Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Trichinellosis Surveillance --- United States, 2002--2007
Abstract
Problem/Condition: Trichinellosis is a parasitic disease caused by roundworms of the Trichinella genus. Humans are incidental hosts who become infected after ingestion of raw or undercooked meat containing encysted larvae of Trichinella spp. Common signs and symptoms of trichinellosis include eosinophilia, abdominal pain, fever, periorbital edema, and myalgia.
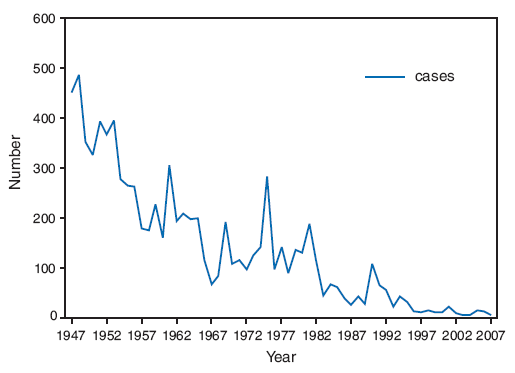
National surveillance has documented a decline in the reported incidence of trichinellosis in the United States since 1947, the first year nationwide data were collected systematically. The decreased incidence of trichinellosis has mirrored the decrease of Trichinella in commercial pork products as a result of changes in pork industry management standards and government regulations. In addition, an overall decrease has occurred in the number of cases of trichinellosis related to pork consumption. During 1997--2001, meats other than pork were the most common source of infection, and more cases were associated with home-raised pork than with store-bought pork.
Reporting Period Covered: 2002--2007.
Description of System: Trichinellosis is a reportable disease in 48 states and has been a nationally notifiable disease since 1966. Cases are defined by clinical characteristics and the results of laboratory testing for evidence of Trichinella infection. States report cases to CDC through the National Notifiable Diseases Surveillance System. Reported cases are summarized weekly and yearly in MMWR. In addition, states are asked to submit a standardized case report form with supplementary case data to CDC's Division of Parasitic Diseases.
Results: During 2002--2007, a total of 66 cases of trichinellosis were reported to CDC. Those cases for which a supplementary case report form was not submitted or that did not meet the case definition were excluded from analysis. Of the 66 cases reported during 2002--2007, a total of 12 (18%) cases were excluded from analysis.
Associated meat products were classified as either pork or meat products other than pork and were identified for 43 (80%) cases. Meat products other than pork were associated with 27 (50%) cases: 21 with bear meat, one with either bear or deer meat, one with cougar meat, one with deer meat, one with walrus or seal meat, and two with commercial beef. Pork was associated with 10 (19%) cases: seven with commercial pork, two with noncommercial pork, and one with an unspecified type of pork. Of the seven cases associated with consumption of commercial pork, five were linked to U.S. commercial pork, and two were attributed to pork ingested during travel in Asia. The two cases associated with noncommercial pork were attributed to wild boar meat; one case involved wild boar meat from a farm and the other wild boar meat from a farmers' market. Six patients reported consuming both pork and meat products other than pork, but the infected meat product could not be identified.
Interpretation: The number of reported trichinellosis cases attributed to commercial pork consumption remains low. The greatest number of cases continues to be associated with consumption of meat other than pork, especially bear meat.
Public Health Action: For the incidence of trichinellosis in the United States to be reduced further, education regarding safe food preparation practices and prevention of trichinellosis should be targeted toward hunters and other consumers of wild game meat, especially bear.
