 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Salmonella Serotype Enteritidis Infections Among Workers Producing Poultry Vaccine --- Maine, November--December 2006On November 15, 2006, the Maine Department of Health and Human Services (MDHHS) was notified of a case of salmonellosis (a nationally notifiable disease) in an employee of a facility that produced poultry vaccine. When a second case of salmonellosis in another employee at the same facility was reported on November 25, MDHHS began an outbreak investigation. Results of that investigation suggested that 21 employees of the facility became ill during a 1-month period from exposure to a strain of Salmonella serotype Enteritidis (SE) that was used in vaccine production. Infection was thought to have resulted from environmental contamination after the spill of a liquid containing a high concentration of SE. As a result, MDHHS recommended that the facility improve its infection-control procedures to better protect workers. This outbreak highlights occupational risks that can be associated with the manufacture of veterinary biologics involving human pathogens. The vaccine-production facility is located in a town of approximately 8,000 persons in central Maine, has 74 employees, and manufactures viral and bacterial vaccines for poultry. The facility had been last inspected in August 2005 by staff members of the U.S. Department of Agriculture's (USDA's) Center for Veterinary Biologics, which regulates animal vaccine-production facilities. The facility maintains stock cultures of four phage types of SE (8, 14B, 23, and 24) for vaccine production. On November 9, 2006, a spill of approximately 1--1.5 liters of liquid occurred in the fermentation room of the production area of the facility; the liquid contained 2 x 1010 to 5 x 1010 colony forming units per milliliter of SE phage type 8. The room was unoccupied at the time the spill occurred. The one worker who was regularly assigned to this room reported finding liquid overflowing onto the floor from the fermentation apparatus when he entered the room, wearing personal protective equipment (PPE) (e.g., biohazard suit, hat, booties, mask, and gloves). He cleaned up the spill using a mop, a 5% bleach solution, and a commercial disinfectant effective against SE. The mop was autoclaved before disposal in a room 30 feet away (room A) used for cleaning and sterilizing laboratory supplies and equipment for vaccine production. The facility did not have a written spill procedure or a spill clean-up kit. On November 15, the worker who cleaned up the spill had diarrhea of 1 day's duration. He did not miss work, seek medical care, or submit a stool specimen for culture. On December 13, a total of 67 (91%) of the 74 employees were interviewed at the facility by MDHHS staff members using a standard questionnaire. A case of diarrheal illness was defined as three or more loose or watery stools in a 24-hour period since November 1. Twenty-one (31%) of the 67 employees interviewed had illness that was consistent with the case definition, with onset ranging from November 8 to December 11 (Figure). The employee with the earliest date of onset of illness was unable to recall the exact day she became ill. When interviewed on November 29, she reported becoming ill approximately 3 weeks earlier; therefore, her illness onset date was recorded as November 8. In addition to diarrhea, patients reported fatigue (86%), cramps (86%), body aches (71%), nausea (62%), headache (57%), chills (57%), fever (43%), vomiting (43%), and blood in stool (29%); none of the employees were hospitalized. No secondary cases in family members were identified. Five of eight stool specimens from eight patients submitted for culture were positive for SE. Among 33 workers in the production area, 18 (55%) had illness consistent with the case definition, compared with three (9%) of 34 workers in other areas of the facility (relative risk: 6.2; 95% confidence interval = 2.0--19.0). When analysis was restricted to workers in the production area, the strongest association with illness was working in room A. Eighteen (69%) of 26 employees who worked in room A (including those who did so intermittently) became ill, compared with none of the seven production-area workers who did not work in room A (p=0.002). During multiple visits to the facility, investigators noted inadequate handwashing and lack of PPE. Aside from working in room A, none of the exposures examined were significantly associated with illness. On November 30, staff members collected 15 environmental swab specimens from the production area; the swabs were processed by a commercial