 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Heat-Related Deaths --- United States, 1999--2003Heat-related illnesses (e.g., heat cramps, heat exhaustion, heat syncope, or heatstroke) can occur when high ambient temperatures overcome the body's natural ability to dissipate heat (1). Older adults, young children, and persons with chronic medical conditions are particularly susceptible to these illnesses and are at high risk for heat-related mortality (2). Previous analyses of the risk factors associated with heat-related deaths* have been based on the underlying cause† entered on the death certificate (4,5) and have not included decedents for whom hyperthermia was listed as a contributing factor but not the underlying cause of death. This report describes an analysis in which number of heat-related deaths were counted, including deaths in which hyperthermia was listed as a contributing factor on the death certificate. The analysis revealed that including these deaths increased the number of heat-related deaths by 54% and suggested that the number of heat-related deaths is underestimated. CDC uses information from death certificates categorized by codes from the International Classification of Diseases to estimate national mortality trends. These data, collected and submitted by states, were used to determine the number of deaths in the United States during 1999--2003 that had exposure to excessive natural heat§ recorded as the underlying cause (code X30 from ICD, tenth revision [ICD-10]), hyperthermia¶ recorded as a contributing factor (ICD-10 code T67) (6), or both. During 1999--2003, a total of 3,442 deaths resulting from exposure to extreme heat were reported (annual mean: 688). For 2,239 (65%) of these deaths, the underlying cause of death was recorded as exposure to excessive heat; for the remaining 1,203 (35%), hyperthermia was recorded as a contributing factor. Deaths among males accounted for 66% of deaths and outnumbered deaths among females in all age groups (Figure). Of the 3,401 decedents for whom age information was available, 228 (7%) were aged <15 years, 1,810 (53%) were aged 15--64 years, and 1,363 (40%) were aged >65 years. The state with the highest average annual hyperthermia-related death rate during 1999--2003 was Arizona (1.7 deaths per 100,000 population), followed by Nevada (0.8) and Missouri (0.6). Cardiovascular disease was recorded as the underlying cause of death in 681 (57%) of cases in which hyperthermia was a contributing factor (Table). Approximately 70% of these heat-related cardiovascular deaths occurred among persons with reported chronic ischemic heart disease. External causes (e.g., unintentional poisonings) were documented as the underlying cause of 345 (29%) deaths in which hyperthermia was a contributing factor. Endocrine, nutritional, and metabolic disorders (e.g., diabetes mellitus) were the underlying causes in 38 (3%) of total deaths. All other underlying causes, including infection and psychiatric disorders, accounted for 139 (11%) deaths. Reported by: GE Luber, PhD, CA Sanchez, MD, Div of Environmental Hazards and Health Effects, National Center for Environmental Health/Agency for Toxic Substances and Disease Registry (proposed); LM Conklin, MD, EIS Officer, CDC. Editorial Note:In this analysis, the inclusion of hyperthermia as a contributing cause of death increased by 54% the total number of heat-related deaths during 1999--2003 that would have been counted through inclusion of a heat-related underlying cause alone. Because heat-related illnesses can exacerbate existing medical conditions and death from heat exposure can be preceded by various symptoms, heat-related deaths can be difficult to identify when illness onset or death is not witnessed by a clinician. In addition, the criteria used to determine heat-related causes of death vary among states. This can lead to underreporting heat-related deaths or to reporting heat as a factor contributing to death rather than the underlying cause (3). The demographics (e.g., sex, age group, and state) of the decedents described in this report are consistent with previous descriptions of persons at risk for heat-related deaths (4,5). This analysis also provides additional information on the underlying causes of death in which hyperthermia was a contributing factor. Although this report might still underestimate the extent of overall heat-related morbidity and mortality, the inclusion of hyperthermia as a contributing factor to death provides a more comprehensive view of the