 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Managing Acute Gastroenteritis Among ChildrenOral Rehydration, Maintenance, and Nutritional Therapy Prepared by The material for this report originated in the National Center for Infectious Diseases, James M. Hughes, M.D., Director, and the Division of Viral and Rickettsial Diseases, James LeDuc, Ph.D., Director. Summary Acute gastroenteritis remains a common illness among infants and children throughout the world. Among children in the United States, acute diarrhea accounts for >1.5 million outpatient visits, 200,000 hospitalizations, and approximately 300 deaths/year. In developing countries, diarrhea is a common cause of mortality among children aged <5 years, with an estimated 2 million deaths annually. Oral rehydration therapy (ORT) includes rehydration and maintenance fluids with oral rehydration solutions (ORS), combined with continued age-appropriate nutrition. Although ORT has been instrumental in improving health outcomes among children in developing countries, its use has lagged behind in the United States. This report provides a review of the historical background and physiologic basis for using ORT and provides recommendations for assessing and managing children with acute diarrhea, including those who have become dehydrated. Recent developments in the science of gastroenteritis management have substantially altered case management. Physicians now recognize that zinc supplementation can reduce the incidence and severity of diarrheal disease, and an ORS of reduced osmolarity (i.e., proportionally reduced concentrations of sodium and glucose) has been developed for global use. The combination of oral rehydration and early nutritional support has proven effective throughout the world in treating acute diarrhea. In 1992, CDC prepared the first national guidelines for managing childhood diarrhea (CDC. The management of acute diarrhea in children: oral rehydration, maintenance, and nutritional therapy. MMWR 1992;41[No. RR-16]), and this report updates those recommendations. This report reviews the historical background and scientific basis of ORT and provides a framework for assessing and treating infants and children who have acute diarrhea. The discussion focuses on common clinical scenarios and traditional practices, especially regarding continued feeding. Limitations of ORT, ongoing research in the areas of micronutrient supplements, and functional foods are reviewed as well. These updated recommendations were developed by specialists in managing gastroenteritis, in consultation with CDC and external consultants. Relevant literature was identified through an extensive MEDLINE search by using related terms. Articles were then reviewed for their relevance to pediatric practice, with emphasis on U.S. populations. Unpublished references were sought from the external consultants and other researchers. In the United States, adoption of these updated recommendations could substantially reduce medical costs and childhood hospitalizations and deaths caused by diarrhea. IntroductionAmong children in the United States, acute gastroenteritis remains a major cause of morbidity and hospitalization, accounting for >1.5 million outpatient visits, 200,000 hospitalizations, and approximately 300 deaths/year. Direct medical costs for rotavirus diarrhea, which represents approximately one third of all hospitalizations for diarrhea among U.S. children aged <5 years, have been estimated to be $250 million/year, with an estimated $1 billion/year in total costs to society (1). Worldwide, diarrheal diseases are a leading cause of pediatric morbidity and mortality, with 1.5 billion episodes and 1.5--2.5 million deaths estimated to occur annually among children aged <5 years (2--4). Although the total number of deaths from diarrhea is still unacceptably high, these numbers have been reduced substantially in the 1980s and 1990s. For example, in 1982, an estimated 5 million deaths/year occurred (5), and in 1992, the estimated annual deaths declined to 3 million/year (6). A substantial portion of the decrease in mortality is attributable to worldwide campaigns to treat acute diarrhea with oral rehydration therapy (ORT). The development of ORT represents a successful collaboration between basic and applied biomedical research (7). The application of ORT also represents a case of reverse technology transfer (8), because protocols originally implemented to benefit patients in developing countries have changed the standard of care in industrialized countries as well. ORT encompasses two phases of treatment: 1) a rehydration phase, in which water and electrolytes are administered as oral rehydration solution (ORS) to replace existing losses, and 2) a maintenance phase, which includes both replacement of ongoing fluid and electrolyte losses and adequate dietary intake. Although ORT implies rehydration alone, the definition used in this report has been broadened to include maintenance fluid therapy and appropriate nutrition. The full benefits of ORT for acute gastroenteritis have not been realized, especially in countries with developed market economies that have lagged behind less-developed countries in their use of ORT. One reason for this low usage of ORT might be the ingrained use of intravenous (IV) therapy or the reduced appeal of a technologically simple solution (9,10). This is especially true in the United States, where children with all forms of dehydration are treated with IV fluids rather than ORT (11--16). Approximately 30% of practicing pediatricians withhold ORT for children with vomiting or moderate dehydration (17). In addition, the practice of continued feeding during diarrheal episodes has been difficult to establish as accepted standard of care. Although substantial in vitro and in vivo data support the role of continued nutrition in improving gastrointestinal function and anthropometric, biochemical, and clinical outcomes (18,19), early appropriate feeding is often withheld. In 1992, CDC prepared the first national guidelines for managing childhood diarrhea (20). Since the last recommendations were published in MMWR, data have emerged regarding diarrhea treatment, including the importance of zinc supplementation and the value of more effective oral solutions of lower osmolarity (i.e., proportionally reduced concentrations of sodium and glucose). These recommendations update the previous report, review the historical background and scientific basis of ORT, and provide a framework for assessing and treating infants and children who have acute diarrhea. The discussion focuses on common clinical scenarios and traditional practices, especially with regard to continued feeding. Limitations of ORT, ongoing research in the areas of micronutrient supplements, and functional foods are reviewed. These updated recommendations