 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Mold Prevention Strategies and Possible Health Effects in the Aftermath of Hurricanes and Major FloodsPrepared by
The material in this report originated in the National Center for Environmental Health, Agency for Toxic Substances Disease Registry,
Howard Franklin, MD, Director, and the Division of Environmental Hazards and Health Effects, Michael A. McGeehin, PhD, Director.
SummaryExtensive water damage after major hurricanes and floods increases the likelihood of mold contamination in buildings. This report provides information on how to limit exposure to mold and how to identify and prevent mold-related health effects. Where uncertainties in scientific knowledge exist, practical applications designed to be protective of a person's health are presented. Evidence is included about assessing exposure, clean-up and prevention, personal protective equipment, health effects, and public health strategies and recommendations. The recommendations assume that, in the aftermath of major hurricanes or floods, buildings wet for >48 hours will generally support visible and extensive mold growth and should be remediated, and excessive exposure to mold-contaminated materials can cause adverse health effects in susceptible persons regardless of the type of mold or the extent of contamination. For the majority of persons, undisturbed mold is not a substantial health hazard. Mold is a greater hazard for persons with conditions such as impaired host defenses or mold allergies. To prevent exposure that could result in adverse health effects from disturbed mold, persons should 1) avoid areas where mold contamination is obvious; 2) use environmental controls; 3) use personal protective equipment; and 4) keep hands, skin, and clothing clean and free from mold-contaminated dust. Clinical evaluation of suspected mold-related illness should follow conventional clinical guidelines. In addition, in the aftermath of extensive flooding, health-care providers should be watchful for unusual mold-related diseases. The development of a public health surveillance strategy among persons repopulating areas after extensive flooding is recommended to assess potential health effects and the effectiveness of prevention efforts. Such a surveillance program will help CDC and state and local public health officials refine the guidelines for exposure avoidance, personal protection, and clean-up and assist health departments to identify unrecognized hazards. BackgroundOn August 29 and September 24, 2005, hurricanes Katrina and Rita, respectively, made landfall along the Gulf Coast. After both storms, levees were breached, leading to massive flooding in New Orleans and surrounding parishes. The duration of flooding, the extent of flooding, and the number of structures flooded in New Orleans as a result of hurricanes Katrina and Rita in August and September 2005 made the likelihood of massive mold contamination a certainty. Many structures remained flooded for weeks after the hurricane and became saturated with water. An assessment of homes in New Orleans (Orleans Parish) and the surrounding parishes of St. Bernard, East Jefferson, and West Jefferson (excluding the 9th Ward) identified an estimated 46% (>100,000 homes) with some mold contamination; approximately 17% (40,000 homes) had heavy mold contamination (1). Recent parallels to the kind of flooding observed in New Orleans as a result of hurricanes Katrina and Rita occurred in 1997 in Grand Forks, North Dakota, and in 1999 in North Carolina after Hurricane Floyd (2). The number of structures affected was much smaller in North Dakota than in New Orleans, and the population affected in North Carolina was much more dispersed than the population affected in New Orleans. In North Carolina, a reported increase in persons presenting with asthma symptoms was postulated to be caused by exposure to mold (2). In 2001, flooding and subsequent mold growth on the Turtle Mountain reservation in Belcourt, North Dakota was associated with self-reports of rhinitis, rash, headaches, and asthma exacerbation (3). MethodsThis document was initially prepared by CDC as a guide for public health officials and the general public in response to the massive flooding and the anticipated mold contamination of homes and other structures along the U.S. Gulf Coast associated with hurricanes Katrina and Rita (4). A workgroup was convened of CDC staff with expertise in relevant subject areas. This included medical epidemiologists, environmental epidemiologists and occupational epidemiologists, industrial hygienists, infectious disease physicians and mycologists. The framework for the document was decided by consensus discussions, and workgroup members were assigned to research and to write different sections. The members produced individual written summaries, which formed the basis of the report. Wherever possible, recommendations were based on existing recommendations or guidelines. Where adequate guidelines did not exist, the guidelines were based on CDC experience and expertise. This revised version is intended to more broadly address public health concerns related to limiting exposure to mold and identifying, preventing, and managing mold-related health effects following any natural disasters or other occurrences that results in flooding or major water intrusion. Published guidelines, established standards, and the peer-reviewed literature were reviewed to ensure the accuracy and consistency of the recommendations. In addition, the document was sent for stakeholder review and external peer review by experts in the areas of worker protection, general public health, medical, environmental and occupational epidemiology, allergy, industrial hygiene, mycology, and pulmonology. Mold: A DefinitionMolds, mushrooms, mildews, and yeasts are all classified as fungi, a kingdom of organisms distinct from plants and animals. Fungi differ from plants and animals in several respects. Unlike animals, fungi have cell walls. However, unlike plants, which also have cell walls, fungal cell walls are made mostly of chitin and glucan. Fungi cannot produce their own nutrients as plants do through photosynthesis. Fungi secrete enzymes that digest the material in which the fungi are imbedded and absorb the released nutrients. Multicellular fungi do not differentiate into different organs or functional components the way plants and animals do (5). Approximately 100,000 species of fungi exists; fewer than 500 fungal species have been described as human pathogens that can cause infections (5). Visible growth of multicellular fungi consisting of branching filamentous structures (mycelia) are known popularly as molds (5) and are referred to by that term in this report. Molds are ubiquitous in nature and grow almost anywhere indoors or outdoors. The overall diversity of fungi is considerable. For example, the genus Aspergillus has at least 185 known species (6). Molds spread and reproduce by making spores, which are small and lightweight, able to travel through air, capable of resisting dry, adverse environmental conditions, and capable of surviving a long time. The filamentous parts of mold (hyphae) form a network called mycelium, which is observed when a mold is growing on a nutrient source. Although these mycelia are usually firmly attached to whatever the mold is growing on, they can break off, and persons can be exposed to fungal fragments. Some micro-organisms, including molds, also produce characteristic volatile organic compounds (VOCs) or microbial VOCs (mVOCs). Molds also contain substances known as beta glucans; mVOCs and beta glucans might be useful as markers of exposure to molds (7). Some molds are capable of producing toxins (sometimes called mycotoxins) under specific environmental conditions, such as competition from other organisms or changes in the moisture or available nutrient supply. Molds capable of producing toxins are popularly known as toxigenic molds; however, use of this term is discouraged because even molds known to produce toxins can grow without producing them (6). Many fungi are capable of toxin production, and different fungi can produce the same toxin (6). Factors That Produce Mold Growth Although molds can be found almost anywhere, they need moisture and nutrients to grow. The exact specifications for optimal mold growth vary by the species of mold. However, mold grows best in damp, warm environments. The availability of nutrients in indoor environments rarely limits mold growth because wood, wallboard, wallpaper, upholstery, and dust can be nutrient sources. Similarly, the temperature of indoor environments, above freezing and below the temperature for denaturing proteins, can support mold growth, even if the actual temperature is not optimal (8). The primary factor that limits the growth of mold indoors is lack of moisture. Substantial indoor mold growth is virtually synonymous with the presence of moisture inside the building envelope. This intrusion of moisture might be from rainwater leaking through faulty gutters or a roof in disrepair, from a foundation leak, from condensation at an interface (e.g., windows or pipes), or between a cold and a warm environment. Water also can come from leaks in the plumbing or sewage system inside the structure. Studies of mold growth on building materials, such as plywood, have found that mold grows on materials that remain wet for 48--72 hours (8). Flooding, particularly when floodwaters remain for days or weeks, provides an almost optimal opportunity for mold growth. How Persons Are Exposed to Mold Mold exposure can produce disease in several ways. Inhalation is usually presumed to be the most important mechanism of exposure to viable (live) or nonviable (dead) fungi, fungal fragments or components, and other dampness-related microbial agents in indoor environments. The majority of fungal spores have aerodynamic diameters of 2--10 µm, which are in the size range that allow particles to be deposited in the upper and lower respiratory tract (5). Inhalation exposure to a fungal spore requires that the spore be initially aerosolized at the site of growth. Aerosolization can happen in many ways, ranging from disturbance of contaminated materials by human activity to dispersal of fungi from contaminated surfaces in heating, ventilating, and air-conditioning (HVAC) systems. Fungal spores also can be transported indoors from outdoors. Overall, the process of fungal-spore aerosolization and related issues (e.g., transport, deposition, resuspension, and tracking of fungi to other areas) are poorly understood. Persons can be exposed to mold through skin contact, inhalation, or ingestion. Because of the ubiquity of mold in the environment, some level of exposure is inevitable. Persons can be exposed to mold through contact with airborne spores or through contact with mycelial fragments. Exposure to high airborne concentrations of mold spores could occur when persons come into contact with a large mass of mold, such as might occur in a building that has been flooded for a long time. Exposure to mycelia fragments could occur when a person encounters a nutrient source for mold that has become disrupted, such as would occur during removal of mold-contaminated building material. Skin contact or exposure by inhalation to either spores or mycelial fragments also could occur in a dusty environment, if the components of dust include