, probably severely underestimate the true number of measles importations since many imported cases may not seek medical care and do not result in further transmission. The outbreaks in Brazil, Canada and other countries of the region suggest that there may be a significant number of young adults who remain susceptible to the disease. For practical purposes, persons born before 1960 in most countries of the Region of the Americas can be assumed to have been exposed to naturally circulating measles virus, and thus be immune to the disease. Therefore, the overwhelming majority of adults are already immune, and most susceptible young adults are at very low risk of being exposed to measles virus. Mass campaigns among young adults are not recommended. However, experience has shown that certain institutional settings (e.g. colleges and universities, military barracks, health care facilities, large factories, and prisons) can facilitate measles transmission, if measles virus is introduced to such populations. In addition to persons living or working in these settings, adolescents and young adults who travel to countries with endemic measles transmission are at increased risk of being exposed to and contracting measles. To prevent the occurrence of measles outbreaks among adolescents and young adults, efforts are needed to ensure measles immunity in these potentially high-risk groups and persons travelling to measles-endemic countries. The measles experience of 1997 clearly demonstrates that there are two major challenges to the region's measles eradication goal by the year 2000. First, the countries of the Region of the Americas need to maintain the highest population immunity possible in infants and children, and to target vaccination to adolescents and young adults who are at highest risk for being exposed to measles virus. Second, increased efforts are needed in other regions of the world to improve measles control and to decrease the number of exported measles cases to the Region of the Americas. As long as measles virus circulates anywhere in the world, the Region of the Americas will remain at risk for measles. The successful achievement of the measles elimination goal in the Region of the Americas will require full implementation of PAHO's recommended immunization strategy in all countries of the region and improved measles control/elimination in other regions of the world, especially Europe and Asia, with the ultimate goal of global eradication of the measles virus (16). References
* Pan American Health Organization, Washington, DC, USA. ** Special Program for Vaccines and Immunization, Pan American Health Organization, Washington, DC, USA. Table 1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size. TABLE 1. Countries conducting catch-up and follow-up campaigns, 1987-97
* Follow-up campaign was to be conducted before writing of this paper. Return to top. Figure 1 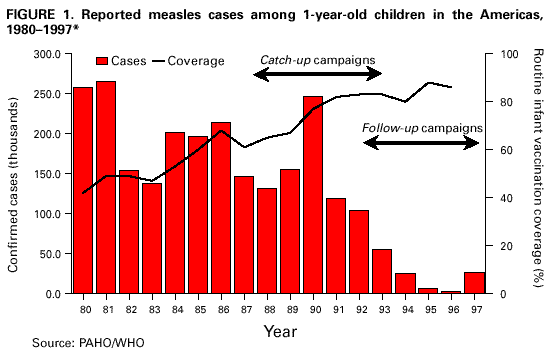 Return to top. Figure 2 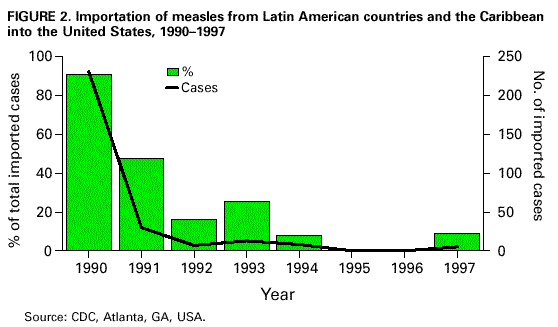 Return to top. Figure 3 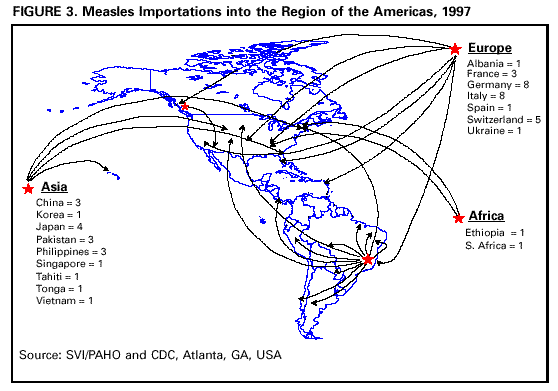 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/3/2000 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
This page last reviewed 5/2/01
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||