 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Mobility Limitation Among Persons Aged >40 Years With and Without Diagnosed Diabetes and Lower Extremity Disease --- United States, 1999--2002Diabetes increases the risk for mobility limitation, especially among older persons (1,2). Lower extremity disease (LED), which includes peripheral arterial disease (PAD) and peripheral neuropathy (PN), also increases the risk for mobility limitation (3,4). To assess the prevalence of mobility limitation among persons with diagnosed diabetes, persons with LED, and persons with both or neither condition, CDC analyzed data from the National Health and Nutrition Examination Survey (NHANES) 1999--2002 for adults aged >40 years. This report summarizes the preliminary findings, which indicated that the national prevalence of mobility limitation is higher among persons with either diagnosed diabetes or LED than those without the conditions, and that adults with both conditions have a higher prevalence of mobility limitation than those with either condition alone. Monitoring the prevalence of diabetes, LED, and associated risk factors and identifying effective LED prevention strategies will help reduce the burden of mobility limitation in the United States. NHANES is an ongoing, cross-sectional survey of representative samples of the U.S. civilian noninstitutionalized population. The survey uses a complex multistage probability design. Data are collected through in-person interviews and medical examinations. During 1999--2002, NHANES participants were asked, "Other than during pregnancy, have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?" Participants who answered "yes" to this question were classified as having diagnosed diabetes; if the answer was "no" or "borderline," participants were classified as not having diagnosed diabetes. LED was defined as the presence of either PAD (ankle/brachial blood pressure ratio <0.9), PN (one or more insensate areas, on the basis of monofilament testing of foot sensation), self-report of foot/leg ulcers, or technician-observed toe or foot lesion or amputation. Further details of these measures have been described previously (5). Mobility limitation was determined on the basis of participants' response to the questions, "How much difficulty do you have walking for a quarter of a mile; walking up 10 steps without resting; and walking from one room to another on the same level?" Participants who responded "some difficulty," "much difficulty," or "unable to do" to one or more of the three questions were classified as having mobility limitation; participants who responded "no difficulty" to all three questions were classified as having no mobility limitation. Prevalence of mobility limitation was calculated for adults with and without diagnosed diabetes and LED by age and sex for participants aged >40 years who had complete data in the interview and examination variables of interest (n = 4,689); of the 6,059 persons aged >40 years who received the health examination, 1,370 (23%) were excluded from the analysis because of missing data. All reported percentages and 95% confidence intervals (CIs) were estimated using examination weights and taking into account the complex sampling design. Data were age-adjusted to the 2000 U.S. standard population using the age groups 40--59 years, 60--74 years, and >75 years. Logistic regression analysis was used to assess the association of diabetes status and LED status with mobility limitation, including whether an interaction existed between diabetes status and LED status in their associations with mobility limitation, after adjusting for demographic characteristics. The age-adjusted prevalence of mobility limitation among adults with diagnosed diabetes was greater than for those without diagnosed diabetes overall (27% and 16%, respectively) and in each age and sex group. The age-adjusted prevalence of mobility limitation among those with LED was also greater than for those without LED overall (26% and 15%, respectively) and in each age and sex group (Table). Overall, adults with diagnosed diabetes but without LED had a similar prevalence of mobility limitation as adults with LED but without diagnosed diabetes (23% and 25%, respectively). Those with diagnosed diabetes and LED had a prevalence of mobility limitation greater than those with either condition alone and almost three times greater than those with neither condition (39% and 14%, respectively). In a logistic regression model that included both diagnosed diabetes and LED, after data were