Introduction
Trichinellosis is a parasitic disease caused by numerous species of roundworms of the genus Trichinella and is enzootic worldwide in many carnivores and omnivores, especially scavengers (1). Humans are infected after ingestion of raw or undercooked meat containing viable encysted larvae of Trichinella spp. Trichinellosis is divided into two phases: an enteral (gastrointestinal) phase and a parenteral (systemic) phase. During the enteral phase, larvae are released from the ingested cysts and invade the wall of the small intestine, where they become adult roundworms. The invasion of the small intestine can cause gastrointestinal symptoms (e.g., upper abdominal pain, diarrhea or constipation, vomiting, and low-grade fever). The parenteral stage begins approximately 5 weeks after ingestion of viable encysted larvae, when adult females release larvae that then migrate to striated muscles, where they encyst. Migration and encystment of larvae can cause inflammatory reactions and local tissue necrosis and can lead to periorbital edema, facial or peripheral edema, fever, myalgia, conjunctivitis, headache, rashes, bronchitis, and eosinophilia. Fatal cases caused by neurologic and myocardial complications occur rarely (1,2). Albendazole is recommended for treatment of the intestinal-stage parasite, while albendazole in conjunction with a steroid may be used during the parenteral phase to treat more serious symptoms.
In the United States, the national trichinellosis surveillance system has documented a decline in the number of trichinellosis cases reported since 1947, the first year that data were collected systematically in the United States. The median number of cases reported annually has declined from 393 during 1947--1951 to 12 during 1997--2001 (3). Historically, the majority of cases of trichinellosis in the United States have been caused by consumption of Trichinella-infected pork, and the decline in human cases is attributed to the decrease in the prevalence of Trichinella infection among commercial swine (3,4). During 1997--2001, consumption of meats other than pork, particularly wild game meat, was the most common cause of infection; more cases were associated with home-raised pork than with store-bought pork (3).
Methods
State health departments report new cases of trichinellosis to CDC through the National Notifiable Diseases Surveillance System with electronic reporting of new cases using the National Electronic Telecommunication System for Surveillance or the National Electronic Disease Surveillance System (5). Additional clinical and epidemiologic information is gathered for each case and reported to CDC on case report forms (CDC 54.7 Rev. 02-90).
A confirmed case of trichinellosis is defined as illness with clinically compatible manifestations of trichinellosis (e.g., eosinophilia, fever, periorbital edema, and myalgia) and laboratory-confirmed Trichinella infection. Laboratory confirmation of infection is made either by a positive serologic test for Trichinella-specific antibody or by identification of Trichinella larvae in tissue obtained by muscle biopsy. An outbreak is defined as two or more epidemiologically linked cases, at least one of which must be laboratory-confirmed. An outbreak-associated case should be reported as confirmed if the patient shared an epidemiologically implicated meal or ate an epidemiologically implicated meat product and had either a positive serologic test for Trichinella or a clinically compatible illness (5).
This report presents trichinellosis surveillance data for 2002--2007. Reported cases not meeting the confirmed case definition or for which a supplemental case report form was not submitted were excluded from analysis. For data analysis, commercial pork products were defined as pork purchased at supermarkets, butcher shops, or restaurants. This category also includes pork products eaten in other countries. Noncommercial pork products were defined as pork obtained directly from a farm, from home-raised swine, or from wild boar.
Results
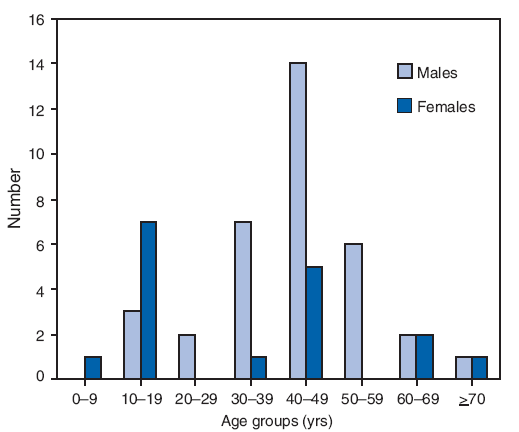
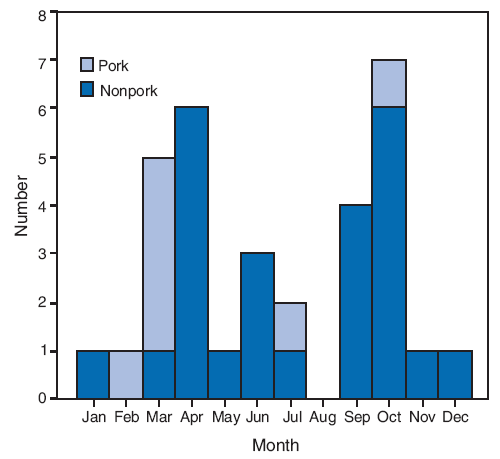