these fungal elements. For the majority of adverse health outcomes related to mold exposure, a higher level of exposure to living molds or a higher concentration of allergens on spores and mycelia results in a greater likelihood of illness. However, no standardized method exists to measure the magnitude of exposure to molds. In addition, data are limited about the relation between the level of exposure to mold and how that causes adverse health effects and how this relation is affected by the interaction between molds and other microorganisms and chemicals in the environment. For this reason, it is not possible to sample an environment, measure the mold level in that sample, and make a determination as to whether the level is low enough to be safe or high enough to be associated with adverse health effects. Persons affected by major hurricanes or floods probably will have exposure to a wide variety of hazardous substances distributed by or contained within the floodwater. This report does not provide a comprehensive discussion of all such potential hazards; such situations will of necessity require case by case evaluation and assessment. Guidance has been provided by CDC for such issues in a number of documents, including NIOSH Hazard Based Interim Guidelines: Protective Equipment for Workers in Hurricane Flood Response (9) and the CDC guidance: Protect Yourself From Chemicals Released During a Natural Disaster (10). Factors That Cause Disease from Mold Numerous species of mold cause infection through respiratory exposure. In general, persons who are immunosuppressed are at increased risk for infection from mold (11). Immunosuppression can result from immunosuppressive medication, from medical conditions and diseases that cause immunosuppression, or from therapy for cancer that causes transient immunosuppression. Although certain species of mold cause infection (5,8,11), many mold species do not cause infection. Infections from mold might be localized to a specific organ or disseminated throughout the body. Many of the major noninfectious health effects of mold exposure have an immunologic (i.e., allergic) basis (6). Exposure to mold can sensitize persons, who then might experience symptoms when re-exposed to the same mold species. For sensitized persons, hay fever symptoms and asthma exacerbations are prominent manifestations of mold allergy (6). Although different mold species might have different propensities to cause allergy, available data do not permit a relative ranking of species by risk for creating or exacerbating allergy. In addition, exposure to beta glucans might have an inflammatory effect in the respiratory system (12). Prolonged exposure to high levels of mold (and some bacterial species) can produce an immune-mediated disease known as hypersensitivity pneumonitis (13). Clinically, hypersensitivity pneumonitis is known by the variety of exposures that can cause this disorder (e.g., farmer's lung, woodworker's lung, and malt worker's lung). Ingesting toxins that molds produce can cause disease. Longterm ingestion of aflatoxins (produced by Aspergillus species) has been associated with hepatocellular cancer (14). In addition, ingestion of high doses of aflatoxin in contaminated food causes aflatoxicosis and can result in hepatic failure (11). Whether concentrations of airborne mold toxins are high enough to cause human disease through inhalation is unknown, and no health effects from airborne exposure to mold-related toxins are proven. General GuidelinesAssessing Exposure to MoldExposure Assessment Any structure flooded after hurricanes or major floods should be presumed to contain materials contaminated with mold if those materials were not thoroughly dried within 48 hours (15,16). In such cases, immediate steps to reduce the risk for exposure to mold are likely to be of greater importance than further exposure assessment steps presented below. Assessing the level of human exposure to mold in flooded buildings where mold contamination is not obvious is often a central and ongoing activity in recovery related to hurricanes and floods. Understanding the strengths and limitations of the approaches that are available to assess such exposures is important. Buildings that were not flooded could also have mold. For example, buildings with leaking roofs or pipes, which allows water to penetrate into biodegradable building materials, or excessive humidity, particularly buildings built with biodegradable materials, are susceptible to mold growth (2). Visual Inspection and Moisture Assessment A visual inspection is the most important step in identifying possible mold contamination (17,18). The extent of any water damage and mold growth should be visually assessed. This assessment is particularly important in determining remedial strategies and the need for personal protective equipment (PPE) for persons in the contaminated area. Ceiling tiles, gypsum wallboard (sheetrockTM), cardboard, paper, and other cellulosic surfaces should be given careful attention during a visual inspection. Not all mold contamination is visible (9,16); with a flood, contamination in the interior wall cavities or ceiling is common. A common means of assessing the mold contamination of a building is to estimate the total square feet of contaminated building materials (9,18,19). However, professional judgment will necessarily play an important role in the visual inspection because less quantifiable factors (e.g., location of the mold, building use, and function) and exposure pathways are also important in assessing potential human exposure and health risks. Ventilation systems also should be visually checked, particularly for damp filters, damp conditions elsewhere in the system, and overall cleanliness. To avoid spreading microorganisms throughout the building, HVAC systems known or suspected to be contaminated with mold should not be run. Guidelines from the U.S. Environmental Protection Agency (EPA) and CDC (20,21) provide useful information concerning this topic. Different algorithms for assessing and remediating mold-contaminated buildings are available. Examples of such algorithms are available from the U.S. Army (22), the New York City Department of Health (18), and OSHA (23). Moisture meters provide qualitative moisture levels in building materials and might be helpful for measuring the moisture content in a variety of building materials (e.g., carpet, wallboard, wood, brick, and concrete) following water damage (9,17). Meters also can be used to monitor progress in drying wet materials. Damaged materials should be removed and discarded. Moisture meters are available from contractor tool and supply outlets. Humidity meters can be used to monitor indoor humidity. Inexpensive (<$50) models that monitor both temperature and humidity are available. A borescope is a hand-held tool that allows users to see hidden mold problems inside walls, ceiling plenums, crawl spaces, and other tight areas (6,18). No major drilling or cutting of dry wall is required. Sampling for Mold Sampling for mold is not part of a routine building assessment (9,16,18,19). In most cases, appropriate decisions about remediation and the need for PPE can be made solely on the basis of visual inspection. If visible mold is present, then it should be remediated regardless of what types of microorganisms are present, what species of mold is present, and whether samples are taken. Other than in a controlled, limited, research setting, sampling for biologic agents in the environment cannot be meaningfully interpreted and would not substantially affect relevant decisions about remediation, reoccupancy, handling or disposal of waste and debris, worker protection or safety, or public health. If sampling is being considered, a clear purpose should exist. For example:
Types of Samples. Types of samples used to assess the presence of mold and the potential for human exposure to mold in a water-damaged building include air samples, surface samples, bulk samples, and water samples from condensate drain pans or cooling towers. Detailed descriptions of sampling and analysis techniques have been published (6,17). Among the types of samples, airborne sampling might be a good indicator of exposure from a theoretical point of view, particularly for assessing acute short-term exposures. However, in practice, many problems (e.g., detection problems and high variability over time) limit the usefulness of these types of samples for most biologic agents. If air sampling is conducted, personal measurements best represent the current exposure, although practical constraints might make personal sampling difficult. Therefore, area sampling is the most commonly performed type of air sampling used to assess bioaerosol exposure despite resultant uncertainty about how accurately the measurements reflect actual personal exposure. One type of surface sampling is the sampling of settled dust. A theoretical advantage of settled-dust sampling is the presumed correlation of concentrations of fungi in the settled dust with chronic exposure to those fungi (17). However, surface sampling is a crude measure and will yield a poor surrogate for airborne concentrations (6,17). Results of surface sampling as a measure of exposure should be interpreted with caution. Bulk samples can provide information about possible sources of biologic agents in buildings and the general composition and relative concentrations of those biologic agents. Assessment of Microorganisms. Two distinct approaches are used for evaluation of the presence of specific microbes: culture-based and nonculture-based. The strengths and limitations of the different approaches have been published (6). Instead of measuring culturable or nonculturable fungi or fungal components, constituents or metabolites of microorganisms can be measured as a surrogate of microbial exposure. Examples of such techniques include polymerase chain reaction (PCR) technologies and immunoassays (6,17). Methods for measuring microbial constituents (with some exceptions) are in an experimental phase and have not yet been routinely applied in clinical assessments, risk assessments, or epidemiologic studies. No health-based standards (e.g., OSHA or EPA standards) or exposure limits (e.g., NIOSH recommended exposure limits) for indoor biologic agents (airborne concentrations of mold or mold spores) exist. Differences in season; climatic and meteorological conditions; type, construction, age, and use of the building and ventilation systems; and differences in measurement protocols used in various studies (e.g., viable versus nonviable microorganism sampling, sampler type, and analysis) make it difficult to interpret sampling data relative to information from the medical literature (6,17). If sampling is performed, exposure data can be evaluated (either quantitatively or qualitatively) by comparing exposure data with background data, indoor environments with outdoor environments, or problem areas with nonproblem areas. A quantitative evaluation involves comparing exposures, whereas a qualitative evaluation could involve comparing species or genera of microorganisms in different environments. Specifically, in buildings without mold problems, the qualitative diversity of airborne fungi indoors and outdoors should be similar. Conversely, the dominating presence of one or two kinds of fungi indoors and the absence of the same kind outdoors might indicate a