were developed by specialists in managing gastroenteritis, in consultation with CDC and external consultants. Relevant literature was identified through an extensive MEDLINE search by using related terms. Articles were then reviewed for their relevance to pediatric practice, with emphasis on U.S. populations. Unpublished references were sought from the external consultants and other researchers. BackgroundEarly attempts at treating dehydration resulting from diarrhea were described in the 1830s during epidemics of Vibrio cholerae infections (21,22). Use of IV fluid did not become widespread until >100 years later. In the 1940s, oral solutions were developed (23), and the effect of potassium replacement in reducing mortality was recognized, which led to substantial decreases in case fatality rates. By the 1950s, patients with cholera were being successfully treated with IV fluids (24). Studies documenting the effectiveness of IV rehydration fluids among economically disadvantaged populations provided an impetus to develop less expensive but equally effective oral solutions. Studies published in 1968 from Dhaka and Calcutta demonstrated the effectiveness of ORS for cholera patients, including those with high stool output (25,26). In 1971, oral electrolyte solutions were tested through the large-scale treatment of refugees from Bangladesh (12,27). The resulting success of oral solutions hastened development of the first World Health Organization (WHO) guidelines for ORT and the production of standard packets of oral rehydration salts. Now, ORT is accepted as the standard of care for the clinically efficacious and cost-effective management of acute gastroenteritis (9,20). Physiologic Basis for Using Oral Rehydration SolutionsHuman survival depends on the secretion and reabsorption of fluid and electrolytes in the intestinal tract. The adult intestinal epithelium must handle 6,500 mL of fluids/day, consisting of a combination of oral intake, salivary, gastric, pancreatic, biliary, and upper intestinal secretions. This volume is typically reduced to 1,500 mL by the distal ileum and is further reduced in the colon to a stool output of <250 mL/day in adults (28). During diarrheal disease, the volume of intestinal fluid output is substantially increased, overwhelming the reabsorptive capacity of the gastrointestinal tract. Applied clinical research, first implemented among patients with cholera (25,29), demonstrated that although the secretory nature of diarrhea in cholera results in substantial stool losses of water and electrolytes, intact Na-coupled solute co-transport mechanism allows efficient reabsorption of salt and water (30). In addition to V. cholerae 01 and 139, certain strains of Escherichia coli, shigella, salmonella, and other pathogenic bacteria produce toxins that bind to enterocyte receptors, causing chloride-mediated secretion stimulated by second messengers (e.g., cAMP, cGMP, and calcium) (31,32). Even those infectious agents typically classified as causing osmotic diarrhea (i.e., fluid and electrolyte loss caused by malabsorbed intestinal contents) can increase enterocyte secretion. Rotavirus damages the villous brush border, causing osmotic diarrhea, and also produces an enterotoxin that causes a Ca++-mediated secretory diarrhea (33). Studies of intestinal solute transport mechanisms were also crucial in outlining the processes by which solute absorption is maintained. Water passively follows the osmotic gradient generated by the transcellular transport of electrolytes and nutrients. Although three principle mechanisms of sodium absorption have been described (28), the mechanism essential to the efficacy of ORS is the coupled transport of sodium and glucose molecules at the intestinal brush border (34) (Figure). Co-transport across the luminal membrane is facilitated by the protein sodium glucose co-transporter 1 (SGLT1). Once in the enterocyte, the transport of glucose into the blood is facilitated by GLUT2 (glucose transporter type 2) in the basolateral membrane. The Na+ K+ ATPase provides the gradient that drives the process. This mechanism remains intact, even in patients with severe diarrhea (25). ORS in which additional co-transporters of Na (e.g., amino acids or cereals) were added has demonstrated promising results, but larger trials have not confirmed their efficacy (35,36). Solutions with a high concentration of co-transporters increase the risk from hypertonic solutions that decrease rather than improve sodium and water transport into the bloodstream. However, solutions of lower osmolarity, but that maintain the 1:1 glucose to sodium ratio, perform optimally as oral solutions for diarrhea management (see Choice of ORS). Home Management of Acute DiarrheaTreatment with ORS is simple and enables management of uncomplicated cases of diarrhea at home, regardless of etiologic agent. As long as caregivers are instructed properly regarding signs of dehydration or are able to determine when children appear markedly ill or appear not to be responding to treatment, therapy should begin at home. Early intervention can reduce such complications as dehydration and malnutrition. Early administration of ORS leads to fewer office, clinic, and emergency department (ED) visits (37) and to potentially fewer hospitalizations and deaths. Initiation of TherapyIn all cultures, treatment of diarrhea usually begins at home (38). All families should be encouraged to have a supply of ORS in the home at all times and to start therapy with a commercially available ORS product as soon as diarrhea begins. Although producing a homemade solution with appropriate concentrations of glucose and sodium is possible, serious errors can occur (39); thus, standard commercial oral rehydration preparations should be recommended where they are readily available and attainable. The most crucial aspect underlying home management of diarrhea is the need to replace fluid losses and to maintain adequate nutrient intake. Regardless of the fluid used, an age-appropriate diet should also be given (18,19). Infants should be offered more frequent breast or bottle feedings, and older children should be given more fluids. Severity AssessmentCaregivers should be trained to recognize signs of illness or treatment failure that necessitate medical intervention. Infants with acute diarrhea are more prone to becoming dehydrated than are older children, because they have a higher body surface-to-volume ratio, a higher metabolic rate, relatively smaller fluid reserves, and they are dependent on others for fluid. For this reason, parents of infants with diarrhea should promptly seek medical evaluation as soon as the child appears to be in distress (Box 1). No guidelines have established a specific age under which evaluation is mandated, but usually, the smaller the child, the lower the threshold