Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail.
HIV Infection --- Guangdong Province, China, 1997--2007
In 2007, an estimated 700,000 persons in China were living with human immunodeficiency virus (HIV) infection. An estimated 50,000 new HIV infections and 20,000 deaths related to acquired immunodeficiency syndrome (AIDS) occurred in 2007, and an estimated 71% of persons with HIV infection were unaware of their HIV status (1). In 2007, 40.6% of those living with HIV had been infected through heterosexual transmission and 38.1% through injection-drug use (1,2). Guangdong Province in southeastern China is the country's most populous province, with an estimated 75.6 million permanent residents and 16.5 million migrants (3); the province has undergone rapid economic development (4). Since 1986, a case-based surveillance system (CBSS) in China has collected data on persons infected with HIV, including demographic characteristics and transmission categories. To assess recent trends in HIV infection in the province, the Guangdong Center for Disease Control, with technical assistance from CDC, analyzed CBSS data for the period 1997--2007. The results of that analysis indicated that the number of HIV cases increased from 102 in 1997 to 4,593 in 2007, although this increase resulted, in part, from expanded testing and surveillance. Among males classified by HIV transmission category, 82.1% of newly diagnosed infections were attributed to injection-drug use. Among females classified by HIV transmission category, 53.7% engaged in high-risk heterosexual conduct. Despite substantial methodologic limitations, these results can be useful to Guangdong public health agencies in targeting and evaluating HIV prevention, care, and treatment programs.
Instituted in 1985 as a paper-based system, CBSS was transitioned to a web-based system in 2004. CBSS data regarding HIV infection and patient characteristics are collected from multiple disparate sources: 1) routine HIV testing at 415 hospitals; 2) HIV testing at 72 counseling and testing centers (5); 3) annual sentinel surveillance HIV testing conducted nationally and at 65 sites in Guangdong Province among consecutively enrolled female sex workers,* injection-drug users,† persons who visit sexually transmitted infection (STI) clinics,§ and pregnant women who visit prenatal clinics for the first time (2,3); 4) biannual behavioral surveillance that collects comprehensive data regarding HIV knowledge and attitudes and sexual risk behavior among sex workers, STI patients, and youths aged ≤16 years enrolled in behavioral surveillance schools; 5) special surveys in 2003, 2005, and 2006 among sex workers and men who have sex with men (MSM) collecting comprehensive HIV-related behavioral data¶ (3); and 6) routine HIV screening for blood donation (6). Data from all components of CBSS are aggregated by the provincial government and currently cannot be analyzed by an individual component.
Regardless of collection site, all specimens are first tested with an enzyme-linked immunosorbent assay (ELISA). Reactive specimens are retested using a second ELISA or rapid test; if the specimen is reactive to one or both tests, a confirmatory Western blot test is performed. All specimens testing positive by Western blot are classified as HIV positive. AIDS cases are defined by laboratory-confirmed HIV infection plus any AIDS-defining condition or CD4 count <200 cells/µL (7). Each HIV-positive laboratory result is returned to local public health staff members, who complete a case card with demographic data, behavioral data, and likeliest transmission category based on initially collected information or patient interview.** Case cards are sent to provincial public health staff or local hospitals, where data are entered into CBSS. As required by Chinese law, HIV-positive patients are reported by name, and duplicate cases are removed by provincial public health staff members (3).††
During 1997--2007, an aggregate total of 22,571 newly diagnosed HIV cases were reported in Guangdong Province: 18,525 (82.1%) in males and 4,046 (17.9%) in females (Table). Among the 11,613 (62.7%) males classified by transmission category, 9,534 (82.1%) of HIV cases were attributed to injection-drug use, followed by 1,535 (13.2%) attributed to high-risk heterosexual contact.§§ Among the 2,322 (57.4%) females classified by transmission category, 1,247 (53.7%) of HIV cases were attributed to high-risk heterosexual contact, followed by 905 (39.0%) attributed to injection-drug use. Among the 12,929 (60.8%) males with known residency, 8,774 (67.9%) were Guangdong Province residents; among the 2,720 (67.2%) females with known residency, 1,483 (54.5%) were residents. Dividing Guangdong Province into central, east, and west regions,¶¶ 14,606 (78.8%) of HIV cases among males and 3,366 (83.2%) of cases among females were reported in the central region (Table).
