 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
| Surveillance Summaries |
| September 22, 2000 / 49(SS09);39-62 |
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Influenza, Pneumococcal, and Tetanus Toxoid Vaccination of Adults --- United States, 1993--1997James A. Singleton, M.S.1 1Epidemiology and Surveillance Division AbstractProblem/Condition: An increasing proportion of adults have received recommended vaccinations against influenza, pneumococcal infection, and tetanus. However, in 1995, fewer than 60% of adults were vaccinated as recommended. Reporting Period Covered: 1993--1997. Description of System: Data were obtained from the state-based Behavioral Risk Factor Surveillance System (BRFSS) for 1993, 1995, and 1997 and from the National Health Interview Survey (NHIS) for 1995 to describe national, regional, and state-specific patterns of use of influenza and pneumococcal vaccines and tetanus toxoid among noninstitutionalized adults aged >18 years. Results: Among adults aged >65 years in 1995, 58% reported receiving an influenza vaccination during the previous 12 months, and 34% reported ever receiving a pneumococcal vaccination. In this age group, non-Hispanic whites were more likely to report receipt of influenza (61%) and pneumococcal vaccines (36%) than non-Hispanic blacks (40% and 22%, respectively) and Hispanics (50% and 23%, respectively). Among the 50 states and the District of Columbia, the median vaccination level among older adults (i.e., persons aged >65 years) increased from 51% in 1993 to 66% in 1997 for influenza vaccine, and from 28% in 1993 to 46% in 1997 for pneumococcal vaccine. Adults with chronic medical conditions had low vaccination levels. Those aged 50--64 years were more likely than those aged 18--49 years to report influenza (38% versus 20%) and pneumococcal vaccination (20% versus 12%). In 1995, the proportion of adults who reported receiving a tetanus vaccination during the previous 10 years decreased with age, from 65% among those aged 18--49 years to 54% among those aged 50--64 years and to 40% among those aged >65 years. In each age group, women were less likely than men to report receiving tetanus toxoid; and among adults aged >65 years, Hispanics and Asians/Pacific Islanders were least likely among all racial/ethnic groups to report receiving tetanus toxoid. Interpretation: By 1995, the Healthy People 2000 objective to increase to at least 60% the proportion of persons aged >65 years who had received annual influenza vaccination had been achieved among non-Hispanic whites (objective 20.11). However, substantial improvement is needed among non-Hispanic blacks, Hispanics, and adults aged <65 years with high-risk medical conditions. Public Health Actions: Continued surveillance of vaccine coverage among adults will direct attention to undervaccinated populations that may be disproportionately affected by vaccine-preventable diseases. Vaccination coverage data can be used to guide efforts to increase awareness among health-care providers and the public about the benefits of vaccination, establish systems to ensure that every contact with the health-care system is used to update vaccinations, and further support financial mechanisms to increase vaccine delivery. INTRODUCTIONThe Advisory Committee on Immunization Practices (ACIP) recommends annual influenza vaccination and one dose of pneumococcal vaccine for persons at increased risk for complications from influenza and pneumococcal infections, including all adults aged >65 years and younger adults with chronic conditions (e.g., heart disease, lung disease, or diabetes) (1,2). During 11 of 23 annual influenza epidemics during 1972--1995 in the United States, approximately 20,000 deaths---most among persons aged >65 years---were attributed to complications of influenza (e.g., exacerbation of underlying medical conditions, secondary bacterial pneumonia, or primary influenza viral pneumonia) (1). Of cases of community-acquired bacterial pneumonia that require hospitalization, 25%--35% are caused by Streptococcus pneumoniae, which also causes an estimated 50,000 cases of pneumococcal bacteremia and 3,000 cases of meningitis annually in the United States (2). Of adults with pneumococcal bacteremia, 60%--87% also develop pneumonia, and as many as 40% die (2). Pneumonia and influenza accounted for most of the infectious disease deaths in the United States during 1900--1996 (3) and were the sixth leading cause of death in the United States in 1996 (4). A Healthy People 2000 objective is to increase the proportion of adults who have received influenza and pneumococcal vaccination to at least 60% among persons at high risk for complications from these diseases (objective 20.11) (5). During 1989--1993, the proportion of U.S. adults aged >65 years who reported receiving influenza