for health-care provider assessment. When fever is present, infants and children should be evaluated to rule out other serious illnesses (e.g., sepsis and meningitis). Underlying conditions, including premature birth, metabolic and renal disorders, immune compromise, or recent recovery from surgery, might prompt early evaluation, as might concurrent illness, including a concurrent respiratory tract infection. Children with dysentery (blood or mucus in stool) or prolonged diarrhea (lasting >14 days) should be evaluated because stool cultures and antimicrobial therapy might be indicated. Reports from parents or other caregivers of dehydration can indicate the need for immediate health-care provider evaluation. Reports of changing mental status are of particular concern. When the child's condition is in doubt, immediate evaluation by a health-care professional should be recommended. Clinical examination of the child provides an opportunity for physical assessment, including vital signs, degree of dehydration, and a more detailed history, and for providing better instructions to the caregivers. Referral for EvaluationIn developed countries, the decision whether to bring a child to an office or ED setting for evaluation is usually made after consultation with a physician or other health-care provider by telephone. Questions should focus on those factors putting a child at risk for dehydration. Whenever possible, quantification is helpful. The clinician should determine how many hours or days the child has been ill, the number of episodes of diarrhea or vomiting, and the apparent volume of fluid output. The child's mental status should be determined. Parents and other caregivers might not mention underlying conditions without prompting; therefore, questions from the health-care provider regarding past medical history are essential. Clinical AssessmentDiarrhea is characterized by the passage of loose or watery stools; a common case definition of acute diarrhea is >3 loose or watery stools/day. The volume of fluid lost through stools can vary from 5 mL/kg body weight/day (approximately normal) to >200 mL/kg body weight/day (40). Dehydration and electrolyte losses associated with untreated diarrhea cause the primary morbidity of acute gastroenteritis. Diarrhea can be among the initial signs of nongastrointestinal tract illnesses, including meningitis, bacterial sepsis, pneumonia, otitis media, and urinary tract infection. Vomiting alone can be the first symptom of metabolic disorders, congestive heart failure, toxic agent ingestion, or trauma. To rule out other serious illnesses, a detailed history and physical examination should be performed as part of the evaluation of all children with acute gastroenteritis. HistoryThe clinical history should assess the onset, frequency, quantity, and character (i.e., the presence of bile, blood, or mucus) of vomiting and diarrhea. Recent oral intake, including breast milk and other fluids and food; urine output; weight before illness; and associated symptoms, including fever or changes in mental status, should be noted. The past medical history should identify underlying medical problems, history of other recent infections, medications, and human immunodeficiency virus (HIV) status. A relevant social history can include the number and nature of caregivers, which can affect instructions regarding follow-up care. Physical ExaminationAs part of the physical examination, an accurate body weight must be obtained, along with temperature, heart rate, respiratory rate, and blood pressure. When recent premorbid weight is unknown but a previous growth curve is available, an estimate of fluid loss can be obtained by subtracting current weight from expected weight as determined on the basis of the previous weight-for-age percentile. The quality of this estimate will vary, depending on the number and variability of prior data points, differences among scales, and other factors. The general condition of the patient should be assessed, with special concern given to infants and children who appear listless, apathetic, or less reactive. The appearance of the eyes should be noted, including the degree to which they are sunken and the presence or absence of tears. The condition of the lips, mouth, and tongue will yield critical clues regarding the degree of dehydration, even if the patient has taken fluid recently. Deep respirations can be indicative of metabolic acidosis. Faint or absent bowel sounds can indicate hypokalemia. Examination of the extremities should be included because general perfusion and capillary refill can help in assessment of dehydration. An especially valid sign is the presence of prolonged skin tenting (41). Visual examination of stool can confirm abnormal consistency and determine the presence of blood or mucus. Dehydration AssessmentCertain clinical signs and symptoms can quantify the extent of a patient's dehydration (Table 1). Assessment of the anterior fontanel might be helpful in selected instances, but it can be unreliable or misleading (41,42). Among infants and children, a decrease in blood pressure is a late sign of dehydration that heralds shock and can correspond to fluid deficits >10%. Increases in heart rate and reduced peripheral perfusion can be more sensitive indicators of moderate dehydration, although both can be difficult to interpret because they can vary with the degree of fever. Decreased urine output is a sensitive but nonspecific sign. Urine output might be difficult to measure for infants with diarrhea; however, if urinalysis is indicated, a finding of increased urine specific gravity can indicate dehydration. Prior guidelines, including CDC's 1992 recommendations (20) and the American Academy of Pediatrics (AAP) 1996 guidelines (9), divide patients into subgroups for mild (3%--5% fluid deficit), moderate (6%--9% fluid deficit), or severe (>10% fluid deficit, shock, or near shock) dehydration. Other classification schemes, including the 1995 WHO (40) and 2001 European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) guidelines (43), divide patients into those indicating no signs of dehydration (<3%--5%), some signs of dehydration (5%--10%), and severe dehydration (>10%). Studies that have evaluated the correlation of clinical signs of dehydration with posttreatment weight gain indicate that the first signs of dehydration might not be evident until 3%--4% dehydration, with more numerous clinical signs evident at 5% dehydration and signs indicating severe dehydration not evident until fluid loss reaches 9%--10% (40,41). Because of this threshold effect, distinguishing between mild and moderate dehydration on the basis of clinical signs alone might be difficult. Therefore, these updated recommendations group together patients with mild to moderate dehydration and specify that the signs of dehydration