moisture problem and degraded air quality. In addition, the consistent presence of fungi such as Stachybotrys chartarum, Aspergillus versicolor or various Penicillium species over and beyond background concentrations might indicate a moisture problem that should be addressed (17). Indoor and outdoor mold types should be similar, and indoor levels should be no greater than levels outdoors or in noncomplaint areas (17). Analytical results from bulk material or dust samples also might be compared with results of similar samples collected from reasonable comparison areas. Other Issues Biomarkers For biologic agents, few biomarkers of exposure or dose have been identified, and their validity for exposure assessment in the indoor environment is often unknown. Testing to determine the presence of immunoglobulin E (IgE) to specific fungi might be a useful component of a complete clinical evaluation in the diagnosis of illnesses (e.g., rhinitis and asthma) that can be caused by immediate hypersensitivity (17,24). Testing is usually done by in vitro tests for serum specific IgE, or by skin prick or puncture tests. Detection of immunoglobulin G (IgG) to specific fungi has been used as a marker of exposure to agents that might cause illnesses such as hypersensitivity pneumonitis (17,24). However, the ubiquitous nature of many fungi and the lack of specificity of fungal antigens limit the usefulness of these types of tests in evaluating possible building-related illness and fungal exposure (17,24). Specific serologic tests (e.g., tests for cryptococcal antigen, coccidioidal antibody, and Histoplasma antigen) are useful in the diagnosis of some fungal infections, but these are the exception. The routine clinical use of immunoassays as a primary means of assessing environmental fungal exposure or health effects related to fungal exposure is not recommended. Health-care providers whose patients express concern about the relation between symptoms and possible exposure to fungi are advised to use immunoassay results with care and only in combination with other clinical information, including history, physical findings, and other laboratory results (24). Mycotoxins In recent years, increased concern has arisen about exposure to specific molds that produce substances called mycotoxins. Health effects related to mycotoxins are generally related to ingestion of large quantities of fungal-contaminated material (17). No conclusive evidence exists of a link between indoor exposure to airborne mycotoxin and human illness (6,25). Many molds can potentially produce toxins given the right conditions (6,11,17). Some molds that produce mycotoxins are commonly found in moisture-damaged buildings; research related to the importance of these findings is ongoing. Although the potential for health problems is an important reason to prevent or minimize indoor mold growth and to remediate any indoor mold contamination, evidence is inadequate to support recommendations for greater urgency of remediation in cases where mycotoxin-producing fungi have been isolated. Summary The interpretation of environmental sampling data generally requires professional judgment, and medical conclusions cannot be made based solely on the results of analysis of environmental sampling. In the context of mold growth following a major hurricane or flood, mold growth itself and the extent of growth based on a thorough visual inspection is sufficient to categorize a building as moldy or not moldy. This should provide sufficient information for action and no additional characterization is needed. Clean-up and PreventionThe most effective way to eliminate mold growth is to remove it from materials that can be cleaned and to discard materials that cannot be cleaned or are physically damaged beyond use (9,18,19,26--30). Persons with respiratory conditions, allergies, asthma, or weakened immune systems should avoid mold cleanup if possible or seek the advice of their doctor and determine what type of personal protective equipment is appropriate. Appropriate PPE (e.g., tight-fitting NIOSH-approved N-95 respirator, gloves to limit contact of mold and cleaning solutions with skin, and goggles) (13,26--30) should be used when performing clean-up or other activities in mold-contaminated homes or buildings after a flood. Clean-up Removing mold problems requires a series of actions (6,9,16). The order of these actions is sometimes important (6), but might vary on a case-by-case basis. Typically, the following actions are taken regardless of whether a problem is small and simple or large and complex:
For small, simple problems, the entire list of tasks can be done by one person. Large, complex problems might require many persons from different professions and trades. For circumstances that fall between those extremes, some combination of occupant action and professional intervention will be appropriate. In general, no single discipline brings together all the required knowledge for successful assessment and remediation. Returning to Mold-Contaminated Homes or Buildings After a Flood When persons return to homes or buildings after a flood, they should take the following steps (6,9,16,26--30):
Removing and Cleaning Up Mold in a Building For cleaning mold covering <10 square feet in an area flooded by clean water, detergent and water might be adequate (9,16). However after hurricanes and major floods, flood water is likely to be contaminated and, in this setting, mold can be removed with a bleach solution of 1 cup chlorine bleach per 1 gallon of water (26--30). Never mix bleach or bleach-containing products with ammonia or ammonia-containing products. If water damage is substantial or mold growth covers >10 square feet, consult the EPA guide, Mold Remediation in Schools and Commercial Buildings (15). Some companies specialize in water damage restoration and can assess the issues involved in cleaning up homes after a flood. Two professional trade groups that might be able to help locate such an expert are the Association of Specialists in Cleaning and Restoration (http://www.ascr.org) and the Institute of Inspection, Cleaning, and Restoration Certification (http://www.iicrc.org). Contractors used for remediation should have experience in cleaning mold. Check references and ask the contractor to follow the recommendations in the guidelines of the American Conference of Governmental Industrial Hygienists (ACGIH) or other guidelines from professional organizations or state agencies. Contact your state health department's website for information about state licensing requirements for contractors in your state. Examples of websites from states that have recently dealt with natural disasters include http://www.tdh.state.tx.us/beh/mold (Texas) and http://www.lslbc.louisiana.gov (Louisiana). Cleaning Clothes, Textiles, or Stuffed Animals Ensure that laundry is washed in safe water. Use only water that is properly disinfected or that the authorities have stated is safe. Take the appropriate steps to make sure that use of gas or electric appliances is safe. Before using a washing machine that was in a flooded building, run the machine through one full cycle before washing clothes. Use hot water and a disinfectant or sanitizer. Take clothes and linens outdoors and shake off any dried mud or dirt before washing them. Hose off muddy items to remove all dirt before putting them in the washer. If the items are only wet, they can be laundered normally. Check the labels on clothes and linens and wash them in detergent and warm water if possible, or take them to a professional cleaner. Adding chlorine bleach to the wash cycle will remove most mildew and will sanitize the clothing. However, bleach might fade some fabrics and damage other fabrics. If the label reads "dry clean only," shake out loose dirt and take the item to a professional cleaner. Consult a remediation professional for advice on whether heavily mold-contaminated items made of leather, suede, or a similar material are salvageable or should be discarded. Do not burn or bury textiles that cannot be cleaned. Put them into properly sealed plastic bags and dispose of them as you would normal household garbage in your area. Salvaging Household Items When assessing or remediating mold contamination to a house, homeowners or clean-up personnel might decide to repair or clean household items (e.g., housewares or kitchen items) damaged or contaminated by flood waters. As with clothing and other textiles, make sure the water being used is safe. Use only water that is properly disinfected or that the authorities have stated is safe. Nonporous items (e.g., dishes, pots, glass items, and hard plastic items) can be salvaged. However, because floodwaters are contaminated, nonporous items should be washed by hand in a disinfectant and then air-dried. Do not use a dish towel. Porous items (e.g., cloth, some wood and wood products, and soft plastic) must be discarded because they probably absorbed whatever contaminants were in the floodwaters. Before using the dishwasher, clean and disinfect it. Then use a hot setting to wash your pots, pans, dishes, and utensils. Do not use the energy-saving setting. Throw away canned foods that are bulging, opened, or damaged. Food containers with screw-caps, snap-lids, crimped caps (soda pop bottles), twist caps, flip tops, snap-open, and home-canned foods should be discarded if they have come into contact with floodwater because they cannot be disinfected. If intact cans have come in contact with floodwater or storm water, remove the labels, wash the cans, and dip them in a solution of 1 cup of bleach in 5 gallons of water. Relabel the cans with a marker. Cleaning a Heating, Ventilating, and Air Conditioning System All surfaces of an HVAC system and all its components that were submerged during a flood are potential reservoirs for dirt, debris, and microorganisms, including bacteria and mold. In addition, moisture can collect in areas of HVAC system components that were not submerged (e.g., air supply ducts above the water line), and this also can lead to the growth of microorganisms. Therefore, all flood water-contaminated and moisture-laden components of the HVAC system should be thoroughly inspected, cleaned of dirt and debris, and disinfected by a qualified professional. CDC has prepared recommendations for professionals to help ensure that floodwater-contaminated HVAC system components are properly cleaned and remediated (21). If HVAC systems are not properly cleaned and disinfected to prevent the dissemination of mold and other debris throughout a building, bioaerosols of mold and other microorganisms might exists and can cause a variety of adverse health effects to the building's occupants. Ensure that the HVAC system is shut down before any remedial activities. Prevention After the Flood Limited scientific information exists on the efficacy and impact of prevention strategies. In addition, little of the practical knowledge acquired and applied by design, construction, and maintenance professionals has been subject to thorough validation (6). No generally accepted health-based standards exist for remediation (6). If property owners decide to make extensive repairs or completely rebuild after a flood, they might consider designing and building in a way that will limit the potential for future mold growth (6,30). The key to prevention of mold is to eliminate or limit the conditions that foster microbial