 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Cholera Outbreak --- Southern Sudan, 2007Vibrio cholerae causes cholera, an acute infectious diarrheal disease that can result in death without appropriate therapy, depending on the severity of the disease (1). War, poverty, inadequate sanitation, and large numbers of refugees and internally displaced persons (IDPs) are major precursors to cholera outbreaks (2). In 2005, Southern Sudan ended its 22-year civil war with North Sudan; as a result, IDPs and refugees are returning to the south (3,4). During April--June 2007, investigators from the Southern Sudan Field Epidemiology and Laboratory Training Program (SS-FELTP) and CDC investigated a cholera outbreak in the town of Juba, Southern Sudan. This report summarizes the results of that investigation, which found that 3,157 persons were diagnosed with suspected cholera during January--June 2007, with 74 deaths resulting from the disease. An environmental investigation revealed suboptimal hygiene practices and a lack of water and sanitation infrastructure in Juba. A case-control study indicated that persons less likely to have cholera were more likely to have consumed hot meals containing meat during the outbreak. Contaminated food or water were not identified as possible sources of the cholera outbreak in Juba. However, this might be attributed to limitations of the study, including small sample size. Cholera can reach epidemic proportions if adequate control measures are not implemented early. Mass media campaigns are important for current and new residents in Juba to understand the importance of proper food handling, clean water, and optimal hygiene practices to prevent the spread of cholera. After the civil war with North Sudan ended in 2005, displaced residents began returning to Juba. Juba is a major urban area in Central Equatoria State and is considered the unofficial capital of Southern Sudan. Housing in Juba for returning residents consisted of informal and formal settlements that included old brick homes, tent camps, and mud thatch houses. The major water sources were borehole well pumps, shallow watering holes, the Nile River, and tanker trucks. Latrines and indoor plumbing were lacking; as a result, some residents used open fields for defecation. Juba had one large open-air marketplace, in which persons could shop for food items, and very few restaurants. In February 2006, a large cholera outbreak began in Juba, resulting in 6,329 suspected infections as of June 2006, with sporadic cases continuing throughout the year. Epidemiologic InvestigationCDC's Coordinating Office for Global Health received a request for technical assistance from SS-FELTP in March 2007 to investigate a second large cholera outbreak in Juba. Investigators arrived at the end of April 2007, after the outbreak had peaked (weeks 10--11) (Figure) and after information about cholera prevention had been communicated to Juba residents. At the time of the investigation, Southern Sudan's Ministry of Health (MOH) was conducting a cholera prevention campaign that included radio prevention messages and community education forums. MOH defined a suspected cholera case as illness in a person of any age with acute watery diarrhea during the 2007 outbreak. Contaminated water and food were hypothesized to be the main sources of cholera in Juba based on previous cholera studies conducted in Africa (1,2) and the lack of sanitation infrastructure observed in Juba. Potential risk factors for cholera were identified after discussions with persons living in Juba and health officials about possible routes of transmission. A review of the weekly surveillance records kept jointly by the World Health Organization (WHO) Juba office and MOH identified 3,157 persons with diagnoses of suspected cholera (case fatality rate: 2%) during January--June 2007 in Juba. The outbreak peaked in March and ended in June 2007. However, isolated cases continued for the remainder of 2007. Information on the number of persons infected with cholera was obtained from the Juba Teaching Hospital (JTH), cholera treatment centers coordinated by Medecins Sans Frontiers (MSF), and other local hospitals and clinics. A review of records from JTH revealed