 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Cigarette Smoking Among Adults --- United States, 2007Please note: An erratum has been published for this article. To view the erratum, please click here. One of the national health objectives for 2010 is to reduce the prevalence of cigarette smoking among adults to <12% (objective 27.1a) (1). To assess progress toward this objective, each year CDC analyzes self-reported data from the National Health Interview Survey (NHIS). This report summarizes findings for 2007, which indicated that approximately 19.8% of adults were current smokers in 2007, a decrease of 1.0 percentage point from 2006 (20.8%) (2). Cigarette smoking has declined during the past 40 years among all sociodemographic subpopulations of adults; however, the declines during the past decade have been smaller than in previous decades. The proportion of current everyday smokers who made a quit attempt during the preceding year decreased 7.2 percentage points from 1993 (47.0%) to 2007 (39.8%). During 1993--2007, young adults (aged 18--24 years) consistently had the highest prevalence of quitting for >1 day during the preceding year (59.3% in 1993 and 53.1% in 2007). Prevention of initiation and smoking cessation at all ages is beneficial in reducing morbidity and mortality. Clinicians should strongly advise smokers to quit and recommend they use effective cessation treatments (3). Health insurers, health insurance purchasers, and health systems should assist clinicians in making effective treatments available by including counseling and medications for smoking cessation as covered benefits and should support effective community interventions for cessation, including increased excise taxes, mass media campaigns, and smoke-free laws (3,4). The 2007 NHIS adult core questionnaire, which contained questions on cigarette smoking and cessation attempts, was administered by in-person interview to a nationally representative sample of the noninstitutionalized, U.S. civilian population aged >18 years (N = 23,393). One adult per selected household was chosen randomly to participate in the survey. NHIS oversampled for blacks, Hispanics, and Asians aged >65 years, who were selected at twice the probability of other adults in the household.* The total household response rate was 87.1%, and the overall survey response rate for the sample adult component of the survey was 67.8%. Smoking status was classified based on the respondent's answers to the following questions: "Have you smoked at least 100 cigarettes in your entire life?" and "Do you now smoke cigarettes every day, some days, or not at all?" Current smokers reported they had smoked 100 cigarettes or more during their lifetime and currently smoke every day or some days. Former smokers reported smoking at least 100 cigarettes during their lifetime and currently do not smoke. The prevalence of one or more cessation attempts during the preceding year was assessed among current everyday smokers and included those who responded "yes" to the question, "During the past 12 months, have you stopped smoking for more than one day because you were trying to quit smoking?" Data were adjusted for nonresponse and weighted to provide national estimates of cigarette smoking prevalence and quit attempts; 95% confidence intervals were calculated using statistical software to account for the multistage probability sample design. For all comparisons, statistical significance was determined using a two-sided z test; differences were considered statistically significant at p<0.05. In 2007, an estimated 19.8% (43.4 million) of U.S. adults were current cigarette smokers; of these, 77.8% (33.8 million) smoked every day, and 22.2% (9.6 million) smoked some days. In 2007, 39.8% (13.4 million) of adult current everyday smokers had stopped smoking for >1 day during the preceding 12 months because they were trying to quit. Among the estimated 86.8 million adults who had smoked at least 100 cigarettes in their lifetime (defined as ever smokers), 52.1% (47.3 million) were no longer smoking at the time of the interview. Smoking prevalence was higher among men (22.3%) than women (17.4%) (p<0.01) (Table). Among the different racial/ethnic populations, Asians (9.6%) had the lowest smoking prevalence, whereas American Indians/Alaska Natives (36.4%) had significantly higher prevalence than the