growth by limiting water intrusion and the nutrients that allow mold to grow (6,9,16,30). The two basic approaches are to keep moisture-sensitive materials dry and to use materials that are not easily biodegradable or which offer a poor substrate for mold growth. Personal Protective EquipmentWorkers and their employers might be required to wear or provide protection to minimize exposure to mold. Workers and employers should refer to pertinent OSHA standards and NIOSH guidelines. Information also is provided for the public. Minimizing exposure to mold involves using PPE and administrative and engineering controls (6,17,18,31,32). Administrative controls include identifying mold-contaminated areas promptly, restricting access to these areas, and minimizing aerosol generating activities (e.g., by suppressing dust) (3,6,18,27,29,32). Engineering controls include ventilating mold-contaminated areas adequately and using heavy equipment with sealed positive pressure, air-conditioned cabs that contain filtered air recirculation units to protect the workers (6,17,18,31,32). Misting contaminated materials with water is a control measure used to reduce dust levels during debris removal. Workers should wear PPE regardless of the engineering controls used, especially for skin and eye protection (1,9,17,18,32). Primary functions of PPE in a mold-contaminated environment are prevention of the inhalation and ingestion of mold and mold spores and prevention of mold contact with skin or eyes (1,32). PPE requirements for workers are likely to differ from the PPE recommendations for homeowners or other building occupants who are less likely to disturb and aerosolize contaminated materials. In addition, PPE recommendations for persons with underlying illness or compromised immune systems will differ from PPE recommendations for healthy persons. Proper training or instruction in the use of protective equipment is essential for effective use. Guidelines for protection of and training recommendation for workers have been published (33). Types of Personal Protective Equipment Skin and Eye Protection Gloves keep the hands clean and free from contact with mold (9,29). Gloves also protect hands from potentially irritating cleaning solutions (29,32,33). Long gloves that extend to the middle of the forearm are recommended. The glove material should be selected on the basis of the type of substance or chemical being handled. When using a biocide (e.g., chlorine bleach) or a strong cleaning solution, gloves made from natural rubber, neoprene, nitrile, polyurethane, or PVC are needed. When using a mild detergent or plain water, ordinary household rubber gloves can be used. Latex or nonlatex medical examination gloves should be used if hands are likely to be in contact with infectious materials. Persons with natural rubber latex allergy should not use natural rubber latex gloves and should consult the NIOSH Alert on latex gloves for further information (34). To protect eyes, properly fitted goggles or a full face-piece respirator are needed. Goggles must be designed to prevent the entry of dust and small particles. Safety glasses or goggles with open vent holes are not appropriate in mold remediation. CDC has published guidelines on this topic (35). Protective Clothing When conducting building inspections and remediation work, workers or homeowners might encounter hazardous biologic agents and chemical and physical hazards. Consequently, appropriate personal protective clothing, either reusable or disposable, is recommended to minimize cross-contamination between work areas and clean areas, to prevent the transfer and spread of mold and other contaminants to street clothing, and to eliminate skin contact with mold or chemicals (9,32). In hot environments, precautions to prevent dehydration and heat stress when wearing protective clothing (e.g., drink plenty of water) are needed. Disposable PPE should be discarded after it is used. Such equipment should be placed into impermeable bags and usually can be discarded as ordinary construction waste. Protective equipment for biocide applicators (e.g., goggles or face shield, aprons or other protective clothing, gloves, and respiratory protection) must be selected on the basis of the product manufacturer's warnings and recommendations. In addition, the manufacturer's recommended precautions should be followed. Reusable protective clothing, including respiratory equipment (36,37), should be cleaned according to manufacturers' recommendations for PPE exposed to mold and other potentially hazardous chemicals (e.g., bleach and biocides). Respiratory Protection Inhalation is the primary exposure route of concern related to mold for workers, homeowners, and building occupants (6,9,17,18). When administrative and engineering controls are not adequate to eliminate airborne exposure to mold (or dust containing mold), respirators provide additional protection from inhalation of airborne mold, contaminated dust, and other particulates that are released during dust-generating processes (e.g., remediation work or debris removal) (6,9,17). Respirators provide varying levels of protection. Selecting a respirator to minimize exposure to molds should be based on a qualitative assessment because quantitative data on mold-contaminated environments are not informative (38--41). All decisions about respirator selection should be made with knowledge of the relative protective capabilities and the advantages and disadvantages of different respirators. Further discussion of respirator selection is available (38--41). Standard surgical or dust masks are intended for use only as barriers against large particles and do not provide protection against many airborne particles (38). Respirators used to protect persons from airborne contaminants (including mold and mold spores) must be certified by CDC's NIOSH. In addition, as specified by the OSHA respiratory protection standard (37), workers whose employers require them to use respirators must be properly trained, have medical clearance, and be properly fit-tested before they use the respirator. If a worker must use respirators, the worker's employer must develop and implement a written respiratory protection program with worksite-specific procedures and elements. Additional information on respiratory protection is available from OSHA (37,42,43). PPE Guidelines for Workers in Mold-Contaminated Areas Outdoors Exposure to some level of airborne mold is inevitable because molds are found indoors and outdoors (6,17). However, demolishing or cleaning heavily mold-contaminated materials outdoors can lead to excessive exposure to mold. The level of exposure to mold outdoors is primarily based on the amount of mold-contaminated material, the amount of mold in the material, and the type of work being performed. The need for PPE (including respiratory, skin, and eye protection) for outdoor workers requires ongoing professional assessment that considers the potential for exposure to mold and the potential for exposure to other hazardous substances that might be in the outdoor work area. Indoors Guidelines summarized below are based on guidelines from OSHA (37,42,43), EPA (13), and the New York City Department of Health and Mental Hygiene (18). These guidelines recommend particular respirators on the basis of the size of the area of mold contamination. However, the size criteria are based on general professional judgment and practicality because data are limited related to the extent of contamination to the frequency or severity of health effects. When determining the potential for airborne exposure to mold and the need for PPE, the size of the area is not the only criterion to be considered. The activities being performed in relation to the mold-contaminated materials are at least as important. Therefore, ongoing professional judgment always must play a part in decisions concerning PPE. For example, any remediation or other work that disturbs mold and causes mold spores to become airborne increases the degree of respiratory exposure. Actions that tend to disperse mold include breaking apart moldy porous materials such as wallboard; destructive invasive procedures to examine or remediate mold growth in a wall cavity; removal of contaminated wallpaper by stripping or peeling; and using fans to dry items or ventilate areas. In addition, health status and other characteristics of the persons potentially exposed to mold also might need to be considered (Table 1). Category I Protection
For use while cleaning the following:
Category II Protection
For use while cleaning the following:
These guidelines should be followed according to professional judgment. For example, more protective respirators might be required if toxic contaminants such as asbestos or lead are encountered during cleanup. All workers dealing with large areas of contamination should be properly trained to handle hazardous materials. PPE Guidelines for the Public (Nonworkers) in Residences and Nonoccupational Settings Clean-up, Debris Removal, or Similar Activities The activities (and possible exposure to mold) of persons re-entering their homes or working outside might be similar to those of workers. Preventing the creation of dust and limiting exposure to dust are the best ways to minimize exposure to mold (1,9,18). For example, using wet mops or vacuums with HEPA filters instead of dry sweeping dust and debris will decrease the amount of dust in the air (1,9,18). If building occupants, residents, or anyone must be around mold-contaminated dust, respirators will offer some protection. Particulate respirators (such as NIOSH-certified N-95 respirators) can be purchased in safety supply stores and in most home improvement stores. Several factors are required for respirators to provide protection from inhalation hazards (15,38,41,43):
A properly worn disposable respirator requires that:
For the Public Not Involved in Clean-up, Debris Removal, or Similar Activities Persons not involved in activities that disturb mold-contaminated materials have a lower risk for inhalation exposure relative to persons performing those types of activities. Persons collecting belongings, visually inspecting homes or buildings, or doing basic clean-up for short periods in a previously flooded home or building will not usually need to use a respirator. For the Public Unable to Use PPE or at High Health Risk from Exposure to Mold The effect of exposure to mold varies widely. Persons who might be affected to a greater extent than the majority of healthy adults include (5,6,9):