that information on sex, age, and symptoms was incomplete in the hospital admissions logbook. Environmental InvestigationLatrines, chlorine for treating water, and soap were lacking in Juba. Residents collected water from borehole pump wells using jerry cans (large plastic containers with small openings), the Nile River, and tanker trucks selling untreated Nile River water. Upon initial inspection, investigators observed an open defecation field near the Nile River, pit latrines built uphill from nearby borehole wells, and several wells closed because of contamination. Case-Control StudyA prospective matched case-control study was conducted during May 24--June 5 by SS-FELTP trainees and CDC investigators. A questionnaire was developed that included demographic characteristics, symptoms, potential exposures (e.g., related to food, water, personal hygiene, and sanitation), large gatherings (e.g., funerals and weddings), and knowledge of cholera prevention. Case-patients were identified upon admission to the infectious disease ward at JTH. For the purposes of the study, a case was defined as illness in a person of any age with acute watery diarrhea (with or without vomiting) in the 4 days before arriving at JTH. Selection of case-patients was consecutive. All persons admitted to JTH during May 24--June 5 who met the case definition were included in the study. Two case-patients died before they could be enrolled in the study and thus were excluded. Among those households with more than one case-patient, only the first ill person was enrolled in the study; secondary cases were excluded. Interviewers traveled to each case-patient's place of residence and matched each case-patient to two community controls by age (within 5 years), sex, and neighborhood. Selected control residences were chosen randomly and could not be residences that were adjacent to the case-patient's residence. Persons living next to the case-patients' residences might have been more likely to also be infected with cholera because many of the home communes observed belonged to the same family, and members shared meals, latrines (if existing), and courtyards. Controls and their household members had no history of diarrhea since January 2007. Case-patients were interviewed in the hospital, and controls were interviewed in their residences. Information was collected on 42 cases and 81 controls. Both bivariate (chi-square) and multivariable (conditional logistic regression) analyses were performed. The multivariable analysis included all variables that were significant (p<0.05) in the bivariate analysis. Stool specimens gathered by rectal swabs from 10 case-patients with suspected cholera who had not received antimicrobial treatment by a certified laboratory technologist were stored in Cary-Blair medium and shipped to the Kenya Medical Research Institute (KEMRI) laboratory in Nairobi, Kenya. Because of limited resources, only 10 specimens were shipped to KEMRI. The median age of both case-patients and controls was 30 years (range: 3--60 years); 2% of case-patients and 1% of controls were aged <5 years. Approximately half (52%) of the case-patients entered the hospital within 1 day of becoming ill (Table 1). Other symptoms included vomiting, fever, and leg cramps. One third of the case-patients were reported as being severely dehydrated based on the nursing notes in the medical chart. Treatment consisted of oral fluids, tetracycline, doxycycline, and intravenous fluids and varied among case-patients. The majority of case-patients received intravenous fluids, but not all received oral fluids, tetracycline, or doxycycline. The unadjusted matched analysis (Table 2) indicated that persons who 1) self-identified as visitors to Juba (matched odds ratio [mOR] = 5.6); 2) had lived less than 1 year in Juba (mOR = 4.6); and 3) chose a water source close to their place of residence (i.e., <20 meters [mOR = 3.2]) were at greater odds of having cholera, all significant associations at p<0.05. Using tanker trucks drawing water from the Nile River as the main source of drinking water was not significantly associated with cholera. A significant association was observed for persons who did not treat their water (when compared with those who