 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Hypothermia-Related Deaths --- United States, 2003--2004Hypothermia, a reduction in the body's core temperature to <95.0°F (<35.0°C), is a preventable medical emergency usually caused by prolonged exposure to cold temperatures without adequate protective clothing (1). Warning signs and symptoms of hypothermia include lethargy, weakness and loss of coordination, confusion, uncontrollable shivering, and reduced respiratory or heart rate (2). Common risk factors are advanced age, substance abuse, altered mental status, and increased contact with substances that promote heat loss, such as water (3). This report describes three hypothermia-related deaths that occurred in the United States during 2003--2004, summarizes hypothermia-related mortality during 1979--2002, describes risk factors for and symptoms of hypothermia, and reviews measures to prevent hypothermia-related injury and death. Public health strategies tailored to persons at increased risk for exposure to excessive cold might help reduce hypothermia-related morbidity and mortality. Case Reports, 2003--2004Case 1. In December 2003, a man aged 69 years with dementia was reported missing from his residence in Vermont. Despite extensive searches, his body was not found until March 2004 in the backyard of a nearby home. During that period, outdoor temperatures ranged from -14°F to 57°F (-26°C to 14°C). Descriptions and photographs of the scene suggested that the man had tried to cover himself to keep warm. Cause of death was reported as hypothermia, with dementia as a contributing factor. Case 2. In February 2004, a male aged 16 years was found dead 40 yards from a road in a rural park in northwestern New Mexico. He had last been seen alive the previous day when he was dropped off at high school. The boy was found wearing damp, light clothing; his jacket and neck chain were recovered a short distance away. Temperatures in this region ranged from 11°F to 42°F (-12°C to 6°C) on the day he was found. An autopsy identified minor abrasions and contusions on his face and extremities. His blood alcohol concentration (BAC) was 0.15 g/dL, nearly twice the state legal limit of 0.08 g/dL for drivers. Toxicologic analysis of blood and urine also revealed 2 ng/mL of delta-9-tetrahydrocannabinol (THC) and 50 ng/mL of delta-9-carboxy-THC, both active ingredients in marijuana that suggest recent or chronic marijuana use. The cause of death was certified as hypothermia from cold exposure, with alcohol and marijuana intoxication as contributing factors. Case 3. In February 2004, a man aged 18 years was found dead near a creek in southeastern Alaska. He was dressed lightly for winter conditions. The man had been missing for approximately 1 day, during which temperatures had ranged from 39°F to 45°F (4°C to 7°C). Toxicologic testing revealed a BAC of 0.18 g/dL, twice the state legal limit of 0.08 g/dL for drivers, and a urine ethanol concentration of 0.28 g/dL. The cause of death was listed as combined effects of alcohol intoxication and hypothermia. Hypothermia-Related Mortality, 1979--2002During 1979--2002, a total of 16,555 deaths in the United States, an average of 689 per year (range: 417--1,021), were attributed to exposure to excessive natural cold (International Classification of Diseases, Ninth and Tenth Revision ICD-9 codes E901.0, E901.8, and E901.9; ICD-10 code X31) (Figure 1) (4). Annual death rates were highest before 1990 (range: 0.3--0.4 per 100,000 population), then decreased to 0.2 beginning in 1991, except for an increase to 0.3 in 2000. In 2002, a total of 646 hypothermia-related deaths were reported, with an annual death rate of 0.2 per 100,000 population. The majority of reported hypothermia-related deaths (66%) occurred in males (Figure 2), but the overall death rate (0.5) was the same for both males and females. Fifty-two percent of all decedents were aged >65 years, and 50% were male. The death rate for males and females aged >65 years was 1.2 and 0.8, respectively. Forty-five percent of all reported deaths occurred among white males (death rate: 0.3), and 14% occurred among black males (0.5). States with the greatest overall death rates for hypothermia in 2002 were Alaska (3.0), New Mexico (0.9), North Dakota (0.9), and Montana (0.8). In addition, hypothermia-related deaths were reported by states with characteristically milder climates that experience rapid temperature changes (e.g., North Carolina [0.4] and South