During 2002--2007, a total of 18 states* reported 66 cases of trichinellosis to CDC. Of these 66 cases, 12 (18%) were excluded from analysis; eight did not meet the case definition, two were unaccompanied by case report forms, and two had been included previously in the 1997--2001 surveillance summary. Four states accounted for 31 (57%) cases: California (11 cases), Alaska (10 cases), New York (five cases), and Pennsylvania (five cases). Three states in the West (Alaska, California, and Washington) reported 21 (39%) cases, seven states in the Northeast (Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont ) reported 17 (31%) cases, four states in the Midwest (Michigan, Minnesota, North Dakota, and Ohio) reported 10 (19%) cases, and three states in the South (Florida, Maryland, and Tennessee) reported six (11%) cases (Table 1). Of the 54 cases that were analyzed, 35 (66%) occurred in males and 19 in females. For the 53 (98%) patients whose age was known, the median age was 39 years (range: 2--73 years) (Figure 1). Date of illness onset was known for 42 (78%) patients. Five cases occurred in the winter, 16 in the spring, nine in the summer, and 12 in the fall; for 10 cases, the onset date was known, but the associated meat product was unknown.(Figure 2).
At least one common clinical manifestation was reported by 52 (96%) patients. Myalgia was reported in 38 (70%) patients, eosinophilia in 39 (72%) patients, fever in 29 (54%) patients, and periorbital edema in 15 (28%) patients. Of the 52 patients reporting at least one common sign or symptom, 39 (75%) reported having at least two common signs or symptoms, 22 (42%) reported having at least three common signs and symptoms, and eight (15%) reported having all four common signs and symptoms. The two patients who did not report at least one common sign or symptom of trichinellosis both had positive antibody titers and were associated with outbreaks. Of the total of 54 patients, 25 (46%) reported both date of illness onset and date of consumption of implicated meat. The median incubation period was 18 days (range: 2--61 days). For one case, an incubation time of 1,975 days was reported; this patient was removed from the analysis of the incubation period because the incubation period usually is ≤2 months.
Serologic testing was performed on all 54 patients; 52 (96%) patients were seropositive for Trichinella antibodies. Two patients were seronegative but were associated with outbreaks and had one or more of the common signs and symptoms of trichinellosis. A muscle biopsy reportedly was performed on one patient, but no Trichinella larvae were found.
The source of infection was identified for 43 (80%) patients (Table 2). Of the 43 cases with known source of infection, pork was associated with 10 (23%) cases: seven with commercial pork, two with noncommercial pork, and one with an unknown type of pork. Of the seven cases associated with commercial pork, five were linked to U.S. commercial pork and two to pork consumed while traveling in Asia. The two cases associated with noncommercial pork were linked to wild boar meat: one with wild boar meat from a farm and one with wild boar meat from a farmers' market. Of the 43 cases for which a suspected meat product was identified, nonpork products were associated with 27 (63%) cases; bear meat was associated with 21 (78%) of these cases. Of the six cases not associated with bear meat, two were attributed to consumption of U.S. commercial beef and one each to cougar meat, deer meat, either walrus or seal meat, and either bear or deer meat. Six patients reported consuming both pork and nonpork products, but the infected meat product could not be distinguished.
Implicated meat was positive for Trichinella larvae in eight (67%) of 12 cases. Trichinella larvae were found in U.S. commercial pork consumed by two patients who reported eating pork and bear sausage; no larvae were identified in the bear meat. In six cases, Trichinella larvae were identified in nonpork products: bear meat in five cases and cougar meat in one case.
The method used for cooking the implicated meat was known in 30 (56%) cases, including four cases for which multiple methods were used. Meat was uncooked in five cases, fried in nine cases, cooked over an open fire or barbequed in 11 cases, boiled in five cases, baked in two cases, stir-fried in one case, and microwaved or baked in one case. In three cases, meat was both boiled and fried; and in one case, meat was both boiled and stir-fried. In addition, two patients ate rare or partially cooked meat.
