 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Use of Cessation Methods Among Smokers Aged 16--24 Years --- United States, 2003Smoking cessation among adolescent smokers is relatively rare, with approximately 15.6% of smokers aged 12--19 years quitting smoking in a 4-year period (approximately 4% per year) (1). Rates for failed quitting attempts among younger smokers are higher than those for adults (43%) (2), with approximately 58% of high-school smokers having tried to quit at least once for 1 day or longer in the preceding year (3). To track the history of quitting behavior among smokers aged 16--24 years, Roswell Park Cancer Institute (Buffalo, New York) initiated the 2-year longitudinal National Youth Smoking Cessation Survey (NYSCS)* in 2003. This report summarizes key findings from the survey regarding lifetime use of smoking-cessation methods. The findings indicated that smokers aged 16--24 years who had tried to quit were more likely to use unassisted quitting methods than assisted quitting methods; none of the unassisted methods are recommended by the Public Health Service (PHS) clinical guidelines for treatment of tobacco use and dependence, whereas most of the assisted methods are recommended for adults and have been determined to be effective. Many youths aged 16--24 years are trying to quit smoking but often underestimate the rapid progression to tobacco dependence; therefore, PHS clinical practice guidelines for treating tobacco use and dependence recommend that certain clinical interventions proven to be effective among adults be used in youth-based approaches to cessation (4). In addition, other components of comprehensive tobacco-control programs also increase smoking cessation and should be implemented at CDC-recommended levels (5) to lower tobacco use among youths and adults. The 2003 NYSCS collected information on tobacco use and quitting practices through a random-digit--dialed, computer-assisted telephone interview survey of young smokers conducted by Westat (Rockville, Maryland) during June--November 2003. Persons aged 16--24 years who had smoked at least 20 cigarettes in their lifetimes and who had smoked at least once during the preceding 30 days were interviewed from randomly selected U.S. households with telephones. A total of 2,582 respondents completed the initial interview (69.6% response rate for all age-eligible smokers).† Smokers who had ever tried to quit were asked about their knowledge of, the perceived availability of, and use of assisted and unassisted quitting methods. Assisted methods include medications or obtaining assistance from a person, class, telephone counselor, or website. Respondents who were knowledgeable about a specific assisted method and perceived that the method was available were then asked whether they had ever used that method. Respondents who had ever tried to quit also were asked about their use of unassisted methods to quit smoking, including using self-help strategies and educational methods, such as pamphlets/videos, exercising, and changing smoking-related behaviors (e.g., decreasing the number of cigarettes smoked or not buying cigarettes). Data were weighted to represent the population of U.S. smokers aged 16--24 years, according to the 2001--2002 Tobacco Use Supplement to the Current Population Survey. To ensure that respondents being analyzed were established smokers and had attempted to quit, only those who had smoked at least 100 cigarettes during their lifetimes and who had tried to quit smoking at least once were included in the analyses (1,827 respondents). Use of methods to quit also was examined by sex. Of the 13 assisted methods (Table 1), only one (talking with a nurse, doctor, or dentist) was used by at least 20% of this age group, whereas six of the 11 unassisted (i.e., not recommended by PHS guidelines) methods were each used by at least 36% of respondents (Table 2). The most commonly used unassisted strategy (decreasing the number of cigarettes smoked) was tried by 88.3% of young smokers. The remaining five frequently used unassisted strategies were not buying cigarettes (56.0%), exercising more (51.0%), trying to quit with a friend (47.5%), telling others they no longer smoked (44.5%), and switching to light cigarettes (36.1%). Females (24.9%) were more likely than males (15.6%) to seek help from health professionals but less likely to have tried nicotine gum (14.4% versus 20.3%) (Table 1). Females (52.1%) also were more likely than males (43.2%) to try to quit with a friend and to have used self-help pamphlets or videos (19.5% versus 12.5%). However, males (55.7%) were more likely than females (46.0%) to exercise more as a strategy to quit and to switch to