actual effects of heat-related illnesses. The association between cardiovascular disease and heat-related death is well established (7); this analysis suggests the need for additional investigations of the association between noncardiovascular conditions, such as endocrine and respiratory diseases, and the risk for heat-related death. Continued exposure to excessive heat can lead to hyperthermia or death. Of the heat-related illnesses, heat exhaustion and heatstroke are the most serious. Heat exhaustion is characterized by muscle cramps, fatigue, headache, nausea or vomiting, and dizziness or fainting. The skin is often cool and moist, indicating that the body's mechanism for cooling itself (i.e., sweating) is still functioning. The pulse rate is typically fast and weak, and breathing is rapid and shallow. If untreated, heat exhaustion can progress to heatstroke (1). Heatstroke is a serious, life-threatening condition characterized by a high body temperature (>103ºF [>39.4ºC]); red, hot, and dry skin (no sweating); rapid, strong pulse; throbbing headache; dizziness; nausea; confusion; and unconsciousness. Symptoms can progress to encephalopathy, liver and kidney failure, coagulopathy, and multiple organ system dysfunction (2). Prompt treatment of heat-related illnesses with aggressive fluid replacement and cooling of core body temperature is critical to reducing morbidity and mortality (2). Many heat-related deaths, regardless of whether they are associated with chronic medical conditions, are preventable. During periods of extreme heat, heat-related illnesses can be prevented by avoiding strenuous outdoor activities, drinking adequate amounts of fluid, avoiding alcohol consumption, wearing lightweight clothing, and using air-conditioning. Groups at high risk include young children, persons aged >65 years, persons who do strenuous activities outdoors, and persons with chronic (particularly cardiovascular) medical conditions (8). During heat waves, young children, older adults, and chronically ill persons should be checked frequently by relatives, neighbors, and caretakers to evaluate their heat exposure, recognize symptoms of heat-related illness, and take appropriate preventive action. Regardless of the outdoor temperature, parents and other child-care providers should never leave children alone in cars and should ensure that children cannot lock themselves inside enclosed spaces, such as the trunks of automobiles. Communities can prepare for heat-related illnesses by creating well-defined heat response plans (HRPs) (9). Both governmental and nongovernmental organizations, each with specific roles and responsibilities, can be involved in this planning. HRP protocols and communication tools should be reviewed annually, before the summer months begin. The HRPs should identify populations at high risk for heat-related illness and death and determine which strategies will be used to reach them during heat emergencies. The HRP should also include specific criteria for activation and deactivation of the plan. Postemergency evaluations of HRPs are necessary to make appropriate revisions and improve plan effectiveness. References
* Defined as a death in which exposure to high ambient temperatures either caused the death or contributed to it substantially, the decedent had a body temperature at the time of collapse >105ºF (>40.6ºC), the decedent had a history of exposure to high ambient temperature, and other causes of hyperthermia could reasonably be excluded (3). † The underlying cause of death is defined as the disease or injury that initiated the chain of events that lead directly and inevitably to death. Contributing conditions, or factors, are defined as diseases, injuries, or complications that directly caused the death. A sample death certificate, showing underlying and contributing causes of death, is available at http://www.cdc.gov/nchs/data/dvs/death11-03final-acc.pdf. § Heat-related deaths can also be caused by exposure to excessive heat of man-made origin (e.g., from saunas or furnace malfunctions; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] code W92) and can include homicides and suicides involving exposure to excessive heat. Deaths from these causes were not included in this analysis. ¶ Abnormally high body temperature caused by the body's inability to dissipate heat.
Table 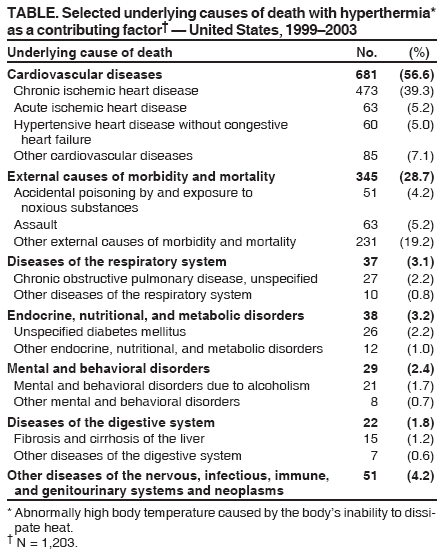 Return to top. Figure 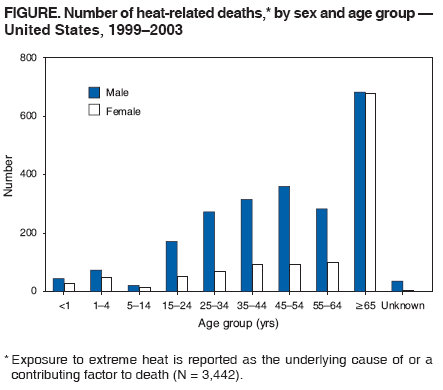 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 7/27/2006 |
|||||||||
|