might be apparent over a relatively wide range of fluid loss (i.e., from 3%--9%) (Table 1). The goal of assessment is to provide a starting point for treatment and to conservatively determine which patients can safely be sent home for therapy, which ones should remain for observation during therapy, and which ones should immediately receive more intensive therapy. Utility of Laboratory EvaluationSupplementary laboratory studies, including serum electrolytes, to assess patients with acute diarrhea usually are unnecessary (44,45). Stool cultures are indicated in cases of dysentery but are not usually indicated in acute, watery diarrhea for the immunocompetent patient. However, certain laboratory studies might be important when the underlying diagnosis is unclear or diagnoses other than acute gastroenteritis are possible. For example, complete blood counts and urine and blood cultures might be indicated when sepsis or urinary tract infection is a concern. Acute Gastroenteritis Therapy Based on Degree of DehydrationSeven basic principles guide optimal treatment of acute gastroenteritis (Box 2) (43); more specific recommendations for treating different degrees of dehydration have been recommended by CDC, WHO, and AAP (Table 2) (9,20,40). Although the first principle, use of ORS, seems self-evident, one national survey of physicians in emergency care facilities indicated that many would treat mild dehydration with IV therapy, and half would always or routinely use IV therapy for a moderately dehydrated child aged <2 years (14). Treatment should include two phases: rehydration and maintenance. In the rehydration phase, the fluid deficit is replaced quickly (i.e., during 3--4 hours) and clinical hydration is attained. In the maintenance phase, maintenance calories and fluids are administered. Rapid realimentation should follow rapid rehydration, with a goal of quickly returning the patient to an age-appropriate unrestricted diet, including solids. Gut rest is not indicated. Breastfeeding should be continued at all times, even during the initial rehydration phases. The diet should be increased as soon as tolerated to compensate for lost caloric intake during the acute illness. Lactose restriction is usually not necessary (although it might be helpful in cases of diarrhea among malnourished children or among children with a severe enteropathy), and changes in formula usually are unnecessary. Full-strength formula usually is tolerated and allows for a more rapid return to full energy intake. During both phases, fluid losses from vomiting and diarrhea are replaced in an ongoing manner. Antidiarrheal medications are not recommended for infants and children, and laboratory studies should be limited to those needed to guide clinical management. Minimal DehydrationFor patients with minimal or no dehydration, treatment is aimed at providing adequate fluids and continuing an age-appropriate diet. Patients with diarrhea must have increased fluid intake to compensate for losses and cover maintenance needs; use of ORS should be encouraged. In principle, 1 mL of fluid should be administered for each gram of output. In hospital settings, soiled diapers can be weighed (without urine), and the estimated dry weight of the diaper can be subtracted. When losses are not easily measured, 10 mL of additional fluid can be administered per kilogram body weight for each watery stool or 2 mL/kg body weight for each episode of emesis. As an alternative, children weighing <10 kg should be administered 60--120 mL (2--4 ounces) ORS for each episode of vomiting or diarrheal stool, and those weighing >10 kg should be administered 120--240 mL (4--8 ounces). Nutrition should not be restricted (see Dietary Therapy). Mild to Moderate DehydrationChildren with mild to moderate dehydration should have their estimated fluid deficit rapidly replaced. These updated recommendations include administering 50--100 mL of ORS/kg body weight during 2--4 hours to replace the estimated fluid deficit, with additional ORS administered to replace ongoing losses. Using a teaspoon, syringe, or medicine dropper, limited volumes of fluid (e.g., 5 mL or 1 teaspoon) should be offered at first, with the amount gradually increased as tolerated. If a child appears to want more than the estimated amount of ORS, more can be offered. Although administering ORS rapidly is safe, vomiting might be increased with larger amounts. Nasogastric (NG) feeding allows continuous administration of ORS at a slow, steady rate for patients with persistent vomiting or oral ulcers. Clinical trials support using NG feedings, even for vomiting patients (45). Rehydration through an NG tube can be particularly useful in ED settings, where rapid correction of hydration might prevent hospitalization. Although rapid IV hydration can also prevent hospital admission, rapid NG rehydration can be well-tolerated, more cost-effective, and associated with fewer complications (45). In addition, a randomized trial of ORS versus IV rehydration for dehydrated children demonstrated shorter stays in EDs and improved parental satisfaction with oral rehydration (46). Certain children with mild to moderate dehydration will not improve with ORT; therefore, they should be observed until signs of dehydration subside. Similarly, children who do not demonstrate clinical signs of dehydration but who demonstrate unusually high output should be held for observation. Hydration status should be reassessed on a regular basis, and might be performed in an ED, office, or other outpatient setting. After dehydration is corrected, further management can be implemented at home, provided that the child's caregivers demonstrate comprehension of home rehydration techniques (including continued feeding), understand indications for returning for further evaluation, and have the means to do so. Even among children whose illness appears uncomplicated on initial assessment, a limited percentage might not respond adequately to ORT; therefore, a plan for reassessment should be agreed upon. Caregivers should be encouraged to return for medical attention if they have any concerns, if they are not sure that rehydration is proceeding well, or if new or worsening symptoms develop. Severe DehydrationSevere dehydration constitutes a medical emergency requiring immediate IV rehydration. Lactated Ringer's (LR) solution, normal saline, or a similar solution should be administered (20 mL/kg body weight) until pulse, perfusion, and mental status return to normal. This might require two IV lines or even alternative access sites (e.g., intraosseous infusion). The patient should be observed closely during this period, and vital signs should be monitored on a regular basis. Serum electrolytes, bicarbonate, blood urea nitrogen, creatinine, and serum glucose levels should be obtained, although commencing rehydration