Persons with special health concerns should consult their health-care provider if they are concerned about mold exposure. Symptoms that might seem related to mold exposure might have other causes, such as bacterial or viral infections or other allergies. The level of risk associated with exposure activities and the potential benefit of recommended PPE are unknown for pregnant women, persons aged >65 years, and children aged <12 years; exposure-reducing behavior and respiratory protection might be difficult for children aged <12 years. Using respirators or other PPE might increase health risks for persons with underlying health conditions. Persons who have trouble breathing while using a respirator should stop working and contact a doctor or other medical provider (1). For persons at potentially increased health risks from exposure to mold, persons of unknown or uncertain risk, or persons unable to use respirators, caution is recommended when entering heavily mold contaminated environments, particularly when mold clean-up is occurring. Persons in these categories should avoid such situations if possible. Potential Health Effects of Fungal ContaminationIn recent years, the health effects of exposure to mold in built environments have been a subject of intense public concern. These concerns and how they are approached will have important implications for the reconstruction and rehabilitation of cities in states affected by major hurricanes or floods. Many clinical conditions could be caused by the fungal contamination associated with flooding after major hurricanes or floods. Predicting what might occur is speculative. However, many of these conditions are uncommon and will be recognized only if there is a high clinical index of suspicion (Table 2). Anticipating what medical problems could be associated with post-flood fungal contamination might help in preventing them by identifying susceptible populations and making recommendations for reducing potentially harmful exposures. Although this report focuses on potential health effects of fungal contamination, other exposures are also of concern. For example, dampness favors proliferation of dust mites and microorganisms such as bacteria (44,45) and nontuberculous mycobacteria (46). Endotoxins (components of the cell walls of Gram-negative bacteria) have strong inflammatory properties (6,44,45,47--49). Moisture also can release chemical constituents from building materials (6). Standing water supports rodent and cockroach infestations (15,44,45) and proliferation of mosquitoes (30). Fecal contamination of the environment raises concerns about protozoal and helminthic parasites (50). Fungi are not the sole potential cause of many conditions discussed in this report, and these conditions are only a subset of the conditions of concern to clinicians and public health professionals dealing with the aftermath of major hurricanes or floods (51). Overview of Fungal-Induced Diseases Fungi can cause a variety of infectious (52--58) and noninfectious conditions (6,44,45,47,59,60). Several basic mechanisms can underlie these conditions, including immunologic (e.g., IgE-mediated allergic), infectious, and toxic (6). Several of these mechanisms contribute to pathogenesis of a fungal-induced disease. The types and severity of symptoms and diseases related to mold exposure depend in part on the extent of the mold present, the extent of the person's exposure, and the susceptibility of the person (e.g., persons who have allergic conditions or who are immunosuppressed are more susceptible than those without such conditions). Molds produce a variety of volatile organic compounds (6,7,60), the most common being ethanol (61), which are responsible for the musty odors associated with fungal growth. Exposure to moldy indoor environments is also associated with a variety of upper and lower respiratory tract symptoms (6). Institute of Medicine Report on Damp Indoor Spaces and Health In recent years, the issue of how damp indoor spaces and mold contamination affect human health has been highly controversial. In response, CDC commissioned the Institute of Medicine (IOM) to perform a comprehensive review of the scientific literature in this area. The resulting report (6) was published in 2004 and remains the most current and authoritative source of information on this subject. The IOM categorized its findings into four categories:
"Inadequate or insufficient evidence to determine whether an association exists" does not rule out the possibility of an association. Rather, it indicates that no studies examined the relation or that published study results were of insufficient quality, consistency, or statistical power to permit a conclusion about an association. No conditions exists for which the IOM found sufficient evidence of a causal relation with mold or with damp indoor spaces. Several of the conditions are of particular interest to those engaged in the response to major hurricanes or floods (Table 3). Sufficient evidence links upper respiratory tract symptoms (e.g., nasal congestion, sneezing, runny or itchy nose, and throat irritation) to damp indoor environments and mold (with exposure to mold often determined by self-report). Similarly, sufficient evidence exists for a link with the lower respiratory tract symptoms of cough and wheeze. Sufficient evidence also was found for a link between damp indoor environments, mold, and asthma symptoms in sensitized persons with asthma. Evidence also is sufficient for an association between mold exposure and hypersensitivity pneumonitis in a small proportion of susceptible persons, invasive respiratory and other fungal infections in severely immunocompromised persons, and fungal colonization of the respiratory tract or infection in persons with chronic pulmonary disorders. IgE-Mediated Diseases Caused by Fungi IgE-mediated, or allergic, responses underlie the most common types of diseases associated with exposure to fungi (6,45,47,48,49). Atopy, or the genetic predisposition to form IgE responses to aeroallergens, is an important risk factor (45,47,48,49). Clinical conditions associated with allergies include allergic rhinitis and asthma (6,45,47,48,49). Allergic rhinitis is often associated with allergic conjunctivitis and sinusitis (45,47,49). Symptoms of allergic rhinitis include sneezing; itching of the nose, eyes, mouth, or throat; nasal stuffiness; clear rhinorrhea; and, if associated with allergic conjunctivitis, red, itchy eyes. If associated with sinusitis, persons also might complain of sinus fullness or postnasal drip, often purulent (47--49). Signs on physical examination include pale, boggy nasal mucosa; nasal obstruction; and conjunctival redness. Examination of nasal scrapings or secretions indicates eosinophilic inflammation (47--49). If appropriate allergy prick skin testing reagents or in vitro tests for serum specific IgE are conducted, they demonstrate specific IgE-sensitization to causative allergens (45,47--49). Skin testing reagents and blood tests documenting IgE-sensitization to molds are, with few exceptions, poorly standardized and of unclear sensitivity and specificity (45). The conventional hierarchy of treatment is avoidance of exposure to inciting agents; pharmacotherapy with antihistamines, decongestants, or anti-inflammatory agents (e.g., nasal steroid sprays); or, as a last resort, allergen immunotherapy (47--49). Immunotherapy with fungal allergenic extracts is, with a few exceptions, of unknown efficacy (47). Asthma is a disease characterized by episodic, reversible airways obstruction and eosinophilic airways inflammation (45,47--49,62,63). Over time, chronic asthma can lead to airways remodeling and irreversible airways obstruction (45,47--49,62,63). Persons with asthma often have symptoms such as chest tightness, wheezing, dyspnea, or cough (45,47--49,62,63). Physical examination during active asthma might indicate wheezing, but results of examinations between attacks are most often normal (62,63). If performed during an active asthma attack, spirometry most often indicates obstruction that reverses with inhalation of a bronchodilator (62,63). Persons with asthma generally exhibit bronchial hyperreactivity to methacholine challenge (45,47--49,62). However, a small proportion of persons without asthma and a substantial proportion of persons with airway disorders, including chronic obstructive pulmonary disease (COPD), also might exhibit hyperreactivity to inhaled methacholine (49); therefore, test results must be considered together with other clinical information (47--49,62,63). Approaches to demonstrating specific IgE sensitization to molds and limitations of available methods are as described for allergic rhinitis (45,47--49). Asthma is associated with airways inflammation that can be demonstrated by examining induced sputum for eosinophils or measuring exhaled nitric oxide (47), but these tests are often not performed in clinical settings. Comprehensive guidelines for the staging and treatment of asthma are provided by the National Institutes of Health (62,63). Identifying and avoiding triggers, including occupational triggers, is a critical element of treatment. It is important to identify persons with asthma triggered by materials in flood-damaged areas so avoidance measures can be taken. Drug treatment of asthma consists of symptom controllers such as bronchodilators and anti-inflammatory agents (e.g., corticosteroids or leukotriene antagonists) (47--49,62,63). The role of allergen immunotherapy with most fungal agents in treatment of asthma is unclear (48). Therapy with monoclonal anti-IgE is a recently developed treatment option that can be used in carefully selected patients when other, less expensive modalities fail to reduce dependence on systemic corticosteroids (63). The exacerbation of symptoms of asthma is consistently associated with damp buildings (6). If persons with asthma must engage in activities within damp or mold contaminated buildings, their asthma should be well controlled before entering these buildings, and those around them should be aware of the signs of asthma symptoms. The onset of symptoms while in damp moldy environments, especially while wearing PPE, should be an indication to leave the area and to seek appropriate medical care. Allergic Diseases Associated With Airways Colonization Allergic bronchopulmonary aspergillosis (ABPA) is a disease that can occur when the airways of persons with obstructive pulmonary diseases (e.g., asthma or cystic fibrosis) become colonized with Aspergillus fumigatus or other Aspergillus species (6,17,45,47--49). Inflammatory responses lead to additional airways damage. Marked worsening of existing asthma is a typical presentation of ABPA. Symptoms include recurrent episodes of bronchial obstruction, fever, malaise, expectoration of brownish plugs, peripheral blood eosinophilia, hemoptysis, and sometimes asymptomatic pulmonary consolidation. Other features include immediate skin test reactivity to Aspergillus spp. antigens, precipitating serum antibodies to A. fumigatus, markedly elevated serum total IgE, fleeting lung infiltrates, and central bronchiectasis (45,47--49). Criteria for diagnosis have been published (45,47--49). Airways colonization with other fungal species can result in a similar clinical picture. Although no known relation exists between levels of exposure to Aspergillus spp. and development of ABPA, clinicians should suspect and evaluate for the condition when appropriate. Allergic fungal sinusitis (AFS) is typically noninvasive and occurs in allergic, immunocompetent patients (6,45,47--49): most have asthma, and 85% have nasal polyps (47). Invasive fungal sinusitis can occur in patients who are immunocompromised with illnesses such as diabetes, hematologic malignancies or immunosuppressive treatments or chronic steroid therapy (6,47). Fungal colonization is associated with a characteristic allergic mucin containing high levels of eosinophils (6,45,47--49). The mere presence of fungi in the nasal passages is not indicative of an active infection. Hypersensitivity Pneumonitis Hypersensitivity pneumonitis (HP), also known as extrinsic allergic alveolitis, is a granulomatous interstitial lung disease (6,17,45,47--49). A wide range of materials, including fungi, can be inhaled