other racial/ethnic populations (p<0.05 for all comparisons). Smoking prevalence among whites (21.4%) and blacks (19.8%) was significantly higher than among Hispanics (13.3%) (p<0.01 for both comparisons). Smoking prevalence also varied by education level among adults aged >25 years. Adults who had a General Education Development (GED) diploma (44.0%) and those with 9--11 years of education (33.3%) had the highest prevalence of current smoking. Those who had an undergraduate or graduate degree had the lowest smoking prevalence (11.4% and 6.2%, respectively). By age group, the prevalence of smoking was lowest among those aged >65 years (8.3%), compared with those aged <65 years (persons aged 18--24 years [22.2%], aged 25--44 years [22.8%], and aged 45--64 years [21.0%]). Smoking among adults whose incomes were below the federal poverty level (28.8%) was significantly higher than those whose incomes were at or above this level (20.3%) (p<0.02).† The prevalence of cigarette smoking among adults was significantly lower in 2007 (19.8%) than in 2006 (20.8%) (p=0.05). Subgroups with significant decreases in smoking prevalence from 2006 to 2007 included blacks (from 23.0% in 2006 to 19.8% in 2007 [p=0.01]) and adults aged >65 years (from 10.2% in 2006 to 8.3% in 2007 [p=0.01]). From 1993 (the first year that quit attempt data were collected in NHIS with everyday smokers identified separately) to 2007, the prevalence of a quit attempt during the preceding 12 months among everyday smokers decreased (p<0.01); these decreases were significant among those aged 25--44 years (p<0.01) and >65 years (p=0.02) (Figure). In each year, the proportion of current everyday smokers who tried to quit during the preceding 12 months decreased with increasing age, and young adults aged 18--24 years were significantly more likely to have made a quit attempt than older adults (p<0.05 for all comparisons). In 2007, the proportion of current everyday smokers who tried to quit was 53.1% among persons aged 18--24 years, 39.9% among those aged 25--44 years, 38.1% among those aged 45--64 years, and 25.3% among those aged >65 years. Reported by: SL Thorne, MPH, A Malarcher, PhD, E Maurice, MSPH, R Caraballo, PhD, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:After 3 years during which prevalence in current cigarette smoking among adults remained virtually unchanged (20.9% in 2004, 20.9% in 2005, and 20.8% in 2006), the prevalence in 2007 (19.8%) was significantly lower than in 2006 (2). For 5 consecutive years, the prevalence of smoking among women remained below 20% (19.2% in 2003, 18.5% in 2004, 18.2% in 2005, 18.0% in 2006, and 17.4% in 2007); however, variability existed among the subgroups of women. Also, for 6 consecutive years, former smokers outnumbered current smokers. During the past 40 years, smoking prevalence has declined overall and among each sociodemographic subpopulation.§ However, large disparities in smoking prevalence continue to exist by race/ethnicity and education level. The continuing higher prevalence among several populations, such as American Indians/Alaska Natives (36.4%), persons with GED diplomas (44.0%), and persons reporting family incomes below the federal poverty level (28.8%), emphasizes the need for more effective policy and environmental and individual-level interventions to reach and assist these subpopulations. The trends in smoking prevalence from NHIS data showing a slow decrease from the 1990s through the early- and mid-2000s are similar to trends in other national surveys (e.g., the National Household Survey on Drug Use and Health and the Tobacco Control Supplement to the Current Population Survey¶). NHIS data on smoking prevalence is the primary measure used to assess progress in meeting the Healthy People 2010 objective of reducing smoking among adults to <12%, and these data indicate that the objective likely will not be met. Before 2007, several population subgroups had met the Healthy People 2010 smoking prevalence objective of <12% and, in 2007, these same subpopulations continued to meet this goal. Subpopulations who continued to meet this goal in 2007 include Hispanic (8.3%) and Asian (4.0%) women, women with 0--8 years of education (10.0%) or undergraduate (9.4%) or graduate degrees (6.0%), and women aged >65 years (7.6%). Men with graduate degrees (6.4%) and men aged >65 years (9.3%) also