therapy without these results is safe. Normal saline or LR infusion is the appropriate first step in the treatment of hyponatremic and hypernatremic dehydration. Hypotonic solutions should not be used for acute parenteral rehydration (47). Severely dehydrated patients might require multiple administrations of fluid in short succession. Overly rapid rehydration is unlikely to occur as long as weight-based amounts are administered with close observation. Errors occur most commonly in settings where adult dosing is administered to infants (e.g., "500 mL NS [normal saline] IV bolus x 2" would provide 200 mL/kg body weight for an average infant aged 2--3 months). Edema of the eyelids and extremities can indicate overhydration. Diuretics should not be administered. After the edema has subsided, the patient should be reassessed for continued therapy. With frail or malnourished infants, smaller amounts (10 mL/kg body weight) are recommended because of the reduced ability of these infants to increase cardiac output and because distinguishing dehydration from sepsis might be difficult among these patients. Smaller amounts also will facilitate closer evaluation. Hydration status should be reassessed frequently to determine the adequacy of replacement therapy. A lack of response to fluid administration should raise the suspicion of alternative or concurrent diagnoses, including septic shock and metabolic, cardiac, or neurologic disorders. As soon as the severely dehydrated patient's level of consciousness returns to normal, therapy usually can be changed to the oral route, with the patient taking by mouth the remaining estimated deficit. An NG tube can be helpful for patients with normal mental status but who are too weak to drink adequately. Although no studies have specifically documented increased aspiration risk with NG tube use in obtunded patients, IV therapy is typically favored for such patients. Although leaving IV access in place for these patients is reasonable in case it is needed again, early reintroduction of ORS is safer. Using IV catheters is associated with frequent minor complications, including extravasation of IV fluid, and with rare substantial complications, including the inadvertent administration of inappropriate fluid (e.g., solutions containing excessive potassium). In addition, early ORS will probably encourage earlier resumption of feeding, and data indicate that resolution of acidosis might be more rapid with ORS than with IV fluid (45). Clinical Management in the HospitalInpatient care is indicated for children if
In addition, studies of mortality caused by acute diarrhea in the United States have identified prematurity, young maternal age, black race, and rural residence as risk factors for suboptimal outcome (48); thus, these factors should also be considered when deciding if hospital care is required. Limitations of ORTAlthough ORT is recommended for all age groups and for diarrhea of any etiology, certain restrictions apply to its use. Among children in hemodynamic shock, administration of oral solutions might be contraindicated because airway protective reflexes might be impaired. Likewise, patients with abdominal ileus should not be administered oral fluids until bowel sounds are audible. Intestinal intussusception can be present with diarrhea, including bloody diarrhea. Radiographic and surgical evaluation are warranted when the diagnosis of bowel obstruction is in question. Stool output in excess of 10 mL/kg body weight/hour has been associated with a lower rate of success of oral rehydration (49); however, children should not be denied ORT simply because of a high purging rate, because the majority of children will respond well if administered adequate replacement fluid. A limited percentage of infants (<1%) with acute diarrhea experience carbohydrate malabsorption. This is characterized by a dramatic increase in stool output after intake of fluids containing simple sugars (e.g., glucose), including ORS. Patients with true glucose malabsorption also will have an immediate reduction in stool output when IV therapy is used instead of ORS. However, the presence of stool-reducing substances alone is not sufficient to make this diagnosis, because this is a common finding among patients with diarrhea and does not in itself predict failure of oral therapy. Certain patients with acute diarrhea have concomitant vomiting. However, the majority can be rehydrated successfully with oral fluids if limited volumes of ORS (5 mL) are administered every 5 minutes, with a gradual increase in the amount consumed. Administration with a spoon or syringe under close supervision helps guarantee a gradual progression in the amount taken. Often, correction of acidosis and dehydration lessens the frequency of vomiting. Continuous slow NG infusion of ORS through a feeding tube might be helpful. Even if a limited amount of emesis occurs after NG administration of fluid, treatment might not be affected adversely (45). The physician might meet resistance in implementing NG rehydration in a vomiting child, but NG rehydration might help the initial rehydration and speed up tolerance to refeeding (50), leading to improved patient disposition and quicker discharge. Hypernatremic DehydrationPatients with hypernatremic dehydration (i.e., serum sodium concentration >145 mEq/L) respond well to ORT. Those with severe dehydration should first receive IV hydration as previously discussed. Subsequent hydration should be achieved with ORS (51). As with isonatremic dehydration, ORS should be administered to replace the calculated deficit and ongoing losses. ORS might be safer than IV therapy because it is less likely to lead to a precipitous increase in intracellular water associated with seizures and elevated intracranial pressure (43). For more detailed recommendations regarding therapy of hypernatremic dehydration, other sources should be consulted (52). Dietary TherapyRecommendations for maintenance dietary therapy depend on the age and diet history of the patient. Breastfed infants should continue nursing on demand. Formula-fed infants should continue their usual formula immediately upon rehydration in amounts sufficient to satisfy energy and nutrient requirements. Lactose-free or lactose-reduced formulas usually are unnecessary. A meta-analysis of clinical trials indicates no advantage of lactose-free formulas over lactose-containing formulas for the majority of infants, although certain infants with malnutrition or severe dehydration recover more quickly when given lactose-free formula (53). Patients with true lactose intolerance will have exacerbation of diarrhea when a lactose-containing formula is introduced. The presence of low pH (<6.0) or reducing substances (>0.5%) in the stool is not diagnostic of lactose intolerance in the absence of clinical symptoms. Although