 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Survey of Airport Smoking Policies --- United States, 2002Exposure to secondhand smoke (SHS) causes approximately 38,000 deaths among nonsmokers each year in the United States (1,2). The Task Force on Community Preventive Services has documented strong scientific evidence that smoking bans and restrictions are effective in reducing exposure to SHS (3). In 2002, an estimated 1.9 million workers had jobs at U.S. airports, and more than 1.9 million passengers per day passed through these airports (4). During the fall of 2002, the Center for Health Promotion and Disease Prevention at the Henry Ford Health System (Detroit, Michigan) conducted the Airport Smoking Policy Survey. This report summarizes the key findings from that survey, which indicated that 61.9% of airports reported being smoke-free in 2002 and that larger airports, which account for the majority of passenger boardings, were less likely than smaller airports to have a smoke-free policy. Increased adoption and enforcement of smoke-free policies are needed to protect the health of workers and travelers at U.S. airports. During September--November 2002, a cross-sectional telephone survey was conducted with appropriate personnel at primary commercial-service airports. Primary commercial-service airports are defined as airports having more than 10,000 passenger boardings per year. These airports receive hub size designations (i.e., large hub, medium hub, small hub, and nonhub) from the Federal Aviation Administration (FAA) based on the percentage share of total U.S. passenger boardings an airport accounted for during the previous calendar year (5). Large hubs account for at least 1% of total passenger boardings by scheduled air carriers in the 50 states, the District of Columbia, and other U.S. areas designated by FAA; medium hubs account for 0.99%--0.25%; small hubs account for 0.249%--0.05%; and nonhubs account for less than 0.05% but more than 10,000 boardings annually. Using 2001 FAA passenger boarding data, the survey targeted all large- (n = 31), medium- (n = 35), and small-hub (n = 71) airports and a simple random sample of nonhub airports (64 of 282). Large-hub, medium-hub, small-hub, and nonhub airports accounted for 69.3%, 19.8%, 7.6%, and 3.2%, respectively, of all U.S. passenger boardings in 2001 (5). The survey collected information on the locations (if any) where smoking was allowed at the airport; whether designated smoking areas were enclosed or physically separated from the rest of the airport and whether they had a separate ventilation system; whether airports required smokers to be a minimal distance from airport entrances while smoking outside airport buildings; and methods by which the no-smoking message was communicated to employees, passengers, and visitors at the airport (i.e., written policies, signage, or announcements on the public address system). For this study, a smoke-free airport was defined as an airport that prohibited smoking by anyone, anywhere, and at any time inside the airport. Overall, 197 (98.0%) of the targeted airports participated in the survey, including all 31 large-hub, 34 of 35 medium-hub, 69 of 71 small-hub, and 63 of 64 nonhub airports. Survey results demonstrated airport size to be inversely related to the percentage of airports having a smoke-free policy (Table 1). Smoke-free policies were reported by 122 (61.9%) airports, including 13 (41.9%) large-hub airports, 18 (52.9%) medium-hub airports, 40 (58.0%) small-hub airports, and 51 (81.0%) nonhub airports. Among smoke-free airports, the percentage having a written smoking policy varied by hub size, with 76.9% of large-hub, 66.7% of medium-hub, 65.0% of small-hub, and 82.4% of nonhub airports having a written policy. The majority of smoke-free airports (93.4%) had signage concerning their smoke-free policy. Large-hub airports were more likely to report having public address announcements about their smoking policy than were airports of smaller hub size (Table 1). Travelers and airport employees are also at risk for being exposed to SHS when entering, leaving, or working outside of airport buildings. The 122 smoke-free airports were more likely to have designated outdoor smoking areas (71.3%) than were the 75 non--smoke-free airports (44.0%) (Table 2). Smoke-free airports were also more likely (55.7%) than non--smoke-free airports (20.0%) to require that persons maintain a minimum distance from entrances when smoking outside airport buildings. Reported by: ES Pevzner, MPH, Univ of North Carolina at Chapel Hill. RM Davis, MD, Center for Health Promotion and Disease Prevention, Henry Ford Health System, Detroit, Michigan. WKY Pan, DrPH, Johns Hopkins Univ Bloomberg School of Public