During 2002--2007, six outbreaks involving a total of 16 patients were reported by five states (Table 3). Two outbreaks occurred in Alaska. One outbreak each occurred in California, Minnesota, New York, and Tennessee. Bear meat was implicated in four outbreaks (12 cases), pork in one outbreak (two cases), and an unknown meat source of either pork or deer in one outbreak (two cases).
In April 2002, five cases of trichinellosis in Alaska were associated with consumption of meat from a black bear that had been killed by a hunter in March 2002; the hunter brought three pounds of bear meat to a barbeque at a remote cabin and shared the meat with 10 other persons. Meat from the bear was unavailable for testing. Four patients were seropositive for Trichinella antibodies, and one patient was linked epidemiologically to the barbeque. In September 2003, two cases of trichinellosis in Tennessee were associated with bear meat consumed in August 2003. The bear was hunted, and the meat was cooked over an open fire. Trichinella larvae were found in the bear meat implicated in this outbreak, and both patients were seropositive for Trichinella antibodies. In June 2005, three cases of trichinellosis in Alaska were associated with meat from a bear that one of the outbreak patients killed during a hunting trip. Two patients reported consumption of uncooked bear meat during preparation of sausage. The meat was tested for Trichinella larvae, but no larvae were identified. In October 2006, two cases of trichinellosis in California were associated with consumption of fried meat from a bear killed during a hunting trip during the same month. Trichinella larvae were identified in the bear meat implicated in this outbreak, and both patients were seropositive for Trichinella antibodies. In August 2006, two cases of trichinellosis in Minnesota were associated with the consumption of either commercial pork or hunted deer meat. One child tested positive for Trichinella antibodies during a visit to an allergist for a history of constipation and stomach pain of >1 year. The other five family members were tested subsequently, and one sibling tested positive for Trichinella antibodies. Each year, the family reportedly consumed 50--70 pounds of hunted deer meat mixed with commercial pork. In June 2007, two cases of trichinellosis in New York were associated with consumption of commercial pork. Both patients had tasted the uncooked meat while preparing pork and bear meat sausage. The pork was purchased fresh from a local market, and the bear meat was provided by a friend who had killed the bear during a hunting trip in California. Trichinella larvae were found in the sausage and in the pork but not in the bear meat. Both patients were seropositive for Trichinella antibodies.
Discussion
The number of trichinellosis cases reported in the United States has declined since the U.S. Public Health Service began keeping records on the disease in 1947 (Figure 3). The decrease in the number of cases has mirrored the decline in the prevalence of Trichinella in commercial pork products as a result of changes in swine production practices (3,4). Risk factors for Trichinella infection in swine include feeding of Trichinella-infected waste products, consumption of rodents or other wildlife infected with Trichinella, and cannibalism among pigs within an infected herd (6). During the mid-20th century, laws that required the cooking of all garbage fed to swine were passed in an effort to control porcine vesicular exanthema (1953--1954) and hog cholera (1962) (7); this single change to a long-standing industry practice is thought to have played a major role in the decrease in prevalence of Trichinella in swine that occurred subsequently. In 1980, Congress passed the Federal Swine Health Protection Act (Public Law 96-468), which prohibited feeding potentially contaminated raw garbage to swine. In response to increasing concerns over the safety and biosecurity of the U.S. food supply, many states also have passed regulations that mandate the confinement rearing of swine, prohibit the feeding of all food waste to swine, limit swine exposure to rodents and wildlife, and ensure that dead pigs are removed from a herd immediately.
