 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Update: Influenza Activity --- United States, February 5--11, 2006During February 5--11, 2006,* the number of states reporting widespread influenza activity† increased to 13. Twenty-one states reported regional activity, 11 reported local activity, and five reported sporadic activity (Figure 1).§ The percentage of specimens testing positive for influenza increased in the United States overall. During the preceding 3 weeks (weeks 4--6), the largest number of isolates were reported from the South Atlantic and Mountain regions. During this time, the percentage of specimens testing positive for influenza ranged from 26.3% and 23.4% in the East North Central and South Atlantic regions, respectively, to 7.4% in the Pacific region. The percentage of outpatient visits for influenza-like illness (ILI)¶ increased during the week ending February 11 and remains above the national baseline.** The percentage of deaths attributed to pneumonia and influenza (P&I) was below the epidemic threshold for the week ending February 11. Laboratory SurveillanceDuring February 5--11, World Health Organization (WHO) collaborating laboratories and National Respiratory and Enteric Virus Surveillance System (NREVSS) laboratories in the United States reported testing 2,438 specimens for influenza viruses, of which 455 (18.7%) were positive. Of these, 136 were influenza A (H3N2) viruses, six were influenza A (H1N1) viruses, 280 were influenza A viruses that were not subtyped, and 33 were influenza B viruses. Since October 2, 2005, WHO and NREVSS laboratories have tested 66,129 specimens for influenza viruses, of which 5,216 (7.9%) were positive. Of these, 5,025 (96.3%) were influenza A viruses, and 191 (3.7%) were influenza B viruses. Of the 5,025 influenza A viruses, 2,378 (47.3%) have been subtyped; 2,351 (98.9%) were influenza A (H3N2) viruses, and 27 (1.1%) were influenza A (H1N1) viruses. P&I Mortality and ILI SurveillanceDuring the week ending February 11, P&I accounted for 7.0% of all deaths reported through the 122 Cities Mortality Reporting System. This percentage is below the epidemic threshold†† of 8.3% (Figure 2). The percentage of patient visits for ILI was 2.5%, which is above the national baseline of 2.2% (Figure 3). The percentage of patient visits for ILI ranged from 1.5% in the Pacific region to 4.7% in the West South Central region. Pediatric Deaths and HospitalizationsDuring October 2, 2005--February 11, 2006, CDC received reports of 14 influenza-associated deaths in U.S. residents aged <18 years. Twelve of the deaths occurred during the current influenza season, and two occurred during the 2004--05 influenza season. During October 1, 2005--February 4, 2006, the preliminary laboratory-confirmed influenza-associated hospitalization rate reported by the Emerging Infections Program§§ for children aged 0--17 years was 0.30 per 10,000. For children aged 0--4 years and 5--17 years, the rate was 0.78 per 10,000 and 0.04 per 10,000, respectively. During October 30, 2005--February 4, 2006, the preliminary laboratory-confirmed influenza-associated hospitalization rate for children aged 0--4 years in the New Vaccine Surveillance Network¶¶ was 0.33 per 10,000. Human Avian Influenza A (H5N1)No human avian influenza A (H5N1) virus infection has ever been identified in the United States. From December 2003 through February 20, 2006, a total of 170 laboratory-confirmed human avian influenza A (H5N1) infections were reported to WHO from Cambodia, China, Indonesia, Iraq, Thailand, Turkey, and Vietnam.