and thus sensitize susceptible persons by inducing both antibody and cell-mediated immune responses (6,17,45,47--49). Re-exposure of sensitized persons leads to lung inflammation and disease (6,17,45,47--49). Building-related HP caused by fungi and bacteria has been well documented (6,17). Usually, only a small fraction of those with a given exposure develop HP; therefore, poorly understood host factors play an important role in disease pathogenesis (6,47--49). The presentation of HP is complex and can be either acute, subacute, or chronic (6,47,48). The acute form is often associated with heavy exposures and characterized by chills, fever, malaise, cough, and dyspnea appearing 4--8 hours after exposure (6,47,48) and is often confused with pneumonia. The chronic form is thought to be induced by continuous low-level exposure. Onset generally occurs without chills, fever, or malaise and is characterized by progressive shortness of breath with weight loss (47,48). Chronic HP can be confused with idiopathic pulmonary fibrosis or other forms of interstitial lung disease (47,48). The diagnosis of HP, especially the chronic form or when presentation is mild, is often missed early in the course of the disease. If it does occur in the aftermath of major hurricanes or floods, a high degree of clinical suspicion is required for detection. In general, when HP is suspected, a clinical and exposure history should be performed. Patients should be asked about their possible exposure to damp and water-damaged areas, farms, birds, hot tubs, and other environments that might cause HP. Environmental sampling for the presence of microorganisms known to cause HP and serologic testing for circulating precipitins can help to establish causative exposures (47--49). Chest imaging using chest radiographs or high-resolution computed tomography scanning of the thorax, lung-function tests, broncholaveolar lavage, and lung biopsy all have roles in diagnosis (47--49). Although established criteria exist for the diagnosis of hypersensitivity pneumonitis (64,65), in the setting of a documented post-disaster HP outbreak, a noninvasive approach to identifying cases could be more appropriate and cost-effective than requiring conventional diagnostic testing. A recent, large multicenter study indicated that under conditions of low or high prevalence, six predictors could be used in combination for noninvasive diagnosis of HP (66):
Optimal treatment is elimination of causative exposures. The IOM report (6) provides information about management of building-related HP that is relevant to reoccupation of structures contaminated by fungi after major hurricanes or floods. Such management includes giving standard medical therapy (e.g., systemic corticosteroids and removing sources of fungal contamination from the environment). In some cases, if efforts to remove mold from a building are unsuccessful in relieving symptoms, the patient might need to move to another home or office. Inhalation Fevers Inhalation fever is a general name given to a variety of influenza-like, self-limited syndromes that might be caused by a variety of stimuli. Two types of inhalation fevers are of potential concern after major hurricanes or floods. Humidifier fever is characterized by fever, respiratory symptoms, and fatigue with onset within hours after exposure to contaminated humidification systems (6,17,45,47). Obtaining a supportive history is critical to diagnosis. Thermophilic actinomycetes; other bacteria, including species of Legionella and Pseudomonas; and protozoa have been associated with humidifier fever (17). Aerosolized endotoxin derived from Gram-negative bacteria has an important role in this condition (17,47). Although humidifier fever can be confused with acute HP, it is a short-term ailment and removal from exposure is effective treatment (17,47). Humidifier fever is thought to represent a nonspecific inflammatory response to exposure (17,47). Organic dust toxic syndrome (ODTS) has been reported among workers in a variety of agricultural and industrial settings and is thought to involve inhalation exposure to materials with heavy microbial contamination (67--69). Etiologic exposures that cause ODTS are often a poorly defined mixture of substances, including fungi, bacteria, and microbial constituents such as endotoxin (67--69). ODTS is characterized by fever and influenza-like symptoms, including general weakness, headache, chills, body aches, and cough occurring 4--12 hours after heavy exposure to organic dust (67--69). Dyspnea also is sometimes present. Results of chest auscultation and chest radiographs are usually normal (67,68). The peripheral white blood count is often elevated during attacks. Accurate patient history is critical for making a correct diagnosis. Although the symptoms resemble those of acute HP, they are not caused by response of the immune system to a specific antigen in the environment (67,68). ODTS poses a risk for workers performing renovation work on building materials and is a realistic concern for workers handling heavily contaminated materials in the aftermath of major hurricanes or floods. ODTS is best prevented by minimizing exposure through engineering controls, administrative controls, and respirators (69). For agricultural workers handling organic dusts, CDC recommends using the most practical respirator with the highest assigned protection factor. Toxic Effects of Fungi Certain common molds can produce metabolites with a wide range of toxic activities such as antibiotic (e.g., penicillium), immune-suppressive (e.g., cyclosporine), carcinogenic (e.g., aflatoxins), emetic, and hallucinogenic (e.g., ergot alkaloids) (6,11,17,59). Mycotoxins are fungal metabolites that poison humans and animals. Although ingestion is the most common route of exposure, inhalation and dermal contact also are exposures of concern (6,11,17,59). Mycotoxin production is dependent not only on species and strain of mold, but also on environmental conditions (e.g., temperature, water activity, light) and growth substrate (11,17). Thus, the presence of toxin-producing mold species does not necessarily indicate whether mycotoxins are present. Mycotoxins were prematurely proposed as the cause of a disease outbreak of eight cases of acute pulmonary hemorrhage/hemosiderosis in infants in Cleveland, Ohio, in 1993 and 1994 (70). The cluster was attributed to exposure to mycotoxins produced by Stachybotrys chartarum. Subsequent reviews of the evidence concluded that insufficient information existed and no such association was proven (71). Almost all of the known effects of mycotoxin exposures are attributable to ingestion of contaminated food (72). Health effects from inhalational exposures to toxins are not well documented. IOM found inadequate or insufficient evidence for a link between exposure to damp indoor environments and molds with a variety of conditions that have been attributed to toxicity (6) (Table 3). Certain case studies of agricultural and remediation workers have described adverse health effects such as skin irritation, skin necrosis, cough, rhinitis, and bloody nasal exudate after inhaling or touching materials with heavy fungal contamination (73--76). Whether these effects resulted from exposure to mycotoxins or from a general overload of organic material is unknown. No commercial clinical diagnostic tools are available to determine whether a person's health effect is related to exposure to mycotoxins. Because of the lack of information about noningestion mycotoxin exposure and adverse health effects in humans, precautions should be taken when handling heavily contaminated building materials. Fungal Infections No reports of increased fungal infections related to floods in the United States exist. However, anecdotal case reports of fungal infection after floods include Apophysomyces elegans wound infection in a man who sustained traumatic injuries after the southeast Asian tsunami in December 2004 (77). A. elegans belongs to the Zygomycetes class of fungi. Infections are most commonly seen in immunocompromised and diabetic patients, and rarely in immunocompetent persons. The cause of infection in immunocompetent persons is usually cutaneous trauma with direct implantation of fungal organisms into the wound from soil contamination (78). Theoretically, infection with fungal species that contaminate buildings, building constituents, and the environment after major hurricanes or floods is a potential concern. In general, persons with impaired host defenses (especially if impaired because of cell-mediated immunity or neutropenia) suffer the most severe types of fungal infections (6,52,53) (Table 4). However, invasive fungal infections also can occur in persons with normal host defenses and, in certain situations, can be life threatening (52,53) (Table 5). Persons at greatest risk for invasive fungal infection from heavy fungal contamination after major hurricanes or floods are those with impaired host defenses (6,52,53) (Table 4). Any impairment in cell-mediated immunity or neutropenia (e.g., human immunodeficiency virus [HIV] infection, leukemia, lymphoma, and diabetes mellitus) increases risk for many types of invasive fungal infections (52,53). Severely immunosuppressed persons, such as solid-organ or stem-cell transplant recipients or those receiving cancer chemotherapy agents, corticosteroids, or other agents inhibiting immune function, are at much higher risk for locally invasive infections of the lungs, sinuses, or skin and systemic infections (52,53). Aspergillus spp., zygomycetes, and Fusarium spp. are particularly important problems (52,53,56). These serious infections are often fatal, even with aggressive antifungal therapy (52,53,56). Protective measures, such as HEPA filtration, implemented during periods of extreme susceptibility to invasive fungal infections are well established and effective in hospitals (79). However, preventive measures outside the hospital are less well established. Current guidelines emphasize the importance of avoiding areas of high dust (e.g., excavation sites, building construction or renovation sites, chicken coops, and caves) and factors associated with fungal infections (e.g., foods that increase a person's risk for fungal exposure) (80). Obstructive pulmonary diseases such as asthma, cystic fibrosis, and COPD, might predispose persons to airway colonization with Aspergillus spp. (6,17,45,47--49). Inflammatory host responses to colonization can lead to ABPA (6,17,45,47--49,52). Aspergillus spp. also can cause invasive or semi-invasive infection in persons with COPD, especially in those being treated with corticosteroids. Chronic necrotizing pulmonary aspergillosis is an indolent condition observed in persons with underlying lung disease (53). Colonization of lung cavities (e.g., tuberculosis cavities or emphysematous blebs) by Aspergillus spp. can cause pulmonary aspergillomas (fungus balls) (6,52), which are conglomerations of Aspergillus spp. hyphae matted together with fibrin, mucus, and cellular debris. These often do not cause symptoms, but they can be associated with hemoptysis (52,53). An exposure-response relation has never been established linking levels of exposure to Aspergillus spp. with development of any of these conditions. Therefore, to what degree exposure to fungal contamination after major hurricanes or floods would increase any risk is unclear. However, despite unknown