vaccination during the previous 12 months increased from 33% to 52%; the proportion who reported ever receiving pneumococcal vaccine increased from 15% to 28% (6). In addition to influenza and pneumococcal vaccination, ACIP recommends that all adults receive a primary series of three vaccines containing tetanus toxoid and booster doses of tetanus and diphtheria toxoids (Td) every 10 years (7). A Healthy People 2000 objective is to increase to 62% the proportion of persons up to date with the 10-year tetanus booster (objective 21.2) (8). Since the mid-1940s in the United States, incidence of tetanus has declined steadily, following universal availability of tetanus toxoid (9). During 1995--1997, a total of 124 cases of tetanus (95% in persons aged >20 years) were reported in the United States, with adults aged >60 years at highest risk for severe disease (10). National surveillance for receipt of recommended vaccines by adults is conducted to monitor the performance of vaccination programs, assess progress toward national objectives, and identify populations at high risk for not receiving appropriate vaccinations. In this report, data obtained from the state-based Behavioral Risk Factor Surveillance System (BRFSS) for 1993, 1995, and 1997, and the National Health Interview Survey (NHIS) for 1995, were used to describe national, regional, and state-specific patterns of use of influenza and pneumococcal vaccines and tetanus toxoid among noninstitutionalized adults aged >18 years. METHODSThe data in this report were derived from either NHIS (1995) or BRFSS (1993, 1995, or 1997). NHIS is an ongoing, annual cross-sectional household survey of the U.S. civilian, noninstitutionalized population. In 1995, samples were drawn from each state. Both black and Hispanic persons were oversampled to improve the reliability of estimates for these groups. Responses to three questions were analyzed: "During the past 12 months, have you had a flu shot?"; "Have you ever had a pneumonia vaccination?"; and "During the past 10 years, have you had a tetanus shot?" The estimated prevalence of vaccine receipt for a sample of 17,317 adults aged >18 years was stratified by age. Of these 17,317 persons, 10,826 were aged 18--49 years, 3,023 were aged 50--64 years, and 3,468 were aged >65 years. The questions about vaccination and related medical conditions were asked of one adult sample participant per family in the half of households that were administered the Year 2000 Objectives Supplement. The prevalence of influenza and pneumococcal vaccination among adults aged 18--64 years was estimated for those at high risk for influenza- or pneumococcal-related complications. A total of 1,979 persons were categorized in the high-risk group for influenza-related complications because they reported one or more of the following: diabetes during the previous year; asthma, emphysema, chronic bronchitis, or tuberculosis during the previous year; chronic kidney disease during the previous year; current treatment for any cancer; or ever being told by a physician about having had a heart attack, heart failure, chronic heart condition, or rheumatic heart disease. Persons who were categorized in the high-risk group for influenza-related complications were also included in the high-risk group for pneumococcal-related complications, along with persons who reported liver disease or cirrhosis during the previous year. BRFSS is an ongoing, state-based, random-digit--dialed telephone survey of U.S. noninstitutionalized civilian adults aged >18 years. BRFSS excludes households without telephones; however, only approximately 2.5% of older adults do not have a telephone (11). Data from BRFSS were used to summarize state-specific trends in influenza and pneumococcal vaccination among adults aged >65 years during 1993--1997. Responses to two questions about receipt of vaccinations were analyzed: "During the past 12 months, have you had a flu shot?" and "Have you ever had a pneumonia vaccination?" The estimated prevalence of vaccine receipt was analyzed for survey respondents aged >65 years: 19,761 respondents in 1993; 22,889 in 1995; and 26,469 in 1997. For this report, BRFSS data were aggregated to create annual samples for each of the 50 states and the District of Columbia (DC). Wyoming did not participate in BRFSS in 1993, and the District of Columbia did not participate in 1995. Data were then weighted to account for both the respondent's probability of selection and the distribution of each state's population by age, sex, and race, according to the most recent census or intercensal estimates (12,13). Median vaccination prevalence estimates were based on estimates for the 50 states and the District of Columbia. Overall vaccination prevalence estimates for each of the nine regions used to report weekly cases of nationally