met this goal. The percentage of everyday smokers who attempted to quit for >1 day during the preceding 12 months decreased during 1993--2007. The lack of funding for comprehensive state tobacco-control programs likely has remained a barrier to achieving progress in increasing smokers' quit attempts. In fiscal year 2005, investments by states in tobacco control varied; the mean per capita expenditure was $2.76, with some states investing approximately $11.00, whereas others invested nothing (4). CDC recommends a per capita annual expenditure of $9.23 to $18.03 by state comprehensive tobacco-control programs to implement effective programs (5). The majority of smokers who attempt to quit do not use recommended cessation methods (3), and most of these untreated smokers relapse within the first 8 days after quitting; an estimated 24%--51% are abstinent at 1 week, 15%--28% are abstinent at 1 month, and 10%--20% are abstinent at 3 months (6). Of untreated adult smokers who try to quit smoking each year, only 4%--7% are likely to be successful (3). Among daily smokers, younger adults (aged 18--24 years) were more likely to try to quit smoking during the preceding year than older adults. This finding is consistent with other national studies (7). Young adults have lower levels of addiction, are less likely to be heavy smokers, and are more likely to have smoke-free homes than older adults; lower levels of dependence and having a smoke-free home are associated with increases in trying to quit during the preceding year (7). Smoking cessation is beneficial at any age; however, quitting at younger ages is associated with greater decreases in premature mortality (8). The findings in this report are subject to at least three limitations. First, estimates of cigarette smoking were based on self-report and were not validated with biochemical tests. However, self-reported smoking status has validity when compared with measured serum cotinine levels and yields similar population prevalence estimates (9). Second, the NHIS questionnaire is administered in English and Spanish only, which might affect estimates for racial/ethnic populations who do not speak English or Spanish primarily. Finally, single-year estimates with large confidence intervals for certain population groups (e.g., American Indians/Alaska Natives) primarily resulted from small sample sizes. Tobacco use screening with a brief cessation intervention is one of the top three clinical preventive services that have been found to be cost-saving (10). Effective clinical cessation interventions include brief interventions by clinicians; individual, group, or telephone counseling; and the following pharmacologic therapies: Bupropion SR, Varenicline, and nicotine gum, inhaler, lozenge, nasal spray, or patch (3). Clinicians and health-care delivery systems need to consistently identify and document tobacco use status, treat every tobacco user seen in the health-care setting, and promote patients' use of quitlines (available countrywide through the toll-free access number 1-800 QUIT- NOW) (3). These effective clinical approaches should be part of a comprehensive tobacco-control program that includes increasing the real price of tobacco products, implementing smoke-free policies, and increasing health insurance coverage for effective cessation interventions; with wider implementation of these policies and programs, greater progress in reducing smoking prevalence among adults could be attained (4,5). References
* For this report, persons identified as white, black, Asian, and American Indian/Alaska Native are all non-Hispanic. Persons identified as Hispanic might be of any race. † 2007 estimates are based on family income reported by respondents and 2006 poverty thresholds (published by the U.S. Census Bureau). § Additional information available at http://www.cdc.gov/tobacco/data_statistics/tables/adult/table_2.htm. ¶ Available at http://www.oas.samhsa.gov/nsduhlatest.htm and http://riskfactor.cancer.gov/studies/tus-cps, respectively.
Table 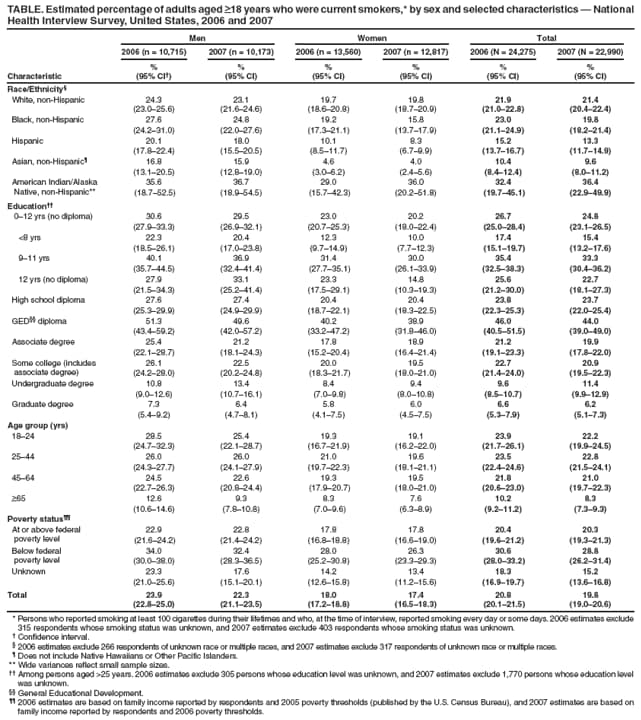 Return to top. Figure 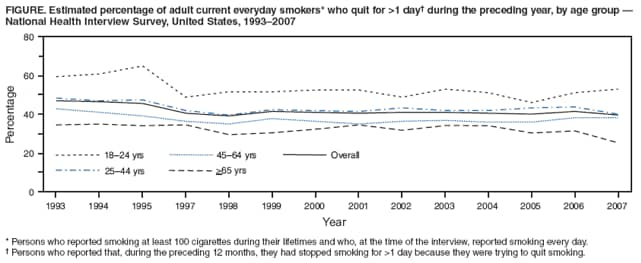 Return to top.
All MMWR HTML versions of articles are electronic conversions from typeset documents. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (http://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 11/13/2008 |
|||||||||
|