benefit, persons with clinically significant obstructive pulmonary diseases (e.g., asthma, cystic fibrosis, COPD), and persons with cavitary lung disease from conditions such as tuberculosis should avoid airborne exposure to materials that have become heavily contaminated with fungal growth in the wake of major hurricanes or floods. Persons with normal host defenses also are subject to fungal infections (52,53) (Table 5), and persons with impaired host defenses can acquire any of these, often with greater severity. Ocular, skin, and superficial infections occur in those with normal host defenses and range from the relatively common (e.g., ringworm, athlete's foot) to the relatively rare (e.g., sporotrichosis) (52,53). Of particular relevance in areas with fungal contamination after major hurricanes or floods are organisms that cause localized skin and superficial infections following traumatic inoculation with soil and plant saprophytes, which are found in air, soil, and plant materials. For example, Scedosporium apiospermum (Pseudallescheria boydii) can be recovered from polluted water, sewage, swamps, and poultry or cattle manure (52,53,55,58). Although rare in the United States, this organism can cause a soft tissue infection called Madura foot, a mycetoma in which the draining sinuses show white grains containing fungal elements. This organism also can produce septic arthritis or osteomyelitis after penetrating trauma. Sporothrix schenckii is a dimorphic fungus that produces soft tissue infections after traumatic inoculation from a contaminated environmental source (52,53), such as sphagnum moss, roses, plant seedlings, and other vegetation. Lymphocutaneous lesions are the hallmark of sporotrichosis, as the organisms spread through the local lymphatics after primary inoculation. A high degree of clinical suspicion is needed to diagnose the less common, locally invasive fungal infections. Diagnosis is made by histopathology and culture after biopsy of the affected lesion. Histopathology must be performed to verify that a recovered isolate is the cause of disease and not an environmental contaminant. Culture must be performed to identify the agent correctly. Fungal isolates are identified in a clinical mycology laboratory. Exposures that result in invasive pulmonary mycoses in persons with normal host defenses are generally thought to occur outdoors where active disturbance of a reservoir has occurred (52,53). The mode of transmission is inhalation of fungal spores. Person-to-person transmission of pulmonary mycoses does not occur (53). Diseases relevant to flood prone areas such as the Gulf Coast states include histoplasmosis and blastomycosis. Histoplasmosis is unlikely to be increased as a result of fungal contamination after major hurricanes or floods. The condition is caused by Histoplasma capsulatum, a dimorphic fungus found in soil enriched with the droppings of birds and bats (52,53). Areas with endemic disease in the United States include the Mississippi and Ohio River valleys, but cases have occurred in other parts of the United States. Many persons develop no symptoms when exposed to H. capsulatum in an endemic setting. Blastomycosis is a potential problem after major hurricanes or floods in areas with endemic disease because it can cause serious disease even in those with normal host defenses (52,53). Blastomycosis is caused by the dimorphic fungus Blastomyces dermatitidis (52,53). The organism is found in moist soil, frequently along streams or rivers enriched with decaying vegetation. In the United States, the organism is most commonly found in states surrounding the Mississippi and Ohio rivers (52,53). An area in Louisiana about 70 miles from New Orleans has endemic blastomycosis (81). In Louisiana, cases occur at an incidence of about 1--10 per year, mostly in the area of Washington Parish where the condition is endemic (81). Outbreaks have been associated with manipulation of decaying vegetation or recreational activity near lakes or rivers (53). The incubation period is not certain but, on the basis of data from outbreaks, appears to be about 45 days (82), ranging from weeks to months. The clinical spectrum of blastomycosis includes asymptomatic infection, acute or chronic pneumonia, and disseminated disease (52,53). Pulmonary infection can mimic acute bacterial pneumonia or tuberculosis with progression to acute respiratory distress syndrome. Alveolar infiltrates, mass lesions that mimic bronchogenic carcinoma, and fibronodular interstitial infiltrates are the most common radiographic findings (52,53). Disseminated blastomycosis often appears as ulcerative skin lesions with multiple necrotic bone lesions in the vertebrae, skull, or long bones (52,53). Culture of lesions or histopathologic evidence from infected tissue is required for diagnosis of blastomycosis (52,53). Direct microscopy of pus, scrapings from skin lesions, or sputum showing thick-walled broad-based budding yeast cells 5--15 µm in diameter supports a presumptive diagnosis of blastomycosis and might, in the appropriate clinical setting, prompt the initiation of antifungal therapy (52,53). Serologic tests can be performed on serum from patients showing signs of suspected pulmonary blastomycosis or with suggestive skin lesions. A positive immunodiffusion (ID) test, showing a precipitin band with the Blastomyces A antigen, is highly specific for the disease and does not require paired serum samples (52,53). However, the sensitivity is poor (33%--88%), so a negative ID test does not rule out the disease (52,53). For cases with negative results, the test should be repeated in 3--4 weeks after the initial sampling. The complement fixation (CF) test for blastomycosis has poor sensitivity and specificity. Fungal brain abscesses are uncommon in healthy persons (52,53,57). The primary infection results from inhalation of infectious conidia from the environment; the route of infection appears to be hematogenous dissemination from the lungs (52,53,57). Of particular interest after major hurricanes or floods is S. apiospermum (P. boydii) (52,53,57). Many case reports document patients with focal neurologic defects caused by multiple brain abscesses weeks or months after nearly drowning. The organism apparently spreads hematogenously after initial aspiration of sewage-laden water (from floods, lagoons, or bayous) into the lungs. Near drowning presumptively results in a massive inoculation of mold into the lungs. Preventing Adverse Health Effects From Environmental Fungal Contamination After Major Hurricanes or Floods Persons should reduce their exposure to molds as much as possible (with the realization that fungi are ubiquitous). Persons with underlying or induced immunosuppressed conditions or diseases caused by immune sensitization to fungal constituents present in mold growth should be especially careful to reduce exposure. If exposure to heavily mold-contaminated materials is unavoidable, persons should use appropriate administrative, engineering, and personal protection controls. Because a person's likelihood of developing adverse health effects from mold exposure depends on the type of exposure and on individual susceptibility, precautionary measures need to be customized. Recommended measures are based on professional judgment because of lack of available scientific evidence. For example, no research studies have evaluated the effectiveness of personal protective equipment in preventing illness from mold exposure. Total avoidance of heavily contaminated buildings or other high exposure situations is suggested for persons with specific underlying conditions such as profound immunosuppression. Respiratory protection, dermal protection, and occlusive eye protection recommendations are customized to various populations and exposure-associated activities. Repeated or prolonged exposure probably poses a greater health risk than do exposures of a similar intensity, but short duration. Preventive precautions are especially important for persons who expect to be highly exposed for a long time. Public Health Strategies and Recommendations for State and Local OfficialsRecommendations from CDC are for protecting and monitoring the health and safety of workers and residents who enter, repair, or destroy flooded buildings. The recommendations are focused on limiting human exposure to mold and other microbial agents and preventing any adverse health effects related to such exposure. Several factors are assumed:
Assessing Exposure to Mold Exposure assessment is usually a critical step in determining whether persons are exposed to a hazard at a level that could have an adverse health effect. The mere presence of a chemical or biologic hazard in the environment is insufficient to create a public health hazard. The contaminant must be present in an environmental medium (e.g. air, water, food, and dust) that allows it to come in contact with persons and move along a biologic pathway (e.g., inhalation, ingestion, and absorption). In addition, the concentration of the contaminant must be sufficient to create a biologic response that leads to an adverse health outcome. Mold and its spores exist in damp materials. Disturbing mold releases potentially hazardous particulates into the air, which can then be drawn into the sinuses and lungs. Although molds also might directly attack the skin or openings in the skin, the most common route of exposure is through the air and into the body by inhalation. Environmental sampling for molds has limited value and, in most instances, is not needed after major hurricanes or floods. Exposure Assessment Building interiors should be assumed to be substantially contaminated with mold in the following circumstances:
Exposure to materials and structures contaminated with mold should be assumed to present a potential health risk regardless of the type of mold. Risk for illness does not necessarily vary with the type of mold or the extent of contamination. Preventing Excessive Exposure to Mold Preventing excessive exposure to mold is the best way to avoid harmful health consequences. The preferred approach to preventing mold exposure is to prevent water from infiltrating a building or damaging household goods and structures. After major hurricanes or floods, substantial water damage and mold growth might occur in many buildings. If left undisturbed, mold is generally not a hazard, and most persons will not be adversely affected by moderate exposure to mold. However, in the aftermath of a major hurricane or flood, remediation activities within buildings will disturb any mold that is growing and lead to exposure. To prevent excessive exposure to mold in contaminated areas that are disturbed, persons who enter those areas should implement environmental controls (e.g., suppression of dust and isolation of the contaminated area), use PPE, or both. Preventing human exposure to mold and health effects from such exposure depends on three factors:
Four methods for preventing exposure to mold can be used in combination:
Avoidance Persons The following persons should avoid mold-contaminated environments entirely:
The following persons might be able to tolerate limited exposure, but they should consult with their physicians and should consider avoiding areas where moldy materials are disturbed:
Places All buildings with extensive mold contamination require remediation before rehabilitation. Remediation includes structural repairs to prevent additional water intrusion, removal of mold-contaminated materials that cannot be adequately cleaned and decontaminated, and cleaning and decontamination of mold-contaminated materials that can withstand such treatment. Health-care facilities and other locations that house highly susceptible persons require special attention. These facilities must be adequately remediated before being occupied by highly susceptible persons. Guidelines for remediating health-care facilities include:
Use of Environmental Controls Examples of environmental controls include isolation or containment of the contaminated area, ventilation of the area, and suppression of dust in the area (e.g., by wet-mopping the mold-contaminated surfaces to reduce airborne mold concentrations). Certain methods of isolation can be used to minimize mold exposure. For example, workers operating heavy equipment during the demolition and removal of mold-contaminated materials can be isolated in sealed, positive-pressure, air-conditioned cabs that contain filtered air recirculation units. Another method of isolation is sealing off of mold-remediation areas in occupied, mold-contaminated buildings. However, such isolated areas must also be adequately ventilated. Preventing the creation of dust and limiting exposure to dust are essential to minimizing exposure to mold. When cleaning up dust, workers should use wet mops or vacuums with HEPA filters instead of dry sweeping. Use of PPE Respirators Inhalation is the primary exposure route of concern related to mold for workers, homeowners, and building occupants. Environmental controls are sometimes inadequate to control airborne exposure to mold or dust containing mold. In such cases, respirators protect persons from inhaling airborne contaminated dust and other particulates released during dust-generating processes (e.g., clean-up or debris removal). Recommendations on when to wear a respirator depend on the severity of mold contamination, whether the person's activity is such that mold or particles containing endotoxin or other microbial agents are likely to be released into the air, and the person's health status (Table 1). The following recommendations are made with the assumption that extensive mold contamination is present. Respiratory Protection Recommendations for use of respirators in include:
Guidelines for respiratory protection use:
Eye Protection and Protective Clothing Eye protection is warranted for workers cleaning up mold-contaminated areas and for persons with health conditions that place them at high health risk (Table 1). To protect eyes, a full face-piece respirator or properly fitted goggles designed to prevent the entry of dust and small particles should be used. Safety glasses or goggles with open vent holes are not appropriate during mold remediation. The CDC/NIOSH publication Eye Safety: Emergency Response and Disaster Recovery, provides further information on this topic (35). While conducting building inspections and remediation work, persons might encounter hazardous biologic agents and chemical and physical hazards. Consequently, appropriate personal protective clothing, either reusable or disposable, is recommended to minimize cross-contamination between work areas and clean areas, to prevent the transfer and spread of mold and other contaminants to street clothing, and to eliminate skin contact with mold and chemicals. In hot climates, wearing protective clothing might increase risk for dehydration or heat stress, and special precautions to avoid these conditions (e.g., drink plenty of water) might be needed. Hygiene Disposable PPE should be discarded after it is used. Such equipment should be placed into impermeable bags and usually can be discarded as ordinary construction waste. Appropriate precautions and protective equipment for biocide applicators should be selected on the basis of the product manufacturer's warnings and recommendations (e.g., goggles or face shield, aprons or other protective clothing, gloves, and respiratory protection). Reusable protective clothing should be cleaned according to the manufacturers' recommendations after the product has been exposed to mold. Hands should be washed with clean potable water and soap after gloves are removed. General Distribution of PPE Health officials should consider whether their agencies should supply PPE to residents who might not otherwise be able to acquire the necessary equipment. Providing PPE to the local population would require substantial resources and a mechanism for distributing them. Clean-up Mold-Contaminated Areas
Mold Removal The procedure to remove mold from hard surfaces that do not soak up water (i.e., nonporous) is as follows:
Cleaning Hard Surfaces That Do Not Soak Up Water The procedure to prevent mold growth on hard surfaces that do not soak up water is as follows:
Additional Safety Guidelines for Mold Clean-up Persons cleaning moldy or potentially moldy surfaces should:
Health-Outcome Surveillance and Follow Up State and local public health agencies do not generally collect information on the conditions related to mold exposure. In situations where there are large numbers of flooded and mold-contaminated buildings, such as occurred in New Orleans after hurricanes Katrina and Rita in fall of 2005 (2), the repopulation of those once-flooded areas probably will expose a large number of persons to potentially hazardous levels of mold and other microbial agents. Efforts to determine the health effects of these exposures and the effectiveness of recommendations to prevent these adverse health effects require a surveillance strategy. Developing such a strategy requires that federal and local health agencies work together to monitor trends in the incidence or prevalence of mold-related conditions throughout the recovery period. Monitoring trends in health outcomes that might be related to mold exposure will require substantial human and financial resources and will face several challenges. Health outcomes that might be attributed to mold exposure fall into several broad categories. Some potential health outcomes are rare, difficult to diagnose, and relatively specific for fungal exposure (e.g., blastomycosis). Other health outcomes are relatively easy to diagnose, but they have numerous etiologic factors and are difficult to attribute specifically to mold exposure (e.g., asthma exacerbations). Tracking different health outcomes that might be caused by mold exposure requires different surveillance methods. In some cases, follow-up research will be needed to verify that surveillance findings and health outcomes are the result of mold exposure. For some conditions, difficulties in interpreting trends and in relating the outcome to mold exposure might suggest that surveillance is not an appropriate public health approach. Results of surveillance and follow-up activities will help CDC refine the guidelines for exposure avoidance, personal protection, and clean-up. In addition, these activities should assist health departments to identify unrecognized hazards. Surveillance Public health agencies should consider collecting health outcome information from health-care facilities to monitor the incidence or prevalence of selected conditions. State or local agencies should determine the feasibility of this approach and consider the required resources available or attainable to accomplish this goal. Institutions from which data could be collected include hospitals, emergency departments, clinics and, for some outcomes, specific subspecialty providers. Surveillance will require the establishment of case definitions and reporting sources; development of reporting mechanisms; training of data providers; and the collection, analysis, and reporting of data. The surveillance data should be used to identify increases in disease that are substantial enough to trigger public health interventions or follow-up investigations to learn the reason for the increase and establish targeted prevention strategies. Public health agencies should consider the need for clinicians to report cases of known or suspected mold-associated illnesses (e.g., invasive fungal disease, blastomycosis, hypersensitivity pneumonitis attributed to mold contamination, ODTS attributed to contaminated dust exposure, and alveolar hemorrhage in infants) to public health authorities for tracking and follow-up investigations. Providers caring for patients at high risk for poor health outcomes related to mold exposure could be targeted. For example, hematologists, rheumatologists, and pulmonologists might care for many patients at risk for invasive mold infections because of underlying malignancies and immunosuppression. Enhancing provider-based surveillance requires targeting and educating providers; developing reporting mechanisms; and collecting, analyzing, and reporting data. Public health agencies should consider the need for establishing laboratory-based surveillance as an efficient method for monitoring mold-related illnesses that involve laboratory analyses (e.g., invasive fungal disease, blastomycosis, invasive aspergillosis, histoplasmosis, Aspergillus preceptins, zygomycosis, and fusariosis). Clinical Care Health-care providers should be alert for unusual mold-related diseases that might occur (e.g., hypersensitivity pneumonitis, ODTS, and blastomycosis). Otherwise, such diseases might not be recognized. Scientific evidence is insufficient to support the routine clinical use of immunodiagnostic tests as a primary means of assessing environmental fungal exposure or health effects related to fungal exposure. Health-care providers who care for persons who are concerned about the relation between their symptoms and exposure to fungi are advised to use immunodiagnostic test results with care and only in combination with other clinical information, including history, physical examination, and other laboratory data. If appropriate allergy prick skin testing reagents or in vitro tests for serum specific IgE are available, they can be used to show specific IgE-sensitization to causative allergens. Unfortunately, skin testing reagents and blood tests documenting IgE-sensitization to molds are, with few exceptions, poorly standardized and of unclear sensitivity and specificity. The conventional hierarchy of treatment for allergic diseases includes avoidance of exposure to inciting agents, pharmacotherapy and, as a last resort, allergen immunotherapy. Immunotherapy with fungal allergenic extracts is, with a few exceptions, of unknown efficacy. Clinicians should report cases of mold-induced illness to local health authorities to assist in surveillance efforts. Acknowledgments Athena Gemella, MS, coordinated the external review of the document; Marissa Scalia, MPH, and Allison Stock, PhD, provided background and resource materials for the document, National Center for Environmental Health. Kay Kreiss, MD, provided input and feedback during the development of the document, National Institute for Occupational Safety and Health. References
Table 1 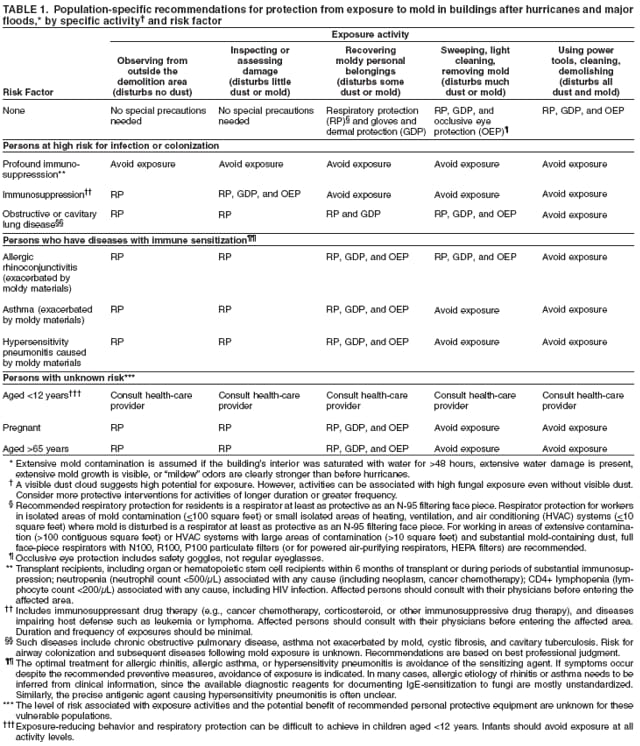 Return to top. Table 2 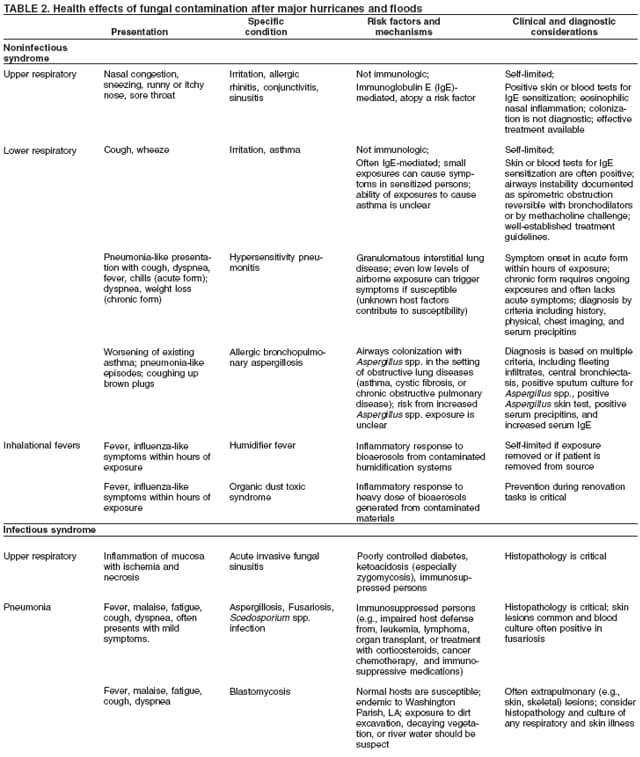 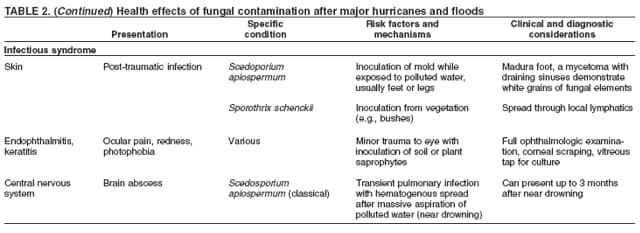 Return to top. Table 3  Return to top. Table 4 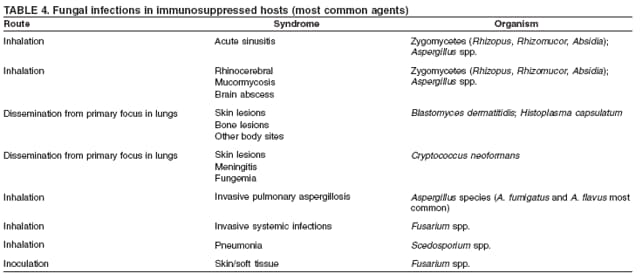 Return to top. Table 5 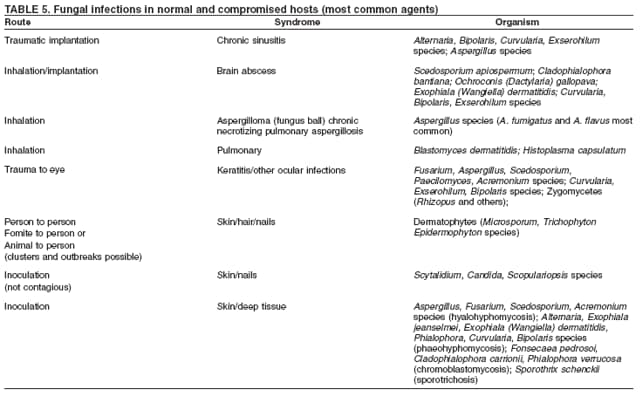 Return to top.
All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 5/25/2006 |
|||||||||
|