Over time, the number of newly diagnosed HIV cases increased from 102 (86 in males and 16 in females) in 1997 to 4,593 (3,524 in males and 1,069 in females) in 2007 (Figure 1). From 2003 to 2005, the total number of newly diagnosed HIV cases increased threefold, from 1,284 (1,052 in males and 232 in females) to 5,223 (4,501 in males and 722 in females). However, from 2005 to 2007, although cases in females increased 48.1%, cases in males decreased 21.7% (Figure 1).
Every year during 1997--2007, injection-drug use was the most commonly reported transmission category in newly diagnosed HIV cases (Figure 2). From 2003 to 2005, the number of cases attributed to injection-drug use increased from 639 to 2,344, then decreased to 1,680 in 2007. In contrast, the number of cases attributed to high-risk heterosexual contact increased from 138 in 2003 to 403 in 2005, then increased to 1,015 in 2007.
Reported by: P Lin, MD, Y Wang, MD, Y Li, MD, Institute of HIV/AIDS, Guangdong Center for Disease Control. J Liu, MPH, J Zhao, MD, Global AIDS Program China; A Kim, PhD, Div of Global AIDS; M Chen, MS, Div of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; N Shah, MD, EIS Officer, CDC.
Editorial Note:
The findings in this report indicate that the number of reported newly diagnosed HIV cases in Guangdong Province, China, increased steadily from 1997 to 2003, then rose sharply. The substantial increase in cases likely resulted in part from a 2003 national initiative to expand and intensify testing services and surveillance efforts, including the transition of CBSS to a web-based system in 2004 (1,8). Contributing to the rise in HIV cases were expansion of surveillance sites from 43 to 70 in Guangdong Province in 2004 and active case-finding through special surveys of populations at high risk conducted during 2003--2006 (3).
The recent increase in reported HIV cases attributed to high-risk heterosexual contact and the decline in cases attributed to injection-drug use might suggest a shift in Guangdong's HIV epidemic similar to the national trend, in which heterosexual transmission was the main transmission category in China in 2007 (3,8). In the central region of Guangdong Province, where approximately 80% of the province's HIV cases were reported in 2007, rapid economic growth has led to an influx of migrant workers. Migrant women who lack appropriate job skills or who seek to supplement the family income might become sex workers, and migrant men living apart from their spouses might become clients of sex workers (6).
Analyses completed for this report could only be conducted on aggregate data from multiple disparate sources with different methods of sampling. Ideally, trend analysis should be conducted using data that are specific to each surveillance method and consistent over time. Such methods are not yet possible in Guangdong province. However, the aggregate CBSS data, although imperfect, provide an important window into reporting of HIV cases across age, sex, and transmission categories essential for understanding the HIV epidemic in the province, allow identification of the most obvious changes in the dynamics of the HIV epidemic, and recognize key populations at risk. These CBSS data also are instrumental for programmatic resource allocation related to HIV care and treatment. Furthermore, despite the limitations imposed by aggregation, results are consistent with national trends and data from other provinces (1,2,6,8,9).
The findings in this report are subject to at least three other limitations. First, large percentages of data were missing for key HIV case characteristics analyzed. For example, for approximately 22% of cases, the patient age group was unknown, and approximately 38% of patients were not classified by transmission category. Second, because definitions for sex worker and injection-drug user were institution based (10), verification was not possible. Finally, because HIV-positive persons in CBSS are required by law to report their names and national identification numbers, those consenting to HIV testing likely represent a sample that is biased in unpredictable ways.
Although Guangdong Province has made considerable progress in HIV case-based surveillance, improvements can be made that will increase the ability to identify those in need of care (2). Currently, China is working on improvements to CBSS that will allow separate data analyses of sentinel and behavioral surveillance data and improve data quality and analysis. Additionally, more community-based sampling of populations at high risk are being planned to provide a more complete picture of the HIV epidemic in Guangdong for prevention programming and resource allocation (2,10). Sentinel surveillance methods also should be redefined so that they rely less extensively on institutions and more accurately represent those populations at greatest risk (10). Finally, because an estimated 71% of persons with HIV infection in China are unaware of their status (1), more provider-initiated HIV counseling and testing should be considered to help reduce stigma, increase case-finding, and link more HIV patients with treatment and counseling (8).
