Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
Prevalence of Diagnosed Tourette Syndrome in Persons Aged 6--17 Years --- United States, 2007
Tourette syndrome (TS) is an inheritable, childhood-onset neurologic disorder marked by persistent multiple motor tics and at least one vocal tic (1).* Tics are involuntary, repetitive, stereotypic movements or vocalizations that are usually sudden and rapid and often can be suppressed for short periods (1). The prevalence of TS is uncertain; the broad range of worldwide estimates, from 1--30 per 1,000 population (2,3), likely is the result of differences in study methodology. This report presents the first estimate of national prevalence of diagnosed TS among a national sample of U.S. children and adolescents aged 6--17 years. Based on data from the 2007 National Survey of Children's Health (NSCH) (4), the estimated prevalence of a lifetime diagnosis of TS by parent report was 3.0 per 1,000. A diagnosis of TS was almost three times as likely for boys as girls, twice as likely for persons aged 12--17 years than for those aged 6--11 years, and twice as likely for non-Hispanic white persons than for Hispanic and non-Hispanic black persons. Among persons ever diagnosed with TS, 79% also had been diagnosed with at least one co-occurring mental health or neurodevelopmental condition. CDC sponsors efforts by the Tourette Syndrome Association to educate health-care providers and school personnel about TS to ensure earlier identification and promote appropriate medical, educational, and comprehensive behavioral interventions for children with TS and co-occurring mental health or neurodevelopmental conditions.
The 2007 NSCH was the first national, population-based survey of persons aged <18 years that included questions on TS (4). NSCH is a random-digit--dialed telephone (landline only) survey used to estimate the prevalence of a variety of child health and well-being indicators for every state and to examine these indicators together with information on family characteristics and neighborhood environment.†
Telephone interviews (N = 91,642) were completed with parents (or guardians) from April 2007 through July 2008. One child was randomly selected from each household to be the focus of the interview. Complete data on TS were available for 64,034 persons aged 6--17 years. The overall response rate was 46.7%; the cooperation rate was 66.0%.§ Data were weighted to account for unequal probability of selection of each household and child, for nonresponse, and for households without landline telephones. Weights were adjusted further so that estimates reflected the demographic distribution of noninstitutionalized U.S. children and adolescents from the 2007 American Community Survey of the U.S. Census Bureau.
Parents were asked, "Has a doctor or other health-care provider ever told you that [your child] had Tourette syndrome?" Affirmative responses were followed by asking whether the child currently has TS, and if so, whether the parent would describe the child's TS as mild, moderate, or severe (severity was only assessed for current TS). The same series of questions (e.g., current or ever doctor diagnosis) were asked about other co-occurring conditions, including attention-deficit/hyperactivity disorder (ADHD), depression, anxiety problems, behavioral or conduct problems such as oppositional defiant disorder or conduct disorder, and developmental delays affecting a child's ability to learn. Prevalence of parent-reported TS diagnosis (ever and current) among U.S. children, presence of co-occurring conditions, and severity of symptoms among children with current TS were calculated using statistical analysis software to account for the complex sampling design of NSCH.
All estimates in this report reflect persons aged 6--17 years. Estimates for children aged <6 years had high relative standard errors (>0.3) and are not reported. The estimated prevalence for ever receiving a TS diagnosis, by parent report, was 3.0 per 1,000, representing approximately 148,000 children (95% confidence interval [CI] = 111,000--197,000) (Table) in the United States. A diagnosis of TS was approximately three times as likely for boys compared with girls, and approximately twice as common in persons aged 12--17 years compared with those aged 6--11 years. Non-Hispanic white children were twice as likely as non-Hispanic black children and Hispanic children to have a parent-reported TS diagnosis. No differences were noted by parental education or household income. Among children ever diagnosed with TS, 79% also had been diagnosed with at least one co-occurring mental health or neurodevelopmental condition (Figure): 64% had been diagnosed with ADHD, 43% with behavioral or conduct problems, 40% with anxiety problems, 36% with depression, and 28% with a developmental delay affecting the child's ability to learn.
Among children with a TS diagnosis, 62% (weighted N = approximately 92,000, CI = 65,000--131,000) were described as currently having TS. Most current cases were described as mild, and 27.1% (CI = 15.0--43.8) were rated as moderate or severe. Persons aged 6--13 years were more likely than those aged 14--17 years to currently have TS (82.6% versus 42.1%, p<0.01). Differences between the 6--11 years and 12--17 years age groups were not statistically significant.