medical practice has often favored beginning feedings with diluted (e.g., half- or quarter-strength) formula, controlled clinical trials have demonstrated that this practice is unnecessary and is associated with prolonged symptoms (54) and delayed nutritional recovery (55). Formulas containing soy fiber have been marketed to physicians and consumers in the United States, and added soy fiber has been reported to reduce liquid stools without changing overall stool output (56). This cosmetic effect might have certain benefits with regard to diminishing diaper rash and encouraging early resumption of normal diet but is probably not sufficient to merit its use as a standard of care. A reduction in the duration of antibiotic-associated diarrhea has been demonstrated among older infants and toddlers fed formula with added soy fiber (57). Children receiving semisolid or solid foods should continue to receive their usual diet during episodes of diarrhea. Foods high in simple sugars should be avoided because the osmotic load might worsen diarrhea; therefore, substantial amounts of carbonated soft drinks, juice, gelatin desserts, and other highly sugared liquids should be avoided. Certain guidelines have recommended avoiding fatty foods, but maintaining adequate calories without fat is difficult, and fat might have a beneficial effect of reducing intestinal motility. The practice of withholding food for >24 hours is inappropriate. Early feeding decreases changes in intestinal permeability caused by infection (58), reduces illness duration, and improves nutritional outcomes (18,19). Highly specific diets (e.g., the BRAT [bananas, rice, applesauce, and toast] diet) have been commonly recommended. Although certain benefits might exist from green bananas and pectin in persistent diarrhea (59), the BRAT diet is unnecessarily restrictive and, similar to juice-centered diets, can provide suboptimal nutrition for the patient's nourishment and recovering gut. Severe malnutrition can occur after gastroenteritis if prolonged gut rest or clear fluids are prescribed (60). Children in underdeveloped countries often have multiple episodes of diarrhea in a single season, making diarrhea a contributing factor to suboptimal nutrition, which can increase the frequency and severity of subsequent episodes (61). For this reason, increased nutrient intake should be administered after an episode of diarrhea. Recommended foods include age-appropriate unrestricted diets, including complex carbohydrates, meats, yogurt, fruits, and vegetables. Children should as best as possible maintain caloric intake during acute episodes, and subsequently should receive additional nutrition to compensate for any shortfalls arising during the illness. Pharmacologic TherapyAntimicrobial AgentsBecause viruses (e.g., rotavirus, astrovirus, enteric adenovirus, norovirus, and sapovirus) are the predominant cause of acute diarrhea in developed countries (62), the routine use of antimicrobial agents for treating diarrhea wastes resources and might lead to increased antimicrobial resistance. Even when a bacterial cause is suspected in an outpatient setting, antimicrobial therapy is not usually indicated among children because the majority of cases of acute diarrhea are self-limited and not shortened by antimicrobial agents. Exceptions to these rules involve special needs of individual children (e.g., immune-compromised hosts, premature infants, or children with underlying disorders). Information regarding appropriate antimicrobial therapy of bacterial and parasitic causes of acute infectious diarrhea is available (63--66). Nonantimicrobial Drug TherapiesNonspecific antidiarrheal agents (e.g., adsorbents such as kaolin-pectin), antimotility agents (e.g., loperamide), antisecretory drugs, and toxin binders (e.g., cholestyramine), are commonly used among older children and adults, but data are limited regarding their efficacy. Side effects of these drugs are well-known, in particular among the antimotility agents, including opiate-induced ileus, drowsiness, and nausea caused by the atropine effects and binding of nutrients and other drugs. In Pakistan, 18 cases of severe abdominal distention associated with using loperamide included 6 deaths (67). Bismuth subsalicylate has limited efficacy in treating traveler's diarrhea (68) and other causes of acute gastroenteritis among children (69). Although the side effects are fewer than those from antimotility agents, certain theoretical concerns regarding the potential toxicity from salicylate absorption remain (70), and trials supporting its use have employed frequent doses (e.g., every 4 hours for 5 days) (71). None of these drugs address the underlying causes of diarrhea, specifically increased secretion by intestinal crypt cells. Racecadotril, an enkephalinase inhibitor, preserves the antisecretory activity of enkephalins and does not slow intestinal transit or promote bacterial overgrowth (72). Its use has demonstrated promise in two controlled clinical trials among children, among whom it significantly reduced stool output when compared with placebo (73,74). Although the majority of cases of acute diarrhea require no adjunctive therapy, racecadotril might prove to be a useful adjunct. More studies are needed. Antiemetics are usually unnecessary in acute diarrhea management. Using phenothiazines might interfere with oral rehydration by causing sleepiness. Ondansetron, a serotonin antagonist, either by the oral (75) or IV (76) route, can be effective in decreasing vomiting and limiting hospital admission. However, reliance on pharmacologic agents shifts the therapeutic focus away from appropriate fluid, electrolyte, and nutritional therapy, can result in adverse events, and can add unnecessarily to the economic cost of illness. Because acute diarrhea is a common illness, cost-effective analyses should be undertaken before routine pharmacologic therapy is recommended. Supplemental Zinc TherapyMultiple reports have linked diarrhea and abnormal zinc status (77), including increased stool zinc loss, negative zinc balance (78), and reduced tissue levels of zinc (79). Although severe zinc deficiency (e.g., acrodermatitis enteropathica) is associated with diarrhea, milder deficiencies of zinc might play a role in childhood diarrhea, and zinc supplementation might be of benefit either for improved outcomes in acute or chronic diarrhea or as prophylaxis against diarrheal disease. Reduced duration of acute diarrhea after zinc supplementation among patients with low zinc concentrations in rectal biopsies has been demonstrated (79). In Bangladesh, zinc supplements also improved markers of intestinal permeability among children with diarrhea (80). In India, zinc supplementation was associated with a decrease in both the mean number of watery stools per day and the number of days with