notifiable diseases were based on combined data from the states within each region. Overall vaccination prevalence estimates for the 50 states and the District of Columbia combined, presented by age, race/ethnicity, education level, years since last visit to a doctor for a routine checkup, and self-reported health were previously reported (14). For both NHIS and BRFSS, SUDAAN statistical software was used to calculate the prevalence estimates, their standard errors, and 95% confidence intervals (CIs) and to adjust for the complex structure of each survey. SUDAAN was also used to compare NHIS prevalence estimates using chi-square tests and odds ratios. Prevalence estimates are presented only if the ratio of the standard error divided by the prevalence estimate was <0.3, and the denominator comprises at least 30 respondents. The standard of reliability is RSE <0.3 (where RSE = the ratio of the standard error and the prevalence). Estimates that do not meet this standard or with a denominator <30 are not presented. Previously published vaccination data from the 1993 and 1995 BRFSSs included in the denominators those respondents who did not report or did not know their vaccination status. However, in this report, respondents who did not report or did not know their vaccination status were excluded from the analysis; as a result, vaccination prevalence estimates for 1993 and 1995 are slightly higher in this report than in previously published data for the same years (15,16). Institutionalized persons, who accounted for approximately 4% of the population aged >65 years in 1995 (17), are not included in either NHIS or BRFSS. RESULTSInfluenza and Pneumococcal Vaccination of Persons Aged 18--64 Years With High-Risk Medical ConditionsAccording to 1995 NHIS data, the proportion of persons at increased risk for complications from influenza and pneumococcal infections increased with age, from 11% among adults aged 18--49 years to 24% among those aged 50--64 years. Persons aged 50--64 years with one or more high-risk medical conditions were more likely to report receipt of influenza vaccine during the previous year (37.7%) and to report ever receiving pneumococcal vaccine (20.1%) than those aged 18--49 years with one or more high-risk conditions (for influenza, 20.4%; for pneumococcal, 11.8%) (Table 1). Of persons aged 50--64 years with one or more high-risk conditions, non-Hispanic whites were more likely to report receipt of influenza vaccine (40.4%) or pneumococcal vaccine (21.5%) than non-Hispanic blacks (24.5% and 11.7%, respectively) (Table 1). For persons aged 18--49 years, the prevalence of vaccine receipt was similar among racial/ethnic groups, by sex and by education level. In addition, adults aged 18--64 years with one or more high-risk conditions who reported having medical insurance or more frequent contacts with physicians were more likely to report receipt of influenza vaccination (Table 1). Persons aged 18-64 years with one or more high-risk conditions were more likely than those with no high-risk conditions to report receipt of vaccinations (Table 2). Vaccination levels varied among persons with high-risk conditions. Influenza and Pneumococcal Vaccination of Persons Aged >65 YearsOn the basis of 1995 NHIS data, persons aged >65 years were more likely to report receipt of influenza vaccine during the previous 12 months (58.2%) than to report ever receiving pneumococcal vaccine (34.0%). In this age group, vaccination levels were significantly different by race/ethnicity, poverty status, education level, and number of physician contacts during the previous year (Table 1). Vaccination levels were not compared by insurance status because approximately 99% of this population reported having Medicare or another form of medical insurance. Among persons aged >65 years, non-Hispanic whites were more likely to report receipt of influenza (60.7%) and pneumococcal vaccines (35.9%) than non-Hispanic blacks (39.9% and 21.8%, respectively) and Hispanics (49.9% and 23.2%, respectively) (Table 1). Asians/Pacific Islanders were less likely to report influenza vaccination (50.9%) and pneumococcal vaccination (22.4%) than non-Hispanic whites, but these estimates were less reliable because of small sample sizes. The number of older American Indians/Alaskan Natives included in the NHIS sample was not sufficient to allow reliable estimation of vaccination levels. Older persons with incomes at or above poverty level were more likely than those with incomes below poverty level to report vaccination (for influenza, 59.4% versus 50.5%, and for pneumococcal, 35.4% versus 25.3%) (Table 1). Older adults reported frequent contacts with physicians: 89% reported one or more contacts during the previous year, and 34% reported five or more. Influenza and pneumococcal vaccination levels increased