adjusted for age, sex, and race/ethnicity, the odds of mobility limitation were greater for adults with diagnosed diabetes (odds ratio [OR] = 2.0; CI = 1.4--3.0) than adults without diagnosed diabetes; the odds of mobility limitation were also increased among adults with LED (OR = 2.3; CI = 1.7--2.9) compared with adults without LED. No statistically significant interaction between diabetes status and LED status existed (i.e., the relative odds of mobility limitation for persons with diagnosed diabetes or LED were additive overall and not modified by the presence of both conditions). Among persons with mobility limitation, the most frequently reported mobility limitations were related to walking a quarter mile and walking up 10 steps without resting (Figure). Among those who had both diagnosed diabetes and LED, 33% reported difficulty walking a quarter of a mile and difficulty walking up 10 steps; 6% reported having difficulty walking from one room to another on the same level, which is the most severe form of mobility limitation analyzed. Reported by: MS Eberhardt, PhD, S Saydah, PhD, R Paulose-Ram, PhD, National Center for Health Statistics; M Tao, PhD, EIS Officer, CDC. Editorial Note:Diabetes has long been identified as one of the major factors associated with mobility limitation (6,7). The findings in this report suggest a statistically significantly higher prevalence of mobility limitation among adults aged >40 years who had diagnosed diabetes compared with those without diagnosed diabetes. The cross-sectional design of NHANES does not permit an investigation into the causal pathway for mobility limitation; however, research has indicated that PN and PAD, as well as other diabetic complications (e.g., vision loss) or comorbidities (e.g., obesity, cardiovascular disease, or arthritis), are predictors of mobility limitation among persons with type 2 diabetes (2). Studies have also demonstrated that LED has an independent effect on mobility among older persons (3,4). Consistent with previous findings, this report indicates substantially higher percentages of mobility limitation among adults aged >40 years with LED but without diabetes, compared with those with neither condition. In this sample of the noninstitutionalized U.S. population, only a small percentage (6%) of those with diagnosed diabetes and LED reported difficulty moving from one room to another on the same level, which can impair a person's ability to perform activities of daily living. A larger percentage reported impaired ability to walk a quarter mile or climb 10 steps without resting. Such physical limitations can affect a person's ability to live independently or participate in community life and might decrease well being. The findings in this report are subject to at least three limitations. First, NHANES does not include institutionalized persons, such as those in long-term--care facilities, a population less healthy and more likely to have functional limitations. Second, the sample size was not sufficiently large to analyze additional factors related to mobility limitations (e.g., comorbidities) through bivariate analysis. Finally, among the 6,059 persons aged >40 years who received the health examination, 1,370 (23%) were excluded from the analysis because of missing data; because persons with missing data were older and more likely to have diagnosed diabetes, the prevalence of mobility limitation is probably underestimated. As the U.S. population ages and the prevalence of diabetes increases, LED and its health consequences, including chronic ulcers in feet or legs, amputations, and mobility limitations, will become increasing public health concerns. Proper foot care is one example of preventive care that might help reduce the prevalence of LED and mobility limitations. CDC's national diabetes surveillance data for 2003 indicated that only 67% of persons with diabetes reported receiving an annual foot examination, even though 88% reported having an annual doctor visit (8). CDC collaborates with state health departments and communities to prevent and manage LED to minimize its impact on mobility. The National Diabetes Education Program has developed materials related to LED and foot care for persons with diabetes and their health-care providers (available at http://www.ndep.nih.gov/campaigns/feet/feet_overview.htm). References
Table 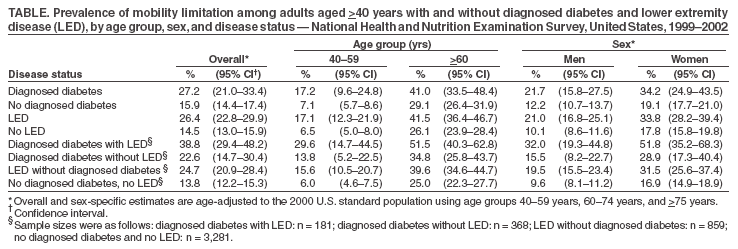 Return to top. Figure 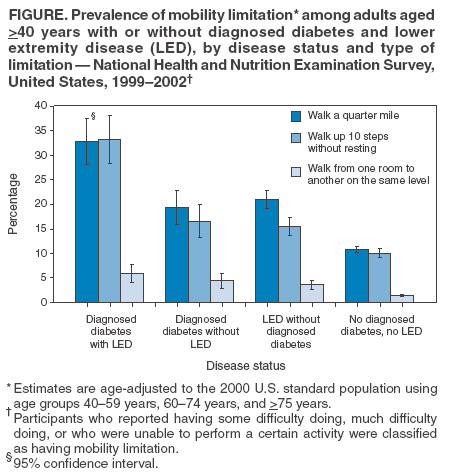 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Date last reviewed: 11/22/2005 |
|||||||||
|