Reported by: L Scahill, PhD, Yale Univ Child Study Center and School of Nursing. RH Bitsko, PhD, SN Visser, MS, Div of Human Development and Disability, National Center on Birth Defects and Developmental Disabilities; SJ Blumberg, PhD, Div of Health Interview Statistics, National Center for Health Statistics, CDC.
Editorial Note:
Worldwide estimates of TS from population-based studies have ranged from 1 to 30 per 1,000 persons (2,3,5). This wide variation likely results from differences in sample size, population source, sample age, diagnostic criteria, and study methods (e.g., parent report, teacher report, and direct observation). TS prevalence described in recent community-based studies ranges from 3.0--8.0 per 1,000 persons (3,5--7).
This report provides the first prevalence estimate of diagnosed TS based on parent report from a nationally representative sample of U.S. children and adolescents. TS is a neurologic condition with genetic predisposition and childhood onset. Tic severity often peaks in adolescence and often declines by early adulthood (8). TS is more common in boys than girls (1--3,9). Children with TS experience associated problems related to academic and work performance and family and peer relationships (3). A TS diagnosis might be delayed or missed if symptoms are atypical, mild, attributed to alternate etiology (e.g., blinking mistaken for visual problem or sniffles mistaken for seasonal allergies), or in children with limited access to specialty health care (e.g. pediatric neurologist or child psychiatrist).
Many studies have reported male-to-female TS prevalence ratios of at least 4:1 (3,9,10). This is consistent with the higher prevalence of TS diagnosis among boys observed in the NSCH data. The reason boys are more likely than girls to express symptoms of TS is unclear and is likely the result of a combination of genetic, hormonal, and environmental factors (1,8).
The higher lifetime prevalence among older children is consistent with the known age distribution. Although average age of tic onset is 5--7 years, the course is often insidious (8). Severity often peaks between ages 10 and 12 years (8). Thus, the onset of TS symptoms might not be recognized immediately by parents or diagnosed by a clinician. After tic severity peaks, it might decline sufficiently that parents will no longer report that their child has TS. Among all children ever receiving a TS diagnosis, current TS was less likely to be reported for persons aged 14--17 years. However, impairment can endure into adulthood (8), and early identification and intervention might improve social, educational, and employment outcomes for persons with TS.
Consistent with community-based studies (2,9), approximately three fourths of children in this study with a current TS diagnosis had mild TS, according to their parents. Even when TS is mild, however, commonly associated co-occurring conditions such as ADHD and obsessive compulsive disorder might contribute to overall impairment (2,10).
The survey-based prevalence estimate described in this report is based on parent report of a TS diagnosis. The detection and diagnosis of TS is less likely for children with limited access to specialty health-care services (2). Thus, the observed survey-based prevalence of 3.0 per 1,000 likely is an underestimate of TS prevalence in children. Results from community-based studies that independently evaluate children for TS and do not rely on parent-reported diagnosis invariably identify cases that were previously not diagnosed (3,6,9). In addition, many children identified as having TS in community-based studies were not receiving mental health services (2,6,9). This suggests that primary-care practices and schools might be important settings to improve recognition and referral.
The survey-based prevalence estimates revealed that non-Hispanic black children and Hispanic children had a lower probability of TS diagnosis compared with non-Hispanic white children. Community-based studies of TS have lacked adequate sample size to determine prevalence for racial or ethnic groups. Differences in the prevalence of TS among racial and ethnic groups might result from biologic risk or disparities in access to specialty health care. The gap between prevalence reported in community-based studies and survey-based prevalence described in this report among non-Hispanic blacks and Hispanics is greater than the gap between reports from community-based studies and the survey-based prevalence among non-Hispanic whites. These gaps support the view that differences in reported prevalence are at least partially attributable to differences in access to care. The lack of association between income and parent education with TS diagnosis suggests that other factors might affect the racial and ethnic differences. Research in communities with adequate representation of minority and underserved populations is needed to clarify the reasons for the differences in prevalence.
The findings in this report are subject to at least four limitations. First, symptoms consistent with TS must be recognized to establish a diagnosis. Some cases might remain undetected because of lack of awareness or access to medical care. Second, families who did not speak English, Spanish, or one of four Asian languages (Cantonese, Korean, Mandarin, or Vietnamese) were excluded from the survey (4). Third, the presence of co-occurring conditions and reported severity might be subject to recall error. Finally, the results are subject to biases associated with telephone surveys, including the exclusion of households without landlines and low response rates relative to population-based, face-to-face surveys.