as the number of reported physician contacts increased. The greatest percentage difference in frequency of vaccination between groups was observed between persons who reported no physician contact during the previous year and those who reported one or two contacts (for influenza, 32.0% versus 56.4%; for pneumococcal, 17.4% versus 29.9%). Non-Hispanic blacks and Hispanics were as likely as non-Hispanic whites to report at least one physician contact during the previous year (88%--89%) and more likely to report five or more physician contacts during the previous year (38% and 39%, respectively, versus 33%). To determine whether racial/ethnic disparities in vaccination levels among persons aged >65 years persisted after controlling for differences in socioeconomic status and access to health care, further analysis stratified racial/ethnic groups by poverty status, education level, and number of physician contacts during the previous year (Table 3). For each level of these three variables, non-Hispanic whites were more likely than non-Hispanic blacks to report receipt of influenza vaccine. Large disparities between non-Hispanic whites and non-Hispanics blacks were observed for persons with incomes at or above poverty level (61.0% versus 40.9%), having more than a high school education (64.1% versus 43.0%), and reporting five or more physician contacts during the previous year (68.8% versus 44.4%). Disparities between non-Hispanic whites and non-Hispanic blacks were also evident for pneumococcal vaccine among those with incomes at or above poverty level (36.9% versus 22.3%), with more than a high school education (40.8% versus 23.2%), and reporting five or more physician contacts during the previous year (43.9% versus 25.2%). Among persons reporting three or four physician contacts during the previous year, non-Hispanic whites were more likely than Hispanics to report receipt of influenza vaccine (65.5% versus 43.7%). Non-Hispanic whites were more likely to report receipt of pneumococcal vaccine than Hispanics for those with less than a high school education (31.7% versus 17.7%) or with incomes at or above poverty level (36.9% versus 26.5%). Further analysis of vaccination levels among Hispanics was limited by the small number of older Hispanics in the NHIS sample. State-Specific Influenza and Pneumococcal Vaccination of Persons Aged >65 YearsWhen BRFSS data for all reporting areas are combined, in the 50 states and District of Columbia, the median proportion of persons aged >65 years reporting receipt of influenza vaccine during the preceding year increased from 50.8% in 1993 to 60.0% in 1995 and 66.0% in 1997 (Table 4). Similarly, the median proportion of older adults reporting ever receiving pneumococcal vaccine increased from 27.8% in 1993 to 38.4% in 1995 and 45.9% in 1997. These data are similar to those reported by NHIS (14,18). In 50 of the 51 reporting areas, influenza and pneumococcal vaccination levels were higher in 1997 than in 1993 (Wyoming did not participate in BRFSS in 1993). For each vaccine, vaccination levels increased both during 1993--1995 and during 1995--1997 in all but seven of the reporting areas. In 1997, influenza vaccination levels were >70% in nine states: Colorado (74.4%), South Carolina (74.3%), Arizona (72.9%), New Mexico (72.8%), Wyoming (72.4%), Maine (72.1%), Hawaii (71.1%), Missouri (70.3%), and Washington (70.3%). In addition, during this period, pneumococcal vaccination levels were >50% in 17 states, including seven of the nine states with the highest influenza vaccination levels: Arizona (59.4%), Colorado (53.3%), Hawaii (51.7%), Washington (51.6%), Wyoming (50.9%), New Mexico (50.1%), and Maine (50.0%). To assess state-specific variations in vaccination levels among different racial/ethnic populations, data from the 1995 and 1997 BRFSS surveys for each of the 51 reporting areas were combined. Data regarding influenza vaccination coverage among non-Hispanic blacks in 26 reporting areas met the criteria for reliability used in this report. These areas represented 95% of the U.S. non-Hispanic black population aged >65 years as of July 1, 1995. The proportion of older non-Hispanic blacks reporting receipt of influenza vaccine in 1995 or 1997 ranged from 34.5% in Georgia to 60.1% in Nebraska (median: 45.3%) (Table 5). In each of the 26 areas, non-Hispanic whites were more likely than non-Hispanic blacks to report receiving influenza vaccine. Data regarding pneumococcal vaccination coverage among non-Hispanic blacks from 22 states met the reliability criteria; these states represented 84% of the U.S. non-Hispanic black population aged >65 years as of July 1, 1995. The proportion of older non-Hispanic blacks reporting ever receiving pneumococcal vaccine in 1995 or 1997 ranged from 16.2% in South Carolina and Arkansas to 40.1% in Ohio (median: 26.1%). In all states except one (Ohio), non-Hispanic whites were more likely than non-Hispanic blacks to report ever receiving pneumococcal vaccine. After combining data for 1995 and 1997, vaccination levels among older Hispanics could be reliably estimated in nine states; however, these states represented 85% of the U.S. Hispanic population aged >65 years as of July 1, 1995. Influenza vaccination levels were substantially higher in Arizona (71.2%), Colorado (74.2%), and New Mexico (69.3%) than in Florida (44.3%). Influenza vaccination levels among non-Hispanic whites were higher than those among Hispanics in all states except two (Arizona and Colorado). Pneumococcal vaccination levels among Hispanics ranged from 15.8% in Florida to 51.5% in Arizona (median: 32.1%). After combining 1995 and 1997 data for Asians/Pacific Islanders, vaccination levels could be reliably estimated only for California and Hawaii, where 61% of Asians/Pacific Islanders aged >65 years in the United States resided in 1995. Among Asians/Pacific Islanders aged >65 years in California, vaccination levels were 79.1% for influenza vaccine and 49.3% for pneumococcal vaccine; in Hawaii, vaccination levels were 71.6% for influenza and 47.5% for pneumococcal vaccines. After combining 1995 and 1997 data for American Indians/Alaskan Natives, vaccination levels could be reliably estimated only for Alaska and Oklahoma, where 20% of persons aged >65 years in these racial groups resided in the United States in 1995. Influenza vaccination levels were 77.3% in Alaska and 58.8% in Oklahoma; pneumococcal vaccination levels were 56.4% in Alaska and 49.5% in Oklahoma. Tetanus Toxoid Use in Persons Aged >18 YearsIn contrast with the trend for persons who received influenza and pneumococcal vaccines, the proportion of persons in 1995 who reported receiving tetanus toxoid during the previous 10 years decreased substantially with age, from 65.2% among those aged 18--49 to 53.8% among those aged 50--64 years and 39.6% among those aged >65 years (Table 1). In all three age groups, men were more likely than women to report receipt of tetanus toxoid during the previous 10 years. In each age group, Asians/Pacific Islanders were least likely to report receipt of tetanus toxoid compared with other racial/ethnic populations. Among adults aged 18--49 years, Hispanics and non-Hispanic blacks were less likely than non-Hispanic whites to report vaccination (53.2% and 60.5% versus 68.9%). A similar difference in receipt of tetanus toxoid between non-Hispanic whites and non-Hispanic blacks was documented among adults aged 50--64 years. However, among older adults, Hispanics were less likely than non-Hispanic whites to report receipt of tetanus toxoid (28.3% versus 40.8%). Within each of the three age groups, persons with incomes at or above poverty level were more likely than persons with incomes below poverty level to report receipt of tetanus toxoid, and receipt of tetanus toxoid increased as years of education increased. Among persons aged <65 years, those with medical insurance were more likely than those without medical insurance to report receipt of tetanus toxoid. DISCUSSIONAdult Vaccination SuccessesNHIS data indicate that, in 1995, the Healthy People 2000 objective to increase annual influenza vaccination among persons aged >65 years to at least 60% had been achieved among non-Hispanic whites; the overall national coverage level was within 2 percentage points of the objective. In addition, NHIS data indicate that, in 1995, the Healthy People 2000 objective to increase to at least 62% the proportion of adults who are up to date with the 10-year tetanus booster had been achieved among persons aged 18--49 years; the coverage level among persons aged 50--64 years was within 8 percentage points of the objective. Analysis of combined BRFSS data for 1997 from the 50 states and District of Columbia indicates that 65.5% of older persons reported influenza vaccination during the previous 12 months, and 45.4% reported ever receiving pneumococcal vaccine --- the highest levels ever recorded (14). Possible reasons for increases in self-reported influenza and pneumococcal vaccination among persons aged >65 years since 1989 include a) greater acceptance of preventive medical services by practitioners and consumers, b) increased delivery and administration of vaccine by health-care providers and sources other than physicians (e.g., visiting nurse and home-health agencies), c) initiation of Medicare reimbursement for cost of influenza vaccine and its administration in 1993 (19), and d) initiation of Medicare reimbursement for administration of pneumococcal vaccine in 1993 (although authorized in 1981, reimbursement was previously implemented only for the cost of the vaccine) (20). Specific events that might have contributed to greater