watery diarrhea (81). Prophylactic zinc supplementation in India has been associated with a substantially reduced incidence of severe and prolonged diarrhea, two key determinants of malnutrition and diarrhea-related mortality (82). In Nepal, this effect was independent of concomitant vitamin A administration, with limited side effects apart from a slight increase in emesis (83). In Peru, zinc administration was associated with a reduction in duration of persistent diarrhea (84). In two different pooled analyses of randomized controlled trials in developing countries (85,86), zinc supplementation was beneficial for treating children with acute and persistent diarrhea and as a prophylactic supplement for decreasing the incidence of diarrheal disease and pneumonia. Among infants and young children who received supplemental zinc for 5 or 7 days/week for 12--54 weeks, the pooled odds ratio (OR) for diarrhea incidence was 0.82 (95% confidence interval [CIs] = 0.72--0.93), and the OR for pneumonia incidence was 0.59 (95% CI = 0.41--0.83). The efficacy and safety of a zinc-fortified (40 mg/L) ORS among 1,219 children with acute diarrhea was evaluated (87). Compared with zinc syrup administered at a dose of 15--30 mg/day, zinc-fortified ORS did not increase the plasma zinc concentration. However, clinical outcomes among the zinc-fortified ORS group were modestly improved, compared with those for the control group, who received standard ORS only. In that study, the total number of stools was lower among the zinc-ORS group (relative risk: 0.83; 95% CI = 0.71--0.96), compared with the total number for the control group. No substantial effect on duration of diarrhea or risk for prolonged diarrhea was noted. Thus, a number of trials have supported zinc supplementation as an effective agent in treating and preventing diarrheal disease. Further research is needed to identify the mechanism of action of zinc and to determine its optimal delivery to the neediest populations. The role of zinc supplements in developed countries needs further evaluation. Functional FoodsFunctional foods can be defined as foods that have an effect on physiologic processes separate from their established nutritional function (88). Probiotics have been defined as live microorganisms in fermented foods that promote optimal health by establishing an improved balance in intestinal microflora (89). Reviews have evaluated studies of their use in preventing or reducing the severity or duration of diarrheal illnesses among children (90), including diarrhea caused by rotavirus (91) or associated with antibiotic use (92). These products have included various species of lactobacilli or bifidobacteria or the nonpathogenic yeast Saccharomyces boulardii. The mechanism of action might include competition with pathogenic bacteria for receptor sites or intraluminal nutrients, production of antibiotic substances, and enhancement of host immune defenses (93,94). One meta-analysis concludes that Lactobacillus species are both safe and effective as treatment for children with infectious diarrhea (95). A positive recommendation also emerges from a meta-analysis of probiotic use in antibiotic-associated diarrhea (92). Certain trials included in these reviews were of limited sample size, and negative studies might not have been published. Because dietary supplements (e.g., probiotics) are usually not regulated by the federal government, potential exists for great variability among them, providing a challenge to the prescribing physician to make an informed recommendation regarding their use. Prebiotics differ from probiotics in that they are complex carbohydrates rather than organisms used to preferentially stimulate the growth of health-promoting intestinal flora (96). The oligosaccharides contained in human milk have been called the prototypic prebiotic because they foster growth of lactobacilli and bifidobacteria in the colon of breastfed neonates (97). Data have linked higher intakes of breast milk oligosaccharides with a lowered incidence of acute diarrhea (98). Two randomized trials of prebiotic supplemented infant cereal did not demonstrate a reduced incidence of diarrheal disease among infants and children living in an urban economically depressed area (99). Specific recommendations regarding their use should await further well-controlled human trials. Specific Clinical ScenariosOral rehydration therapy is critical in managing specific types of diarrheal diseases. Acute Bloody Diarrhea (Dysentery)Dysentery is defined as acute bloody diarrhea caused by invasive microbial infection. This does not include occult blood (detected by guaiac card only) or streaks of blood on the surface of formed stool. The treatment of dehydration in dysentery follows the same principles as treatment of acute watery diarrhea. The child with bloody diarrhea is at higher risk for complications, including sepsis and other systemic diseases; therefore, the threshold for admission of such children to the hospital for close observation is lower. Stool cultures are indicated in the setting of acute bloody diarrhea and are helpful for guiding therapy. Food should not be withheld for children with dysentery any more than in other cases of diarrhea. More frequent, smaller meals might be better tolerated, and higher protein intakes have proven beneficial among children recovering from dysentery (100,101). In the majority of cases, empiric antimicrobial agents should not be administered while awaiting culture results, because antimicrobial therapy might not be indicated even when culture results are positive. Amoebiasis is an unusual cause of bloody diarrhea in young children, even in less-developed countries (102). Treatment for amoebiasis should be reserved for those cases in which trophozoites are detected on microscopic examination of the stools (65). Recommendations for therapy of specific enteric pathogens associated with bloody diarrhea are available elsewhere (63--66). Persistent Diarrhea and Diarrhea with Severe MalnutritionThese clinical entities are critical, especially among children of developing countries. Therapy should include oral rehydration when indicated, although the specifics of the evaluation, and fluid, electrolyte, and nutritional management differ and are beyond the scope of this review. The reader is referred to other sources for information regarding these conditions (103,104). Choice of ORSIn 1975, WHO and the United Nations Children's Fund (UNICEF) agreed to promote a single ORS (WHO-ORS) containing (in mmol/L) sodium 90, potassium 20, chloride 80, base 30, and glucose 111 (2%) for use among diverse populations. This composition was selected to allow for a single solution to be used for treatment of diarrhea caused by different infectious agents and associated with varying degrees of electrolyte loss. For example, rotavirus