laboratory used by the vaccine manufacturer. Nineteen additional environmental swabs from room A were collected and processed by MDHHS on December 19. All environmental swabs were negative for Salmonella. Six drinking water samples from three sites in the facility were collected on November 30 and processed by MDHHS; all were tested for Escherichia coli as a marker for bacterial contamination. All the samples were negative for E. coli. Testing of water samples for E. coli and fecal coliform also was conducted by the manufacturer; the results were negative. Isolates of SE from four patients and the four vaccine stock cultures from the facility underwent pulsed field gel electrophoresis (PFGE) testing with two enzymes (XbaI and BlnI) by MDHHS and were determined to be indistinguishable. Phage typing was then performed on the SE isolates by the National Microbiology Laboratory of Canada in collaboration with CDC. Isolates from all four patients were phage type 8, matching the phage type of the spilled stock culture. PFGE and phage typing also were performed on all seven SE isolates from ill Maine residents with no connection to the vaccine-production facility that were submitted to MDHHS during October--November 2006. The isolates were from four of Maine's 16 counties; none were from the county where the vaccine facility was located. All seven isolates were indistinguishable from the phage type 8 isolates by PFGE testing on the first enzyme (XbaI); five of the seven isolates were tested on the second enzyme (BlnI), and all five matched the phage type 8 isolates. However, when phage typed, all seven isolates were determined to be phage type 13A. Reported by: D Guppy, A Yartel, MPH, Maine Dept of Health and Human Svcs. A Pelletier, MD, Career Epidemiology Field Officer, CDC. Editorial Note:Salmonella infections usually are acquired by eating contaminated food; however, some outbreaks have been associated with environmental contamination (1,2). Salmonella can survive in the environment for months (3), and the incubation period is 6--72 hours (4). Although the exact mechanism for infection of workers in this outbreak remains unknown, environmental contamination of room A likely was the source of SE infection. Workers might have become infected through hand-to-mouth activities after touching contaminated surfaces in room A. This mode of transmission is plausible because 1) the materials used in the clean-up of the spill were processed in room A before disposal, 2) the phage type of SE among four ill employees (type 8) was the same as that of the stock culture involved in the spill and different from that of the seven isolates from other SE cases (type 13A) reported in Maine during the same approximate period, 3) a strong epidemiologic association was determined between illness and working in room A, and 4) inadequate handwashing practices and lack of PPE were noted in room A. Person-to-person transmission also might have occurred because some persons continued to work at the facility while ill. The findings in this report are subject to at least three limitations. First, staff members at the vaccine-production facility did not document details of the spill that occurred on November 9 until 20 days later, which might have introduced recall bias. Second, environmental specimens were not obtained until 3 weeks after the spill had occurred; routine cleaning and disinfecting had occurred during this interval. Finally, because of the clonal nature of SE, PFGE testing and phage typing alone might not be able to provide definitive strain discrimination; additional typing methods might be required (5). MDHHS recommended that the facility improve hand-washing practices among employees and, especially in room A, the use of PPE, including gloves and (where splashes might occur) gowns and face shields. MDHHS further recommended creation of procedures for handling spills and routinely disinfecting work areas and advised ill employees not to work until their symptoms resolved. Results of the investigation were shared with USDA, the Maine Department of Labor, and the Occupational Safety and Health Administration. USDA reinspected the facility in January 2007 and began a follow-up visit on August 28. Acknowledgments This report is based, in part, on contributions by R Ahmed, MSc, Canadian Science Centre for Human and Animal Health; R Danforth, L Deyrup, PhD, K Phillips, MPH, J Randolph, H Swanson, D Wrigley, Maine Dept of Health and Human Svcs, D Siulinski, Maine Dept of Labor. References
Figure 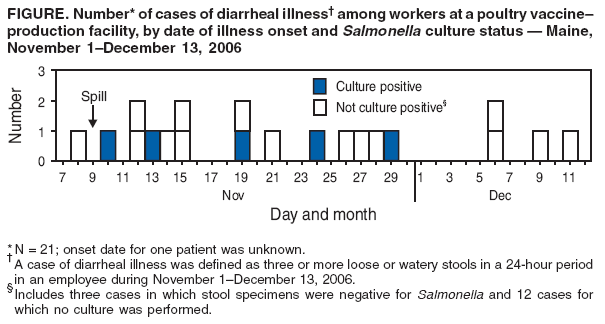 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 8/29/2007 |
|||||||||
|