acceptance and delivery of vaccines include publication of recommendations for adult vaccination (7,21,22); development of standards for adult immunization practice by the National Coalition for Adult Immunization in 1990 (23); establishment of National Adult Immunization Awareness Week (celebrated annually in October) (24); publication of a comprehensive strategy to improve adult vaccination by the Department of Health and Human Services (25); and beginning in 1994, national and state-based campaigns conducted by the Health Care Financing Administration to increase influenza and pneumococcal vaccination coverage among Medicare beneficiaries (26) as well as state and local programs (27,28). State and local health departments have also contributed to the increases in influenza and pneumococcal vaccination coverage (27,28). Vaccination levels among persons aged >65 years in each state and District of Columbia were higher in 1997 than in 1993. In 1997, the Healthy People 2000 national objective for an annual influenza vaccination level of 60% was exceeded by 45 states, and if state-specific coverage continues to increase at rates observed during 1995--1997, a total of 28 states will reach or exceed the 60% objective for pneumococcal vaccination by 2000. Adult Vaccination ChallengesInadequate Influenza and Pneumococcal Vaccination of Adults Aged 18--64 Years With High-Risk Medical Conditions In 1995, influenza vaccination levels for adults with high-risk medical conditions were 22 percentage points below the >60% Healthy People 2000 objective for those aged 50--64 years and 40 percentage points below for those aged 18--49 years. In 1995, pneumococcal vaccination coverage among persons in these two age groups was only slightly higher than half the influenza vaccination coverage level. To improve influenza vaccination levels among adults aged 50-64 years with high-risk medical conditions and in other target groups, the ACIP recently recommended routine annual vaccination of all persons in this age group (1). Inadequate Tetanus Vaccination of Adults Aged >65 Years In 1995, the percentage of adults aged >65 years reporting receipt of tetanus toxoid during the previous 10 years was 22 percentage points below the Healthy People 2000 objective of >62%. Self-reported receipt of tetanus toxoid decreased with increasing age, consistent with patterns of age-specific prevalence of immunity to tetanus in the United States during 1988--1991 (29). Possible reasons for the decline in receipt of tetanus toxoid with increasing age include lack of payment for decennial tetanus boosters by Medicare Part B and missed opportunities for vaccination. To further reduce tetanus morbidity and mortality, increased use of Td is needed, especially among older adults. Inadequate Vaccination of Racial/Ethnic Minority Populations During 1993--1997, racial/ethnic disparities in vaccination coverage of adults aged >65 years continued for non-Hispanic blacks and Hispanics. Non-Hispanic whites were more likely to report influenza and pneumococcal vaccination than non-Hispanic blacks at all poverty levels, education levels, and levels of frequency of contact with health-care providers. State-specific differences in vaccination coverage among Hispanics might reflect socioeconomic and cultural differences of Hispanic subpopulations. More information is needed about racial and ethnic disparities in vaccination coverage in states and local areas, health-care systems, patient and provider barriers to vaccination, and effective interventions to improve vaccination levels. This information will be useful in guiding the President's Initiative to Eliminate Racial and Ethnic Disparities in Health, which seeks to eliminate the health disparities of racial/ethnic minorities in adult (and child) vaccination, breast and cervical cancer screening, diabetes, cardiovascular disease, HIV infections, and infant mortality (30). In this effort, CDC is implementing the Racial and Ethnic Approaches to Community Health (REACH) demonstration projects, which are designed to mobilize communities and organize their resources to support effective and sustainable programs to eliminate health disparities. Pneumococcal vaccination is particularly important for racial/ethnic populations with higher risk for pneumococcal bacteremia and meningitis: Alaskan Natives, some American Indian groups (e.g., Apache), and blacks (2). The relatively high pneumococcal vaccination coverage documented among older American Indians/Alaskan Natives in Oklahoma and Alaska might in part reflect compliance with recommendations for vaccination of these groups. Missed Opportunities to Offer Vaccination In this report, adults who reported more frequent contacts with health-care providers during the previous year were more likely to report vaccination, reflecting