Impairment in learning, school performance, and social competence can result from tics or co-occurring conditions (2). Clinical assessment and treatment of children with TS warrants attention to tics and co-occurring conditions to reduce overall impairment. The degree of impairment and spectrum of co-occurring conditions varies and therefore the treatment should be tailored to address the individual's type and severity of symptoms. Assessment by a specialist (e.g. pediatric neurologist or child psychiatrist), might provide the best available treatment options (e.g., behavioral or pharmacologic interventions). If academic or behavioral performance is of concern, referrals for educational interventions designed to reduce the effect of tics and co-occurring disruptive behavioral problems on learning should be considered.
Defining lifetime prevalence is an important step in defining the public health impact of TS. Although symptoms of TS might disappear in some cases by early adulthood, symptoms of co-occurring conditions can persist. CDC is conducting surveillance, research, and outreach activities to document the impact of TS and improve its recognition. CDC sponsors the Tourette Syndrome Association to provide authoritative education for physicians and allied health care workers, including school personnel, about TS treatment and the effects of the disorder. The programs increase access to accurate and scientifically valid information on the recognition, diagnosis, and treatment of TS, with a view toward improved health and developmental outcomes.
Acknowledgments
This report is based, in part, on contributions from Maternal Child Health Bur, Health Resources and Svcs Admin, US Dept of Health and Human Svcs.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000.
- Scahill L, Sukhodolsky DG, Williams SK, Leckman JF. Public health significance of tic disorders in children and adolescents. Adv Neurol 2005;96:240--8.
- Khalifa N, von Knorring AL. Prevalence of tic disorders and Tourette syndrome in a Swedish school population. Dev Med Child Neurol 2003;45:315--9.
- Blumberg SJ, Foster EB, Frasier AM, et al. Design and operation of the National Survey of Children's Health, 2007. Vital Health Stat 1 (in press).
- Stefanoff P, Wolanczyk T, Gawrys A, et al. Prevalence of tic disorders among schoolchildren in Warsaw, Poland. Eur Child Adolesc Psychiatry 2008;17:171--8.
- Hornsey H, Banerjee S, Zeitlin H, Robertson M. The prevalence of Tourette syndrome in 13--14-year-olds in mainstream schools. J Child Psychol Psychiatry 2001;42:1035--9.
- Scahill L, Williams S, Schwab-Stone M, Applegate JO, Leckman JF. Tic disorders and disruptive behavior in a community sample. Adv Neurol 2006;99:184--90.
- Leckman JF, Zhang H, Vitale A, et al. Course of tic severity in Tourette syndrome: the first two decades. Pediatrics 1998;102:14--9.
- Kadesjo B, Gillberg C. Tourette's disorder: epidemiology and comorbidity in primary school children. J Am Acad Child Adolesc Psychiatry 2000;39:548--55.
- Sukhodolsky DG, Scahill L, Zhang H, et al. Disruptive behavior in children with Tourette's syndrome: association with ADHD comorbidity, tic severity, and functional impairment. J Am Acad Child Adolesc Psychiatry 2003;42:98--105.
* Diagnostic criteria for Tourette syndrome include 1) the presence of multiple motor and one or more vocal tics at some time during the illness, although not necessarily concurrently; 2) occurrence of tics many times a day, nearly every day, or intermittently throughout a period of more than 1 year, with no tic-free period of more than 3 consecutive months; 3) onset before age 18 years; and 4) symptoms not caused by direct physiologic effects of a substance or a general medical condition (1).
† Additional information about NSCH is available at http://www.cdc.gov/nchs/about/major/slaits/nsch07.htm. National and state-based estimates for more than 100 indicators from the NSCH are available at http://nschdata.org.