Health, Baltimore, Maryland. CG Husten, MD, T Pechacek, PhD, A Malarcher, PhD, Office on Smoking and Health, CDC. Editorial Note:The results of the Airport Smoking Policy Survey indicate that travelers and employees at many U.S. airports lack adequate protection from SHS. At the time of the survey, fewer than half of large-hub airports, which service nearly 70% of all airline travelers passing through U.S. airports, were smoke-free. As a result of heightened security following the attacks of September 11, 2001, travelers and airline employees are spending more time in and around U.S. airports and might now be at greater risk for prolonged exposure. SHS is a known human carcinogen (6), and the Surgeon General has concluded that exposure to SHS causes lung cancer among persons who have never smoked (7). The workplace is a major source of SHS exposure, and workplace exposure to SHS is a key predictor of total exposure to tobacco smoke as measured by levels of cotinine, a metabolite of nicotine (2). No safe level of exposure to SHS is known. A recent study indicated that nonsmokers who spent as little as 4 hours in a well-ventilated casino that permitted smoking had significant increases in NNK [4- (methylnitrosamino)-1-(3-pyridyl)-1-butanone], a tobacco-specific lung carcinogen (8). Moreover, low levels of exposure increase the risk for acute myocardial infarction and coronary heart disease (9). Therefore, airport employees and travelers, like employees and patrons at any workplace that permits smoking, are at elevated risk for death and disease caused by SHS (10). Public health authorities recommend that smoking be prohibited in all indoor environments. Smoking lounges and designated smoking areas do not provide sufficient protection because tobacco smoke drifts from smoking to no-smoking areas and smoke-contaminated air is recirculated through a common ventilation system in most buildings where smoking is allowed. When smoking is permitted indoors, authorities recommend that it be confined to a designated area that is separately ventilated and physically separated from adjacent no-smoking areas (10). The findings in this report are subject to at least four limitations. First, the data are based on self-reports of survey participants. However, whenever possible, the survey interviewer spoke with airport personnel who were in the best position to answer the questions in the survey, and follow-up telephone contacts were made whenever necessary to maximize the accuracy and completeness of the information collected. Second, not all medium-, small-, and nonhub airports responded to the survey. However, because nonresponse rates were low (2.9%, 2.8%, and 1.6% for medium-, small-, and nonhub airports, respectively), this potential bias was minimal. Third, the study did not measure the level of tobacco-smoke constituents within the airport environments. Finally, the study did not measure compliance with or enforcement of smoke-free airport policies, and the results might underestimate potential exposure to SHS. Poor compliance with or failure to publicize and enforce smoke-free airport policies would provide little if any protection from SHS exposure among travelers and airport employees. Further studies are needed to assess compliance with and enforcement of smoke-free airport policies to verify the elimination of SHS at "smoke-free" airports. Since the Airport Smoking Policy Survey was completed in November 2002, Connecticut, Delaware, Maine, Massachusetts, and New York have joined California in adopting statewide legislation requiring all workplaces (including restaurants and bars) to be smoke-free. The adoption of smoke-free workplace legislation in these states means that eight additional airports (two large-hub, two medium-hub, and four small-hub airports) that were not smoke-free at the time the survey was conducted are now smoke-free. Several other states and localities are currently considering the adoption of smoke-free workplace legislation, which would further increase the number of smoke-free airports. Nevertheless, the findings from this study demonstrate that many U.S. airports are still not smoke-free and that further efforts are needed to protect airline travelers and airport employees from exposure to SHS at U.S. airports. Acknowledgments The findings in this report are based, in part, on contributions by the Flight Attendant Medical Research Institute, Miami, Florida. C Mack, Henry Ford Health System, Detroit, Michigan. S Glasgow, Federal Aviation Administration. References
Table 1 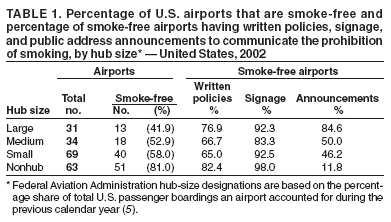 Return to top. Table 2 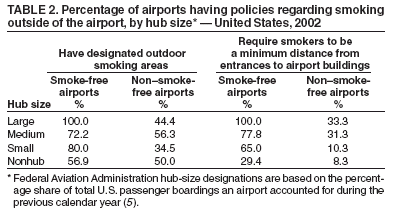 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 12/22/2004 |
|||||||||
This page last reviewed 12/22/2004
|