chewing tobacco, snuff, or other tobacco products (18.0% versus 1.6%) (Table 2). Reported by: DC Barker, MHS, Barker Bi-Coastal Health Consultants, Calabasas, California. GA Giovino, PhD, Roswell Park Cancer Institute and SUNY Buffalo School of Public Health and Health Professions, Buffalo, New York. J Gable, MS, Research Triangle Institute, Atlanta, Georgia. C Tworek, PhD, Center for Public Health Improvement and Innovation, Pacific Institute for Research and Evaluation, Calverton, Maryland. CT Orleans, PhD, Robert Wood Johnson Foundation, Princeton, New Jersey. A Malarcher, PhD, Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The NYSCS results indicate that smokers aged 16--24 years rely more on unassisted methods to try to quit than assisted methods recommended for adults by PHS clinical guidelines (4). The following six cessation methods are recommended by PHS for adults: 1) talk with a health professional, 2) use nicotine-replacement products, 3) use bupropion, 4) talk with a counselor, 5) attend a program or class, and 6) call a telephone helpline. Among NYSCS respondents, only 20.1% who had ever tried to quit had ever spoken with a health-care professional about quitting, the most commonly used assisted method. Among adult smokers who had been to a health-care professional and tried to quit during a given year, 61.8% were advised to quit using tobacco products (6). Female respondents also were more likely than male respondents (24.9% versus 15.6%) to have talked with a health-care professional; this finding might be directly related to a difference in the number of visits typically made by young males and females to health-care professionals, a difference that has been reported for adults (7). Use of certain unassisted strategies such as switching to light cigarettes or switching to chewing tobacco, snuff, or other tobacco products was common. The high proportion of respondents who tried to quit smoking by switching to light cigarettes (36.1% overall) or other tobacco products (18.0% among males) is a concern because such strategies might undermine successful cessation (8). The findings in this report are subject to at least two limitations. First, these nationally representative estimates apply only to smokers aged 16--24 years living in households with telephones. Second, respondents were asked to identify themselves as smokers or nonsmokers and did not submit to any biochemical validation; some smokers might not have identified themselves as such. During the initial questions of the interview, respondents were unaware that participation in the survey was limited to smokers. Because of the lack of sufficient evidence regarding the effectiveness of interventions for smokers aged 16--24 years, persons such as public health practitioners and health-care providers who work with smokers in this age range should consult CDC's Youth Tobacco Cessation: A Guide for Making Informed Decisions, which summarizes what is known about tobacco-cessation interventions for youth and the role of these interventions in comprehensive tobacco-control programs (9). Clinical interventions that apply cognitive-behavioral approaches to behavior change seem the most promising (10). Additional research is needed to find effective clinical cessation interventions to help young persons stop smoking. For smokers aged <18 years, effective behavioral counseling approaches are essential because the Food and Drug Administration has not approved the use of any pharmacotherapy (e.g., nicotine-replacement products or bupropion) for smoking cessation in this age group. As these potential interventions are being researched and developed, comprehensive tobacco-control programs, which also include nonclinical interventions such as increasing excise taxes, promoting smoke-free air policies, conducting media campaigns with other community-based interventions, providing insurance coverage for proven treatments, and establishing telephone helplines, should be fully implemented in every state and territory to prevent youths from starting to smoke and to help youths and adults stop smoking (5). References
* Funded by the Robert Wood Johnson Foundation, with additional analytical support provided by the National Cancer Institute and CDC. † Of 85,000 households in the sample, 60.0% responded, and 21.4% of the responding households had one or more persons aged 16--24 years. Respondents were given a reward for participation worth $20 (either a check, restaurant coupons, or a store gift certificate). Table 1 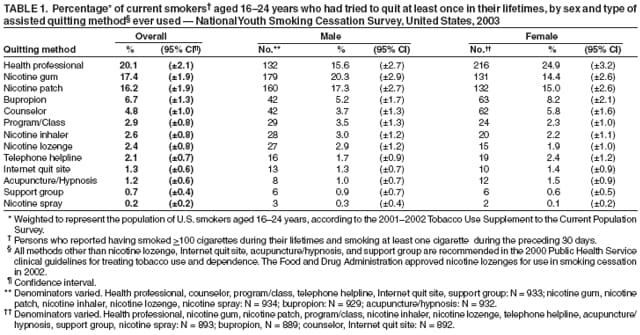 Return to top. Table 2 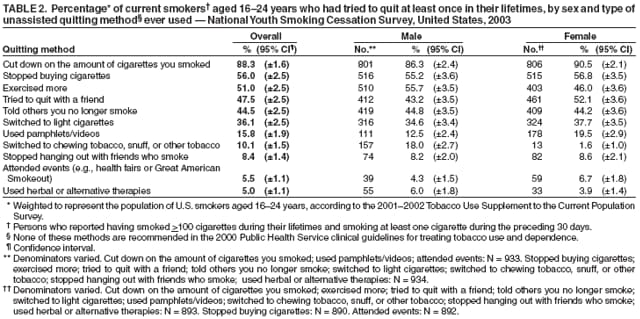 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 12/20/2006 |
|||||||||
|