increased opportunities for vaccinations to be recommended by providers or requested by patients. Approximately one third of persons aged >65 years or younger adults with high-risk medical conditions reported five or more contacts with health-care providers during the previous year; however, most had not been vaccinated against influenza and pneumococcal disease (except persons aged >65 years receiving influenza vaccine). These data indicate missed opportunities by providers to offer vaccination services. A physician's recommendation for vaccination services can have a strong influence on the patient's decision to be vaccinated (31--33). Recent surveys of physicians have indicated that most were aware of and agreed with vaccination recommendations; the main reason many cited for not delivering vaccines was oversight (34,35). Every contact with the health-care system should be used to review and update vaccination status as needed, including review of indications for pneumococcal vaccine and tetanus toxoid when influenza vaccine is administered. Interventions (e.g., standing orders for vaccination [36], provider reminders and feedback, and patient recalls and reminders) have been effective in increasing adult vaccination levels (37,38). Guidelines and tools for implementing these interventions are available through Put Prevention Into Practice, a nationwide campaign to improve delivery of clinical preventive services (22,39). In addition, opportunities for vaccination at nontraditional health-care settings (e.g., pharmacies, grocery stores, or churches) could be increased to reach persons who do not routinely access traditional health-care settings (36). The findings in this report indicate that influenza vaccination coverage exceeded pneumococcal vaccination coverage. Influenza vaccination campaigns are conducted annually before each influenza season; however, many providers and patients might not be simultaneously reminded about the need for pneumococcal vaccination. Pneumococcal vaccine can be administered concurrently with influenza or other vaccines (by separate injection in different limbs) without an increase in side effects or decreased antibody response to either vaccine (2). When indicated, pneumococcal vaccine should be administered to patients who are uncertain about their vaccination history (2). Opportunities for vaccination of adults aged <65 years could also be increased by incorporating vaccination recommendations in guidelines for clinical care of persons with chronic diseases and conducting campaigns designed to reach persons with chronic diseases (e.g., diabetes) and their health-care providers. The finding that vaccination levels varied by type of chronic condition suggests that physicians in certain specialties might assume more responsibility for vaccination of their patients than other physicians (40). Although >80% of adults aged <65 years with high-risk medical conditions reported having health insurance, influenza and pneumococcal vaccination levels among these insured adults were inadequate in 1995. This finding might reflect lack of coverage of influenza and pneumococcal vaccination services among persons aged <65 years by many health insurance plans. To encourage insurance companies to cover vaccination services, influenza and pneumococcal vaccination of all adults with high-risk medical conditions could be considered for inclusion in health plan performance measures such as the Health Plan Employer Data and Information Set (HEDIS) (41). Influenza vaccination of persons aged >65 years is included in the HEDIS version 3.0, and pneumococcal vaccination of persons aged >65 years has been included in the draft HEDIS 2001, which is available for review at <http://www.ncqa.org/pages/communications/news/h2k1rel.htm>. Need for Enhanced State and Local Surveillance of Vaccination The findings in this report indicate that vaccination coverage among older adults in 1997 and changes in coverage during 1995--1997 varied substantially by state. Multiple factors probably account for these state and regional differences, including physician practice patterns, provision of public health adult vaccination programs, and patient attitudes and access to care. More information is needed at local and state levels about the prevalence of physician recommendations for vaccination, availability of vaccination services in different settings, and consumer barriers to vaccination (31,42,43). This information might assist in identifying effective policies and practices that can be implemented in areas with lower vaccination levels. LimitationsThe findings in this report are subject to at least five limitations. First, self-reported data about receipt of influenza and pneumococcal vaccine were not validated. However, in previous studies that validated self reports