The National Trichinae Certification Program, incorporated in the 2008 Farm Bill, was adopted after more than a decade of collaboration between U.S. government regulators and the U.S. pork industry to ensure the quality and safety of U.S. pork products (Voluntary Trichinae Certification Program, 9 C.F.R., Part 149 [2009]). Under the program, three U.S. Department of Agriculture (USDA) agencies (the Animal and Plant Health Inspection Service, the Food Safety and Inspection Service, and the Agricultural Marketing Service) collaborate to verify that pork-production sites manage and produce pigs according to the program's required production practices (see Appendix). USDA audits pork production sites by collecting information about the site, pig sources, feed sources, feed-storage methods, rodent and wildlife control practices, carcass-disposal procedures, and facility hygiene. Pork-production sites that feed and house pigs in confinement structures can participate in the program on a voluntary basis and are certified as trichinae-safe if they adhere to sanctioned production practices. USDA also verifies the identity of pork derived from pigs from certified production sites through slaughter and processing to maintain the link between certification and safety of meat available for purchase. Although the U.S. pork industry has been employing good production practices for decades, the lack of a formal safety certification program diminished demand for U.S. pork exports as a result of a perceived risk for infection. Therefore, although participation is voluntary, certification benefits U.S. pork producers by enabling them to compete with other trichinae-safe pork producers in both international and domestic markets. Because modern pork-production systems have all but eliminated Trichinella as a food-safety risk in the United States, the program is a viable alternative to the time-consuming and expensive process of testing each pig carcass at slaughter, which had been required of U.S. pork exports by some large trading partners, including the European Union and Russia.
Cooking, curing, and freezing are methods used to inactivate Trichinella larvae in meats. USDA recommends that consumers of fresh pork cook the product to an internal temperature of 160°F (71°C). Although Trichinella larvae can be killed at temperatures as low as 131°F (55°C), the recommended temperature allows for cooking methods, particularly microwave cooking, that can result in uneven distribution of temperature throughout the meat. Curing, a processing method involving an interaction of salt, temperature, and drying time, is used in the preparation of many pork products (including sausage, ham, and pork shoulder). Although USDA recommends specific curing procedures for the destruction of Trichinella larvae in pork, no curing procedure has been completely effective at inactivating all Trichinella larvae (Prescribed treatment of pork and products containing pork to destroy Trichinae, 9 C.F.R., Sect. 318.10 [2009]) (7).
Sufficient freezing of Trichinella-infected meat will kill the encysted larvae of several Trichinella species; however, some species are resistant to freezing. The freeze-resistant Trichinella species found in the United States have low infectivity and persistence in pigs; therefore, the larval numbers reached in swine are not high enough to cause human trichinellosis, and freezing remains an effective method to control trichinellosis related to pork consumption† (8,9). Conversely, game animals in the United States can be infected with freeze-resistant Trichinella nativa or Trichinella T6, and infective larvae have been identified in frozen game meat in the United States. In 1995, an outbreak of 10 cases in Idaho occurred after ingestion of cougar jerky infected with a freeze-resistant species of Trichinella (10). In 2003, one patient was infected with T. nativa after eating undercooked frozen bear meat from a slaughter house in upstate New York, and two Tennessee patients were infected with a freeze-resistant species of Trichinella after eating frozen meat from a bear hunted and killed in Canada (11). In 2004, freeze-resistant Trichinella larvae were found in a black bear hunted and killed in New Hampshire (12). Hunters and wild-game consumers need to be aware that freezing does not kill all Trichinella larvae in wild game and that all game meat should be properly cooked to an internal temperature of 160°F (71°C) (6).
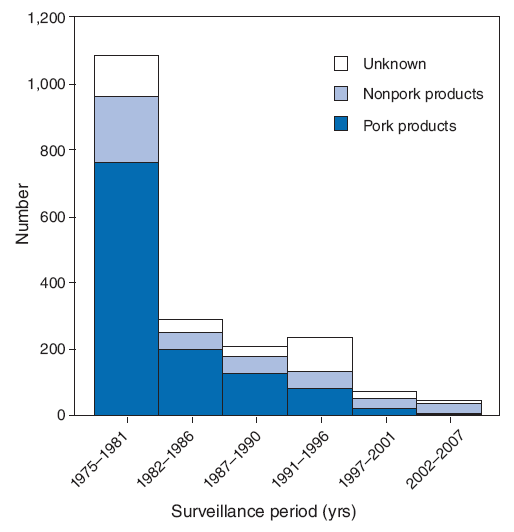
During 1997--2001, the epidemiology of trichinellosis in the United States changed; for the first time, the number of cases associated with the consumption of meat products other than pork (30 cases) surpassed the number of cases associated with pork products (22 cases) (4). During 2002--2007, the number of cases associated with meats other than pork remained greater than the number of cases associated with pork products; the majority of these cases were associated with wild game consumption (Figure 4). Four of the six outbreaks that occurred during 2002--2007 were associated with consumption of wild game, specifically bear meat.