Acknowledgments
This report is based, in part, on contributions by Z Wu, MD, National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention; Guangzhou Sexually Transmitted Infection Clinic, Maternal and Infant Hospital of Guangzhou; Guangzhou District Center for Disease Control and Prevention; Foshan District Center for Disease Control and Prevention; Shunde District Center for Disease Control and Prevention; R Shiraishi, PhD, T Diaz, MD, K Sabin, PhD, Div of Global AIDS, and M Bulterys, MD, Global AIDS Program China, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention.
References
- State Council AIDS Working Committee Office, UN Theme Group on AIDS in China. A joint assessment of HIV/AIDS prevention, treatment and care in China (2007). Available at http://www.undp.org.cn/downloads/otherlocal/hiv/20080104.pdf.
- Sun X, Wang N, Li D, et al, The development of HIV/AIDS surveillance in China. AIDS 2007;21(Suppl 8):S33--8.
- Global AIDS Program, CDC; National Center for AIDS/STD Prevention and Control, China CDC; and Guangdong Provincial Center for Disease Control and Prevention. Evaluation of the Guangdong HIV/AIDS Surveillance System, China; 2008.
- Bui TX, Yang DC, Jones WD, Li JZ, eds. China's economic powerhouse: economic reform in Guangdong Province. New York, NY: Palgrave Macmillan; 2003.
- Ma W. HIV testing and counseling in China. In: Joint WHO/UNICEF/UNAIDS technical consultation on scaling-up HIV testing and counseling in Asia and Pacific. Phnom Penh, Cambodia, June 4--6, 2007.
- Qian HZ, Vermund SH, Wang N. Risk of HIV/AIDS in China: subpopulations of special importance. Sex Transm Infect 2005;81:442--7.
- Chinese Medical Association, Chinese Center for Disease Control and Prevention. Guidelines for diagnosis and treatment of HIV/AIDS in China. Chin Med J 2006;119:1589--1608.
- Wang L. Overview of the HIV/AIDS epidemic, scientific research and government responses in China. AIDS 2007;21 (Suppl 8):S3--7.
- Lu L, Jia M, Ma Y, et al. The changing face of HIV in China. Nature 2008; 455:609--11.
- Jia Y, Lu F, Sun X, Vermund SH. Sources of data for improved surveillance of HIV/AIDS in China. Southeast Asian J Trop Med Public Health 2007;38:1041--52.
* Defined as all women who entered sex work reeducation centers. For behavioral surveillance, sex workers also were identified from venues where sex is known to be sold, including public bath houses and karaoke bars.
† Defined as all persons who have entered drug detoxification centers. Although some of these persons might have used oral drugs (e.g., opium or morphine) exclusively, data regarding specific drug type and methods of use were not recorded by CBSS. Therefore, all who entered drug detoxification were presumed to have injected drugs.
§ Defined as persons aged ≥13 years who visit sentinel surveillance STI clinic for the first time.
¶ Peer-referral sampling methods were used in which initial participants were recruited and asked to recruit peers, with recruitment continuing for multiple waves of peer referrals.
** Case card data include national identification number, medical record number, patient name, ethnicity, marital status, education, address, concurrent infection (i.e., syphilis, gonorrhea, chlamydia, genital warts, or genital herpes), injection-drug use, recent surgeries, occupational exposure, blood donation, STI, HIV-positive mother, nonmarital heterosexual contact, HIV-positive stable partner, most likely transmission category, laboratory test result, date of AIDS diagnosis, date form completed, and reporting facility.
†† All participants provide oral consent for confidential-linked HIV testing, are offered their test results, and are responsible for retrieval. If the test result is HIV positive and results are not retrieved, the patient is contacted by public health staff members based on demographic and behavioral data at the time of specimen collection.
§§ Includes heterosexual sex workers or their clients, and heterosexual sex partners of persons living with HIV infection.