used chlorine treatment) were found to be at less risk for cholera (mOR = 0.2). No significant associations were observed between cholera and hygiene-related factors (i.e., using soap to wash hands before eating or after defecation, and having soap present in the house) or eating leftover foods. Consuming a meal with fish served hot in the 3 days before becoming ill (case-patients) and before being interviewed (controls), was significantly protective for cholera (mOR = 0.3). A similar significant protective association was found for hot meals containing meat (mOR = 0.2). No significant associations with other local food items or attendance at large gatherings (e.g., funerals or weddings) were identified. After the significant variables from the bivariate analysis were included in a multivariable analysis, only consuming at least one hot meal containing meat in the 3 days before becoming ill (case-patients) or before being interviewed (controls) (adjusted mOR = 0.3 [95% confidence interval = 0.1--0.9], p = 0.03) was associated with a lowered risk for cholera. Laboratory ResultsSix of the 10 rectal swabs collected from the case-patients in the case-control study before antimicrobial treatment was started yielded Vibrio cholerae biotype El Tor, serogroup O1, serotype Inaba. This type was resistant to sulfatrimethoprim, nalidixic acid, sulfisoxazole, streptomycin, and furazolidone. Control MeasuresThe cholera outbreak in Juba ended in June 2007. At the time of the investigation, MOH established a working group with key stakeholders (the United Nations Children's Fund, the United Nations Office for Humanitarian Affairs, and WHO) and other international nongovernmental organizations to develop a strategy for cholera prevention and preparedness for Southern Sudan. The following strategies were implemented for the 2007 outbreak and any future outbreaks: 1) community health education, with emphasis on improved hygiene practices and sanitation; 2) establishment of food safety regulations for the local market; 3) expansion of the municipal water supply; 4) establishment of proper city waste disposal systems and house pit latrines; 5) banning of defecation in the three main streams in Juba; 6) a shift from informal to formal planned settlements for houses; and 7) supervision of water treatment with chlorine at collection points along the Nile River. Reported by: L Kur, MS, C Mounir, MD, J Lagu, MD, M Muita, MD, Southern Sudan Field Epidemiology and Laboratory Training Program; J Rumunu, MD, Ministry of Health, Government of Southern Sudan. B Ochieng, Kenya Medical Research Institute, Nairobi, Kenya. A Weathers, MPP, P Nsubuga, MD, E Maes, PhD, Div of Global Public Health Capacity Development, Coordinating Office for Global Health; I Rolle, PhD, EIS Officer, CDC. Editorial Note:Cholera outbreaks continue to occur throughout Africa, despite advances in cholera surveillance, treatment, and prevention. The main contributors to cholera outbreaks worldwide include a lack of clean water, inadequate sanitation, and suboptimal food-handling practices (5). Cholera is a major public health concern because it induces acute severe diarrhea and can result in death if oral rehydration is not administered quickly (1). Once a cholera outbreak occurs, simple interventions can prevent infection: 1) washing hands with soap before eating, cooking, and after defecation; 2) eating cooked food served hot; and 3) drinking water treated by a recommended method (e.g., boiling, chlorination, or solar disinfection through UV+ heat) (5). This investigation of cholera in Juba did not implicate a single source of water or food, which are common modes of cholera transmission. The unadjusted matched analysis indicated that the following were risk factors for cholera: 1) using a water source close to the place of residence (i.e., <20 meters); 2) being a visitor to Juba; and 3) living less than 1 year in Juba. Persons consuming a meal with hot meat or hot fish were less likely to have cholera. Surprisingly, persons who did not treat their water also appeared to have a lower risk for cholera. Persons using untreated water might have been previously exposed to cholera and therefore might have developed some immunity. Moreover, among