by medical record review, the sensitivity of self-reported data regarding influenza vaccination during previous influenza seasons ranged from 92% to 100%, and specificity ranged from 71% to 98% (44,45). For pneumococcal vaccine, a study documented that the sensitivity of self-reported data ranged from 87% to 97%, and specificity ranged from 53% to 76% (45). Second, self-reported data regarding receipt of tetanus toxoid also were not validated. Validation studies have documented contrasting findings. In one study, self-report of the date of last tetanus vaccination was within a year of recorded dates for 18 (82%) of the 22 adult participants (46), and in a study of women in Bangladesh, 40% did not recall receiving tetanus toxoid doses administered 12--23 months before the interview (47). Third, of the persons who reported having any of the pulmonary conditions, those who reported having asthma (which is not an indication for pneumococcal vaccine) could not be distinguished from those who reported having emphysema, chronic bronchitis, or tuberculosis (which are indicators for receiving pneumococcal vaccine). Therefore, the true at-risk population aged <65 years probably is smaller, and the pneumococcal vaccination estimates probably are underestimated. Fourth, after combining 1995 and 1997 BRFSS data for each racial/ethnic population, estimates for many states did not meet the standard of reliability used in this report. Many estimates that met this standard had wide confidence intervals. Combined estimates represent an average of vaccination coverage in 1995 and 1997 and thus may not reflect changes that occurred from 1995 to 1997. Oversampling of racial/ethnic minority populations within states or local areas would provide more reliable estimates. Fifth, not all target groups for influenza and pneumococcal vaccine could be identified by NHIS or BRFSS (e.g., persons with HIV infection). In addition, persons living with or having close contact with persons with high-risk conditions (e.g., persons other than health-care workers) weren't readily identified in either survey. CONCLUSIONSThe substantial reduction in vaccine-preventable diseases, which resulted from increasing childhood vaccination to all-time high levels, has been cited as one of 10 great public health achievements of the 20th century in the United States (9). Similar success can be achieved among the 35 million U.S. adults aged >65 years who should receive annual influenza vaccination and a pneumococcal vaccination, the estimated 33--39 million persons aged <65 years with high-risk conditions who should receive annual influenza vaccination, the 16 million persons aged <65 years with high-risk conditions who should receive a pneumococcal vaccination, and the 202 million adults who should be up to date with tetanus vaccination. National goals for improving prevention of vaccine-preventable diseases among adults include a) increasing the demand for adult vaccination by improving provider and public awareness; b) increasing the capacity of the health-care delivery system to effectively deliver vaccines to adults; c) expanding financing mechanisms to support the increased delivery of vaccines to adults; d) monitoring and improving the performance of the nation's immunization program; and e) enhancing the capability and capacity to conduct research regarding vaccine-preventable diseases in adults, vaccination practices, new and improved vaccines, and international programs for adult vaccination (25,48). Continued efforts will be needed to increase vaccination among older adults during 2000--2010. In Healthy People 2010 (http://www.health.gov/healthypeople/Document/default.htm), objective 14.29 proposes to increase to >90% the proportion of persons aged >65 years (and to >60% the proportion of younger persons with high-risk medical conditions) who are vaccinated against influenza and pneumococcal infections (49). To achieve these objectives, public, private, and community partners must collaborate to implement culturally appropriate and evidence-based interventions to increase vaccine use among all persons at risk for complications from influenza or pneumococcal infections. Timely surveillance of vaccination coverage among adults will focus the attention of public health programs on the undervaccinated populations most likely to suffer disproportionately from vaccine-preventable diseases. AcknowledgmentsThe authors thank Peng-Jun Lu for statistical support and Mary McCauley for her critical review of the manuscript, National Immunization Program. References
Table 1   Return to top. Table 2 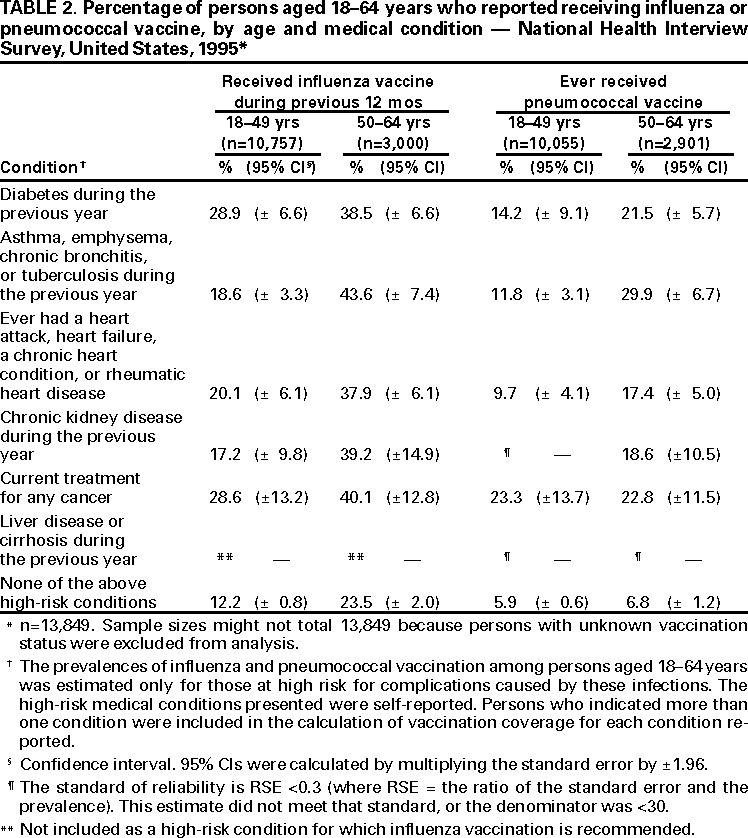 Return to top. Table 3  Return to top. Table 4    Return to top. Table 5    Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 9/12/2000 |
|||||||||
This page last reviewed 5/2/01
|