¶¶ Central region: Guangzhou, Shenzhen, Zhuhai, Foshan, Zhongshan, Jiangmen, and Dongguan prefectures. East region: Shaoguan, Shanwei, Heyuan, Huizhou, Chaozhou, Meizhou, Shantou, and Jieyang prefectures. West region: Zhanjiang, Zhaoqing, Qingyuan, Maoming, Yunfu, and Yangjiang prefectures.
FIGURE 1. Newly diagnosed HIV cases, by sex and year of diagnosis --- case-based surveillance system (CBSS), Guangdong Province, China, 1997--2007*
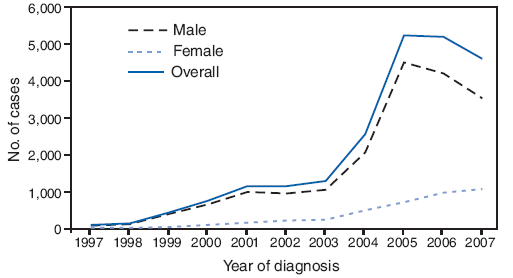
The figure above indicates the number of newly diagnosed HIV cases, by sex and year of diagnosis in Guangdong Province, China, during 1997–2007. Source of the data is China’s case-based HIV surveillance system.
In 1997, overall, 102 newly diagnosed HIV cases were reported, including 86 among males and 16 among females. In 1999, overall, 442 cases were reported, including 401 among males and 42 among females. In 2000, overall, 747 cases were reported, including 648 among males and 99 among females. In 2001, overall, 1,150 cases were reported, including 999 among males and 151 among females. In 2002, overall, 1,157 cases were reported, including 942 among males and 215 among females. In 2003, overall, 1,284 cases were reported, including 1,052 among males and 232 among females. In 2004, overall, 2,548 cases were reported, including 2,055 among males and 493 among females. In 2005, overall, 5,223 cases were reported, including 4,501 among males and 722 among females. In 2006, overall, 15,180 cases were reported, including 4,200 among males and 980 among females. In 2007, overall, 4,593 cases were reported, including 3,524 among males and 1,069 among females.* CBSS collects data regarding persons with HIV infection from various disparate sources, including routine HIV testing, sentinel surveillance testing of certain populations, behavioral surveillance, and special surveys. Data from all components of CBSS are aggregated by the provincial government and cannot be analyzed on an individual survey level.
FIGURE 2. Newly diagnosed HIV cases, by transmission category and year of diagnosis --- case-based surveillance system (CBSS), Guangdong Province, China, 1997--2007*
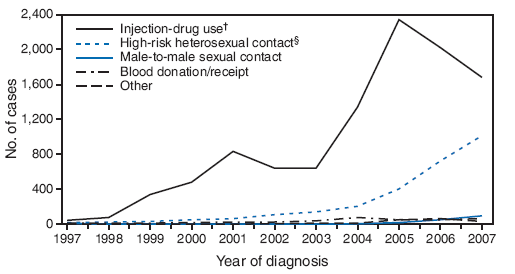
The figure above indicates the number of newly diagnosed HIV cases, by transmission category and year of diagnosis in Guangdong Province, China, during 1997–2007. Source of the data is China’s case-based HIV surveillance system. The data show that every year during 1997–2007, injection-drug use was the most commonly reported transmission category in newly diagnosed HIV cases. From 2003 to 2005, the number of cases attributed to injection-drug use increased from 639 to 2,344, then decreased to 1,680 in 2007. In contrast, the number of cases attributed to high-risk heterosexual contact increased from 138 in 2003 to 403 in 2005, then increased to 1,015 in 2007.
* CBSS collects data regarding persons with HIV infection from various disparate sources, including routine HIV testing, sentinel surveillance testing of certain populations, behavioral surveillance, and special surveys. Data from all components of CBSS are aggregated by the provincial government and cannot be analyzed on an individual survey level.
† Includes all persons who enter drug detoxification centers, all of whom are presumed to have injected drugs.
§ Includes heterosexual sex workers or their clients, and heterosexual sex partners of persons living with HIV infection.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services. |
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices.
**Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 4/22/2009