Carolina [0.4]) and by western states that have high elevations and experience considerable changes in nighttime temperatures (e.g., Arizona [0.3]). Reported by: F Fallico, MD, Alaska Dept of Health and Social Svcs. K Nolte, MD, Office of the Medical Investigator, Univ of New Mexico School of Medicine, Albuquerque, New Mexico. L Siciliano, Vermont Dept of Health. Div of Environmental Hazards and Health Effects, National Center for Environmental Health; F Yip, PhD, EIS Officer, CDC. Editorial Note:All hypothermia-related deaths are preventable. Early recognition of the signs and symptoms of hypothermia and awareness of key risk factors can help minimize morbidity and mortality from exposure to extreme cold. Hypothermia can be classified as mild (core body temperature: 90.0°F to <95.0°F [32.2°C to <35.0°C]), moderate (82.5°F to <90.0°F [28.0°C to <32.2°C]), or severe (<82.5°F [<28.0°C]) (5). Onset of hypothermia is not always evident, although shivering, numbness, lethargy, poor coordination, and slurred speech are typical early manifestations. Among infants, warning signs also include bright red skin and low energy. When body temperature is <90.0°F [<32.2°C], shivering might not be evident, and the victim might not feel cold. In severe hypothermia, the victim loses consciousness, and a pulse might not be apparent (6). Understanding the risk factors for hypothermia can help identify populations at risk. This report highlights three risk factors for hypothermia-related deaths: advanced age (>65 years), mental impairment, and substance abuse. Additional contributing factors can include homelessness, dehydration, and serious medical conditions (2). Older persons are at particular risk because their lower metabolic rate might prevent their maintaining normal body temperatures when indoor or outdoor temperatures fall below 64.4°F (18.0°C) (1). Older persons also might not perceive cold as well as younger persons and might be slow to compensate for the cold. Hypothyroidism and diabetes can contribute to hypothermia risk through decreased metabolic rate and hypoglycemia, respectively (3). Substance abuse is another potential contributor to hypothermia; alcohol and drug use (e.g., sedatives or phenothiazines) can suppress vasoconstriction and the shivering response through cutaneous vasodilation, alter decision-making, and decrease awareness of and response to hazardous environmental conditions (3). Immediate medical attention should be sought for persons who exhibit signs of hypothermia. Wet clothing should be removed and further heat loss prevented by warming the center of the body, using blankets for passive rewarming. Although victims might appear dead, cardiopulmonary resuscitation should be provided during warming until they respond or until medical aid becomes available (6). Active rewarming, especially among persons with moderate to severe hypothermia, typically involves administration of warmed intravenous fluids or rewarming of the airways. To prevent hypothermia-related deaths, public health strategies should target persons at greatest risk. During cold periods, relatives, neighbors, and caretakers of persons at high risk for hypothermia, particularly those of advanced aged, should check frequently on their condition, familiarize themselves with signs of hypothermia, and take appropriate preventive action. Health departments in states characterized by milder winter climates but rapid temperature changes should identify groups at high risk for hypothermia, ensure that proper resources are available to them to minimize exposure to cold, and maintain communication with them regarding preventive measures. Educating public safety personnel and hospital staff to better recognize hypothermia victims and to familiarize themselves with initial treatments also can help prevent hypothermia-related morbidity and mortality. Because certain signs of hypothermia, such as confusion and loss of coordination, can resemble alcohol intoxication, hypothermia victims might be sent to detoxification centers before they are sent to hospitals. Workers at detoxification centers should be aware of signs and risk factors for hypothermia and be instructed to take the temperature of potential hypothermia victims at admission (7). References
Figure 1 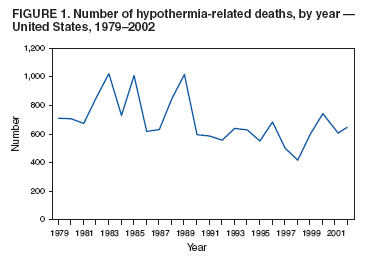 Return to top. Figure 2 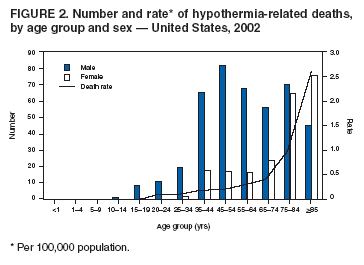 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 2/24/2005 |
|||||||||
This page last reviewed 2/24/2005
|