During 2002--2007, more trichinellosis cases were associated with commercial pork products than with noncommercial pork products whereas during 1997--2001, cases linked to noncommercial pork outnumbered those associated with commercial pork products (3). During 2002--2007, five cases were associated with consumption of U.S. commercial pork; Trichinella larvae were identified in the pork associated with two of these cases. Although the commercial pork industry and USDA have taken efforts to ensure the safety of U.S. commercial pork, a low risk for trichinellosis from commercial pork products still exists. In addition, two cases were linked to commercial pork consumed during foreign travel. Many countries have less stringent food safety regulations than the United States, which might lead to a greater risk for acquiring trichinellosis when consuming improperly prepared meat in these countries.
The niche-market popularity of organic and free-range meat products has increased. The number of swine reared in USDA-certified organic livestock operations increased from 482 in 1997 to 10,018 in 2005 (13). Swine reared by these methods spend time outdoors, which is a known risk factor for Trichinella infection (14) because, unlike commercial pigs that are raised in confinement buildings, these swine potentially are exposed to, and thus could consume, the carcasses of Trichinella-infected wildlife. Whether any of the cases linked to U.S. commercial pork described in this report came from organic or free-range producers is unknown, but incorporating questions that would distinguish the type of operation from which the meat originated into standard trichinellosis case interview forms should be recommended to permit examination of the possibility of consumption of pork from swine raised outdoors as a risk factor for trichinellosis.
Because the consumption of Trichinella-infected meat by an animal host is required for transmission of infection, herbivores such as deer and cattle are atypical Trichinella hosts. However, natural and experimental infections have been reported in cattle and deer (15--17), and trichinellosis outbreaks have been reported in Europe as a result of the consumption of undercooked horse meat (18). During 2002--2007, two cases were associated with consumption of commercial beef, one with consumption of deer meat, and one with consumption of either bear or deer meat. As no leftover meat was available for testing in these cases, whether beef and deer meat were the true sources of infection is unknown; the true vehicle of infection might have been overlooked. Determining the source of a sporadic Trichinella infection can be challenging because much time can elapse between initial infection and when the infection is actually diagnosed, particularly in asymptomatic cases. Because detectable Trichinella antibody levels can persist many years after initial infection (19) and previous infections might be diagnosed years later, the true source of Trichinella infection might not be recalled by the patient when a food exposure history is obtained.
Seasonal peaks in trichinellosis in the United States have been reported previously; during 1997--2001, seasonal peaks associated with noncommercial pork products occurred during May--June, and seasonal peaks associated with bear meat occurred during August--September and November--December (3). During 2002--2007, no significant seasonal peaks occurred (Figure 2). However, an increase occurred in the number of cases associated with meat other than pork in April and during September--October. Of the 16 cases associated with meat other than pork during these months, 15 were associated with wild game and one with beef. These cases might be attributable to the consumption of wild game that was hunted during the spring and fall hunting seasons and indicate the importance of game meat in the epidemiology of trichinellosis.
Conclusion
Although changes in pork production and public health education regarding preparation of pork have been successful in reducing the incidence of trichinellosis in the United States, consumption of meat products other than pork continues to be an important source of infection. The change in the epidemiology of trichinellosis in the United States, where infection often is linked to the consumption of game meat, indicates a need to target education messages about trichinellosis to hunters and consumers of wild game, particularly bear. Information about risk for trichinellosis and proper food safety practices should be disseminated to all persons receiving permits to hunt bear or other carnivores and scavengers that are hunted for food. In addition, education messages should be targeted to consumers of pork from wild boar or pigs raised outdoors, and to travelers who might consume improperly cooked meat during international travel. Finally, although the number of cases associated with U.S. commercial pork continues to decline, and the risk for trichinellosis from consumption of this pork is low, public health prevention messages regarding safe pork preparation and cooking practices also should be targeted toward consumers.