*** Of these, 92 (54%) were fatal (Table). This represents an increase of one case and one death in Indonesia since February 13, 2006. The majority of infections appear to have been acquired from direct contact with infected poultry. No evidence of sustained human-to-human transmission of H5N1 has been detected, although rare instances of human-to-human transmission likely have occurred (1). * Provisional data reported as of February 17. Additional information about influenza activity is updated each Friday and is available from CDC at http://www.cdc.gov/flu. † Levels of activity are 1) widespread: outbreaks of influenza or increases in influenza-like illness (ILI) cases and recent laboratory-confirmed influenza in at least half the regions of a state; 2) regional: outbreaks of influenza or increases in ILI cases and recent laboratory-confirmed influenza in at least two but less than half the regions of a state; 3) local: outbreaks of influenza or increases in ILI cases and recent laboratory-confirmed influenza in a single region of a state; 4) sporadic: small numbers of laboratory-confirmed influenza cases or a single influenza outbreak reported but no increase in cases of ILI; and 5) no activity. § Widespread: Colorado, Connecticut, Florida, Georgia, Kansas, Maryland, New York, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, and Wyoming; regional: Alabama, Alaska, Arkansas, Delaware, Illinois, Indiana, Iowa, Kentucky, Louisiana, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Nebraska, North Carolina, Oklahoma, Oregon, Rhode Island, South Dakota, and Wisconsin; local: Arizona, California, Maine, Montana, Nevada, New Hampshire, New Jersey, New Mexico, North Dakota, Ohio, and Washington; sporadic: Hawaii, Idaho, Utah, Vermont, and West Virginia; no activity: none; no report: Missouri. ¶ Temperature of >100.0°F (>37.8°C) and cough and/or sore throat in the absence of a known cause other than influenza. ** The national baseline was calculated as the mean percentage of visits for ILI during noninfluenza weeks for the preceding three seasons, plus two standard deviations. Noninfluenza weeks are those in which <10% of laboratory specimens are positive for influenza. Wide variability in regional data precludes calculating region-specific baselines; therefore, applying the national baseline to regional data is inappropriate. †† The expected seasonal baseline proportion of P&I deaths reported by the 122 Cities Mortality Reporting System is projected using a robust regression procedure in which a periodic regression model is applied to the observed percentage of deaths from P&I that occurred during the preceding 5 years. The epidemic threshold is 1.645 standard deviations above the seasonal baseline. §§ The Emerging Infections Program (EIP) Influenza Project conducts surveillance in 60 counties associated with 12 metropolitan areas: San Francisco, California; Denver, Colorado; New Haven, Connecticut; Atlanta, Georgia; Baltimore, Maryland; Minneapolis/St. Paul, Minnesota; Albuquerque, New Mexico; Las Cruces, New Mexico; Albany, New York; Rochester, New York; Portland, Oregon; and Nashville, Tennessee. ¶¶ The New Vaccine Surveillance Network (NVSN) conducts surveillance in Monroe County, New York; Hamilton County, Ohio; and Davidson County, Tennessee. *** Available at http://www.who.int/csr/disease/avian_influenza/en. Reference
Figure 1 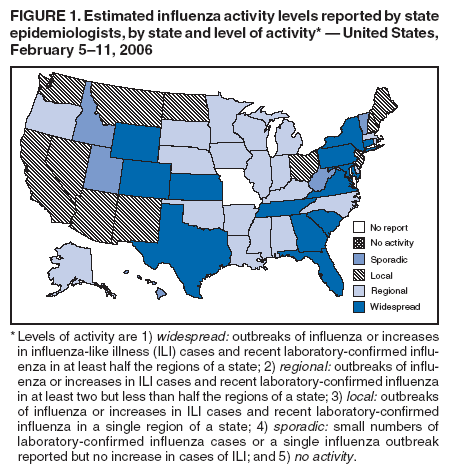 Return to top. Figure 2 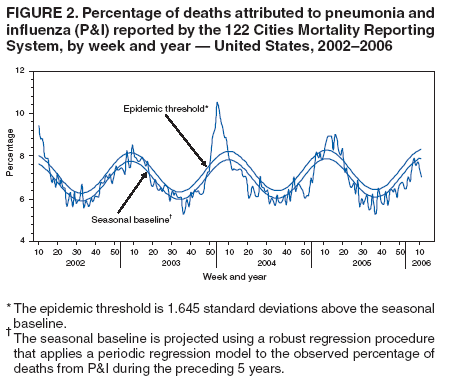 Return to top. Figure 3 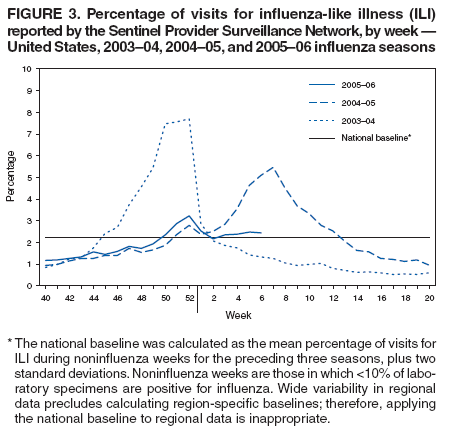 Return to top. Table 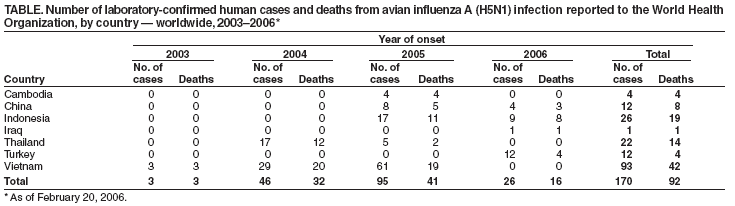 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 2/23/2006 |
|||||||||
|