diarrhea is associated with stool sodium losses of approximately 30--40 mEq/L; enterotoxigenic E. coli infection with losses of 50--60 mEq/L; and cholera infection with losses of >90--120 mEq/L (105). WHO-ORS has been demonstrated during >25 years of use to be safe and effective at rehydration and maintenance for children and adults with all types of infectious diarrhea. However, subsequent clinical research, documented in multiple controlled trials and summarized in a meta-analysis (106), has supported adoption of a lower osmolarity ORS (i.e., proportionally reduced concentrations of sodium and glucose). A reduced osmolarity ORS has been associated with less vomiting, less stool output, and a reduced need for unscheduled intravenous infusions when compared with standard ORS among infants and children with noncholera diarrhea. In cholera infection, no clinical difference existed between subjects treated with the lower osmolarity solution and those treated with the standard solution, apart from certain increased incidence of asymptomatic hyponatremia (107). On the basis of those and other findings, UNICEF and WHO organized a consultation on oral rehydration that recommended a reduced osmolarity solution for global use (108). In May 2002, WHO announced a new ORS formulation consistent with these recommendations, with 75 mEq/L sodium, 75 mmol/L glucose, and total osmolarity of 245 mOsm/L (109) (Table 3). The newer hypotonic WHO-ORS is also recommended for use in treating adults and children with cholera, although postmarketing surveillance is under way to confirm the safety of this indication. The composition of commonly available oral rehydration solutions is distinct from other beverages frequently used inappropriately for rehydration (Table 3). New SolutionsRecipes to improve ORS have included adding substrates for sodium co-transport (e.g., the amino acids glycine, alanine, and glutamine) (35) or substituting complex carbohydrates for the glucose (rice and other cereal-based ORS) (36). The amino acid preparations have not been demonstrated to be more effective than traditional ORS, and they are more costly. Rice-based ORS can be recommended where training is adequate and home preparation is preferable, and it can be particularly effective in treating dehydration caused by cholera (36). Nevertheless, given the simplicity and safety of ORS packets in developing countries and of commercially available ORS in developed countries, these remain the first choice for the majority of clinicians. Other potential additives to ORS include substances capable of liberating short-chain fatty acids (e.g., amylase-resistant starch derived from corn) (110) and partially hydrolyzed guar gum (111). The presumed mechanism of action is the enlistment of increased colonic sodium uptake coupled to short-chain fatty acid transport. Other possible future ORS composition changes include addition of probiotics (91), prebiotics, zinc (87), or protein polymers. Barriers to ORTAmong patients, barriers to using ORS and continued nutrition during diarrheal disease include cultural practices (38), lack of parental knowledge (11), lack of training of medical professionals, and cost of commercially available ORS (112). Among physicians, preference for IV hydration, even where evidence indicates improved results from oral rehydration (13,14), remains a major barrier. Patients, even at times under physician supervision, frequently attempt rehydration with solutions bearing no resemblance to physiologically based ORS. The electrolyte content of different fluids commonly used in treating diarrhea do not contain physiologically sound concentrations of carbohydrates and electrolytes, compared with commonly available ORS (Table 3). An informal survey of hospital Internet sites revealed outdated recommendations for treating diarrhea that include nonstandard fluids (unpublished data, Caleb K. King, M.D., University of North Carolina, Chapel Hill, North Carolina). A case report of one child whose care was compromised by following advice obtained from a prominent hospital's Internet site highlights the continued gap between knowledge and practice and the ongoing need to disseminate accurate information regarding oral rehydration (113). ConclusionTreatment of acute diarrhea has relied upon simple and effective therapy of oral rehydration. The critical co-principle in case management of early resumption of feeding of children immediately upon rehydration has also gained wide acceptance. More recent advances in the science of diarrhea treatment include recognition for the role of zinc supplementation in reducing disease severity and occurrence, and development of an oral rehydration solution of lower osmolarity for global use. The combination of oral rehydration and early nutritional support promises to safely and effectively assist a patient through an episode of diarrhea. If the principles of therapy outlined in this report are accepted by all levels of the medical community and if education of parents includes teaching them to begin ORT at home, numerous deaths and unnecessary clinic visits and hospitalizations can be avoided. ORT is suitable for use among children throughout the world (114). References
Management of Acute Gastroenteritis Among Children External: Richard Cash, M.D., Harvard School of Public Health, Boston, Massachusetts; Olivier Fontaine, M.D., World Health Organization, Geneva, Switzerland; William B. Greenough, III, M.D., Johns Hopkins University, Baltimore, Maryland; Ronald E. Kleinman, M.D., Harvard Medical School, Boston, Massachusetts; Myron (Mike) Levine, M.D., University of Maryland, Baltimore, Maryland; David R. Nalin, M.D., West Chester, Pennsylvania; Margaret B. Rennels, M.D., Center for Vaccine Development, Baltimore, Maryland; Mathuram Santosham, M.D, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland; and John Snyder, M.D., University of California Medical Center, San Francisco, California. CDC: James M. Hughes, M.D., and Steve Ostroff, M.D., Office of the Director, National Center for Infectious Diseases (NCID); Caryn Bern, M.D., Division of Parasitic Diseases, NCID; Eric Mintz, M.D., Division of Bacterial and Mycotic Diseases, NCID; Larry Pickering, M.D., Office of the Director, National Immunization Program; and Larry Anderson, M.D., James LeDuc, Ph.D., and Umesh Parashar, M.B.B.S., Division of Viral and Rickettsial Diseases, NCID. Table 1 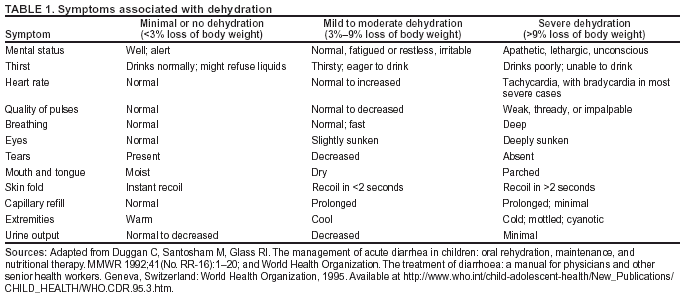 Return to top. Box 1  Return to top. Table 2 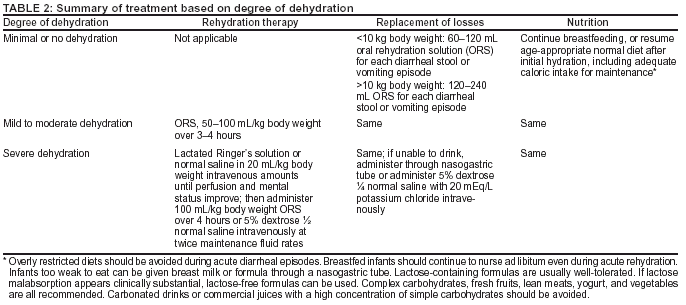 Return to top. Box 2 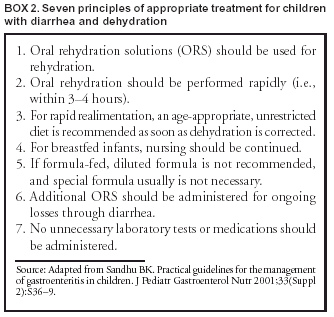 Return to top. Table 3 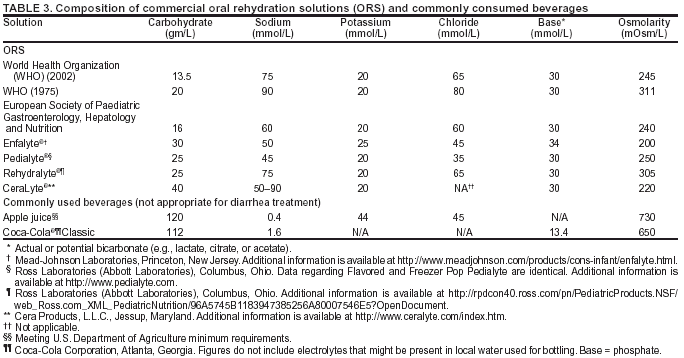 Return to top. Figure 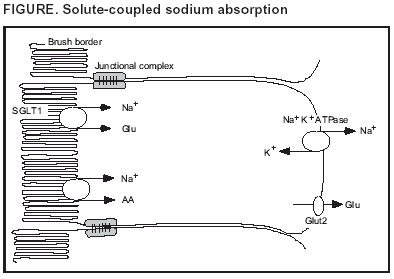 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/10/2003 |
|||||||||
This page last reviewed 11/10/2003
|