References
- Dupouy-Camet J, Kociecka W, Bruschi F, et al. Opinion on the diagnosis and treatment of human trichinellosis. Expert Opin Pharmacother 2002;3:1117--30.
- Gottstein B, Pozio E, Nockler K. Epidemiology, diagnosis, treatment, and control of trichinellosis. Clin Microbiol Rev 2009;22:127--45.
- Roy SL, Lopez AS, Schantz PM. Trichinellosis surveillance---United States, 1997--2001. In: Surveillance Summaries, July 25, 2003. MMWR 2003;52(No. SS-6).
- Gamble HR, Bush E. Seroprevalence of Trichinella infection in domestic swine based on the National Animal Health Monitoring System's 1990 and 1995 swine surveys. Vet Parasitol 1999;80:303--10.
- CDC. Nationally notifiable diseases surveillance system. Atlanta, GA: US Department of Health and Human Services, CDC; 2009. Available at http://www.cdc.gov/ncphi/disss/nndss/nndsshis.htm. Accessed November 19, 2009.
- Gamble HR, Bessonov AS, Cuperlovic K, et al. International Commission on Trichinellosis: recommendations on methods for the control of Trichinella in domestic and wild animals intended for human consumption. Vet Parasitol 2000;93:393--408.
- Gamble HR. Trichinae: pork facts-food quality and safety. Beltsville, MD: U.S. Department of Agriculture, Agricultural Research Service, Parasite Biology and Epidemiology Laboratory; 2001 Available at http://www.aphis.usda.gov/vs/trichinae/docs/fact_sheet.htm. Accessed November 19, 2009.
- Kapel CM, Webster P, Lind P, et al. Trichinella spiralis, T. britovi, and T. nativa: infectivity, larval distribution in muscle, and antibody response after experimental infection of pigs. Parasitol Res 1998;84:264--71.
- Kapel CM, Gamble HR. Infectivity, persistence, and antibody response to domestic and sylvatic Trichinella spp. in experimentally infected pigs. Int J Parasitol 2000;30:215--21.
- CDC. Outbreak of trichinellosis associated with eating cougar jerky---Idaho, 1995. MMWR 1996;45;205--6.
- CDC. Trichinellosis associated with bear meat---New York and Tennessee, 2003. MMWR 2004;53;606--10.
- Hill DE, Gamble HR, Zarlenga DS, et al. Trichinella nativa in a black bear from Plymouth, New Hampshire. Vet Parasitol 2005;132:143--6.
- US Department of Agriculture Economic Research Service, Data Sets. Organic production. Table 5: certified organic livestock. Data on cows, pigs, sheep, chickens and other poultry, by state, 1997 and 2000--2005. Washington, DC: US Department of Agriculture; 2007. Available at http://www.ers.usda.gov/data/organic. Accessed November 19, 2009.
- Gamble HR, Brady RC, Bulaga LL, et al. Prevalence and risk association for Trichinella infection in domestic pigs in the northeastern United States. Vet Parasitol 1999;82:59--69.
- Smith HJ, Snowdon KE, Finley GG, et al. Pathogenesis and serodiagnosis of experimental Trichinella spiralis spiralis and Trichinella spiralis nativa infections in cattle. Can J Vet Res 1990;54:355--9.
- Oksanen A, Oivanen L, Eloranta E, et al. Experimental trichinellosis in reindeer. J Parasitol 2000;86:763--7.
- Moretti A, Piergili-Fioretti D, Grelloni V, et al. Experimental trichinellosis in fallow-deer (Dama dama L.). Parasite 2001;8:S200--2.
- Ancelle T, Dupouy-Camet J, Bougnoux ME, et al. Two outbreaks of trichinosis caused by horsemeat in France in 1985. Am J Epidemiol 1988;127:1302--11.
- Trichinosis: a prospective controlled study of patients ten years after acute infection. Clin Infect Dis 1993;17:637--43.