§ The response rate is the percentage of households that completed interviews among all eligible households, including those that were not successfully contacted. The cooperation rate is the percentage of households that completed interviews among all eligible households that were contacted. NSCH attempts to minimize nonresponse bias by incorporating nonresponse adjustments in the development of the sampling weights.
|
TABLE. Prevalence of ever receiving a diagnosis of Tourette syndrome among persons aged 6--17 years, by selected characteristics* --- National Survey of Children's Health, United States, 2007 |
||||||
|---|---|---|---|---|---|---|
|
Characteristic |
No. in sample (unweighted)† |
No. with reported diagnosis (unweighted) |
Weighted prevalence per 1,000 |
(95% CI§) |
Prevalence ratio |
(95% CI) |
|
Total surveyed |
64,034 |
225 |
3.0 |
(2.3--4.0) |
--- |
--- |
|
Age (yrs) |
|
|||||
|
6--11 |
27,776 |
61 |
1. 9 |
(1.2--2.9) |
Referent |
Referent |
|
12--17 |
36,258 |
164 |
4.0 |
(2.8--5.9) |
2.1 |
(1.2--3.8) |
|
Sex |
|
|||||
|
Male |
33,264 |
179 |
4.4 |
(3.2--6.1) |
2.9 |
(1.4--6.0) |
|
Female |
30,680 |
46 |
1.5 |
(0.8--2.9) |
Referent |
Referent |
|
Ethnicity/Race |
|
|||||
|
Hispanic |
7,347 |
26 |
1.6 |
(0.9--2.8) |
0.4 |
(0.2--0.8) |
|
Non-Hispanic white |
43,766 |
164 |
3.9 |
(2.7--5.6) |
Referent |
Referent |
|
Non-Hispanic black |
6,445 |
18 |
1.5 |
(0.9--2.7) |
0.4 |
(0.2--0.8) |
|
Highest level of education achieved |
|
|||||
|
High school diploma or less |
14,902 |
58 |
3.5 |
(2.0--6.0) |
1.3 |
(0.7--2.4) |
|
At least some college or technical school |
48,376 |
165 |
2.7 |
(2.0--3.8) |
Referent |
Referent |
|
Household income |
|
|||||
|
≤200% of federal poverty level (FPL¶) |
17,646 |
65 |
3.1 |
(1.8--5.2) |
1.1 |
(0.4--3.2) |
|
>200% to ≤400% above FPL |
21,875 |
80 |
3.0 |
(1.8--5.1) |
1.0 |
(0.3--3.2) |
|
>400% above FPL |
24,512 |
80 |
2.9 |
(1.9--4.4) |
Referent |
Referent |
|
* As reported by parents. † The sum of the sample sizes might not equal the total surveyed because some parents did not know or refused to provide an answer to the question about the characteristic. Missing data for family income were derived using multiple imputation techniques (4). Missing data for other characteristics were not imputed. § Confidence interval. ¶ Poverty guidelines for 2007 available at http://aspe.hhs.gov/poverty/07fedreg.pdf. |
||||||
FIGURE. Prevalence of selected diagnoses* among persons aged 6--17 years who have ever received a diagnosis of Tourette syndrome (TS),† by parent report --- National Survey of Children's Health, United States, 2007
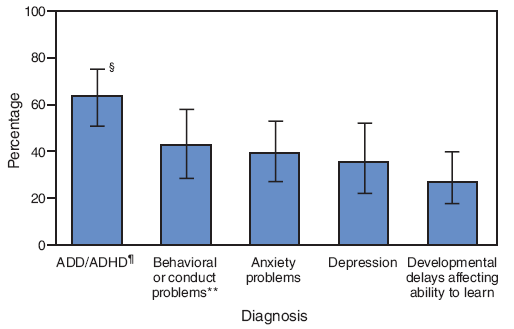
* Selected diagnoses included mental health and neurodevelopmental conditions asked about on the survey, including attention-deficit/hyperactivity disorder (ADHD), behavioral or conduct problems, anxiety problems, depression, and developmental delays.
† Among children ever diagnosed with TS, 79% also had been diagnosed with at least one other selected diagnosis. Among children who currently have TS, 73% currently have at least one additional selected diagnosis.
§ 95% confidence interval.
¶ Attention-deficit disorder or attention-deficit/hyperactivity disorder, by parent report.
** Such as oppositional defiant disorder or conduct disorder, by parent report.
Alternative Text: The figure above shows the prevalence of selected diagnoses among persons aged 6-17 years who have ever received a diagnosis of Tourette Syndrome by parent report in the United States in 2007. Among children ever diagnosed with TS, 79% also had been diagnosed with at least one co-occurring mental health or neurodevelopmental condition. Sixty-four percent had been diagnosed with ADHD, 43% with behavioral or conduct problems, 40% with anxiety problems, 36% with depression, and 28% with a developmental delay affecting the child's ability to learn.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 6/3/2009