persons with cholera who treated their water, poor techniques for treating water with chlorine might have resulted in exposure to cholera. This is especially likely if those persons who used chlorine were more likely to have used visibly turbid water from the Nile River that was imperfectly disinfected by chlorine. Despite these findings, the majority of the associations observed became insignificant in the multivariable analysis, which indicated that the initial results were artifacts or were attributed to limitations of the study. Only eating a hot meal containing meat in the 3 days before becoming ill (case-patients) or being interviewed (controls) remained significantly protective (p = 0.03) in the multivariable analysis when all the significant variables from the bivariate analysis were included. Knowledge of proper food handling and the importance of heating foods thoroughly before eating might have helped prevent the transmission of cholera in this population, as suggested by the lower odds of cholera by those persons eating at least one hot meal with meat. Cholera can grow in food kept at room temperature (5). Food was routinely cooked outside using makeshift stoves, and cold storage of food was limited because of a lack of electricity. Previous studies of cholera outbreaks have implicated the consumption of cold foods (e.g., seafood and raw vegetables) as risk factors for cholera and recommended that food be cooked and eaten hot (6,7). Treatment of the case-patients consisted of the recommended WHO treatment of rehydration using oral rehydration and intravenous therapy. Approximately half of the case-patients received antibiotics, which WHO indicates should only be administered in severe cases (5). Only 14 case-patients were classified as having severe dehydration. The findings in this report are subject to at least three limitations. First, the data collected in the case-control study (e.g., information related to the main source of drinking water and water treatment supplies) were self-reported. In addition, widespread exposure to health messages might have increased reports of risk-reducing behavior because of social desirability bias. The investigation team arrived after the outbreak had peaked, and the health messages had been in operation for at least 1 month before the team's arrival. Second, misclassification bias might have occurred because some of the controls might have developed immunity to cholera, and laboratory tests revealed that, of the 10 case-patients tested, only six were found to have cholera. Controls were not tested for cholera. As a result, some of the cases might not have been actual cases, and some of the controls might have been cases. Finally, the sample size for the case-control study was small and therefore might have limited significant associations for risk factors with p-values <0.05. In developing countries such as Southern Sudan or those recovering from war, returning residents might be at greater risk for diseases such as cholera. Cholera prevention strategies recommended by WHO and MSF that could be used for countries recovering from war include 1) encouraging proper food-handling techniques, including eating heated food; 2) intensifying surveillance to detect cases early; 3) building proper pit latrines; 4) cleaning defecation fields; 5) providing soap and chlorine free of charge or at a reduced cost; and 6) implementing appropriate water and sanitation policies (5,8). Acknowledgments This report is based, in part, on contributions by A Taban, O Jackson, E Kosti, J Benjamin, L Okeny, C Olur, B Samuel, Ministry of Health, Government of Southern Sudan; S Dada, World Health Organization, Juba Office, Southern Sudan; and E Mintz, MD, Div of Bacterial, Foodborne, and Mycotic Diseases, National Center for Zoonotic, Vector-Borne, and Enteric Diseases, and T Handzel, PhD, Div of Emergency and Environmental Health Svcs, National Center for Environmental Health, CDC. References
Table 1 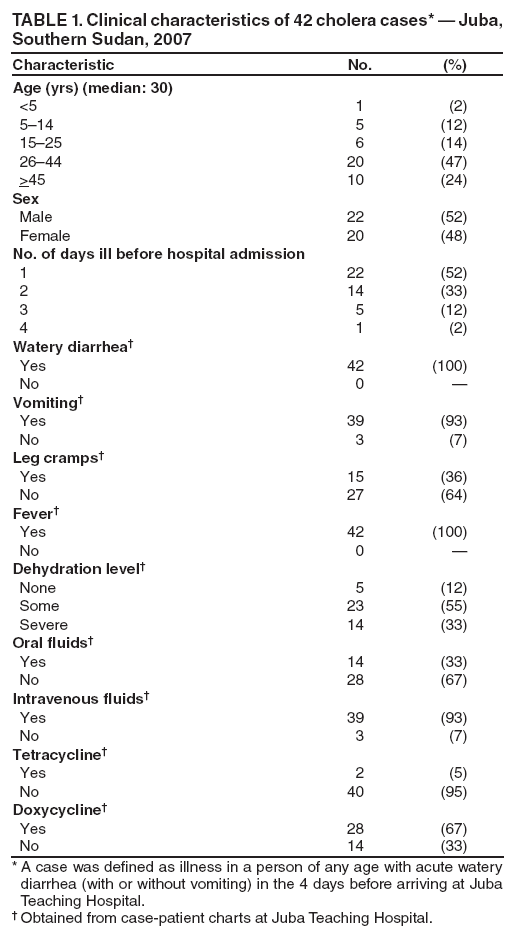 Return to top. Table 2 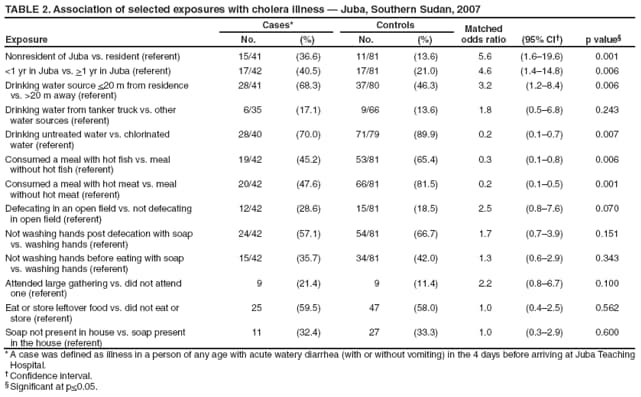 Return to top. Figure 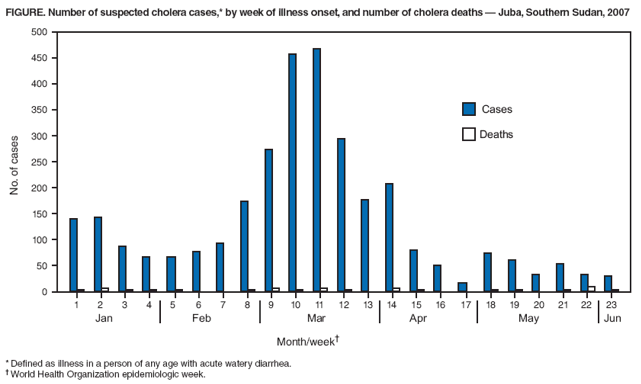 Return to top.
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 4/8/2009 |
|||||||||
|