 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Asthma Prevalence and Control Characteristics by Race/Ethnicity --- United States, 2002During 1980--1999, asthma prevalence, morbidity, and mortality increased among U.S. adults. These annual rates were higher among certain racial/ethnic minority populations than among whites (1). In addition, racial/ethnic minority populations reported higher use of emergency departments (EDs) and doctors' offices for asthma treatment than whites (1). To assess asthma prevalence and asthma-control characteristics among racial/ethnic populations, CDC analyzed 2002 data from the Behavioral Risk Factor Surveillance System (BRFSS). This report summarizes the results of that analysis, which indicated that among the estimated 16 million (7.5%) U.S. adults with asthma, self-reported current asthma prevalence among racial/ethnic minority populations ranged from 3.1% to 14.5%, compared with 7.6% among whites. Comprehensive state-specific asthma surveillance data are necessary to identify disparities in asthma prevalence and asthma-control characteristics among racial/ethnic populations and to develop targeted public health interventions. BRFSS is a state-based, random-digit--dialed telephone survey of the noninstitutionalized, civilian U.S. population aged >18 years. The survey collects information about modifiable risk factors for chronic diseases and other leading causes of death and is administered in English and Spanish. In 2002, two questions about asthma were used in the core survey by the 54 reporting areas (i.e., the 50 states, the District of Columbia [DC], Guam, Puerto Rico, and the U.S. Virgin Islands [USVI]). Lifetime asthma was defined as a "yes" response to the question, "Have you ever been told by a doctor, nurse, or other health professional that you have asthma?" Current asthma was defined as a "yes" response to the same question and the question, "Do you still have asthma?" Weighted prevalence estimates and 95% confidence intervals (CIs) were calculated by using SUDAAN to account for the complex survey design. In 2002, the median response rate for all 54 reporting areas was 58.3% (range: 42.2% [New Jersey]--82.6% [Minnesota]) (2). The overall prevalence of lifetime asthma for the 54 reporting areas was 11.9% (N = 247,646) (range: 8.6% [South Dakota]--19.6% [Puerto Rico]). Within the 50 states and DC, lifetime asthma prevalence was 11.8% (range: 8.6% [South Dakota]--14.5% [Montana]). The prevalence of current asthma in the 54 reporting areas was 7.6% (range: 4.7% [USVI]--11.5% [Puerto Rico]). Within the 50 states and DC, current asthma prevalence was 7.5% (range: 5.8% [South Carolina]--10.0% [Maine]) (Table 1). Eight questions in the Adult Asthma History Module were used in 19 areas* to examine the asthma-control characteristics among respondents with current asthma in eight racial/ethnic populations: 1) non-Hispanic whites, 2) non-Hispanic blacks, 3) non-Hispanic Asians, 4) non-Hispanic American Indians/Alaska Natives (AI/ANs), 5) non-Hispanic Native Hawaiians/Pacific Islanders (NH/PIs), 6) non-Hispanic persons reporting "other" race/ethnicity, 7) non-Hispanic persons reporting multiple races/ethnicities, and 8) Hispanics. Respondents with current asthma were asked to report the 1) number of ED visits during the preceding 12 months, 2) number of doctors' office visits for urgent care during the preceding 12 months, 3) number of routine check-ups for asthma during the preceding 12 months, 4) presence of asthma attacks or episodes during the preceding 12 months, 5) presence of asthma symptoms during the preceding 30 days, 6) number of days with sleep disturbances during the preceding 30 days, 7) use of medication during the preceding 30 days, and 8) number of days with activity limitation during the preceding 12 months. Respondents who answered "yes" or provided a numeric response (other than zero) to any question were coded as "yes" to the question, and all other responses were coded as "no." Respondents who answered "don't know" or who refused to answer the question were excluded. The overall current asthma prevalence in the 19 areas using the adult asthma module without race/ethnicity stratification was 7.3% (95% CI = 6.9%--7.6), compared with 7.6% for all 54 reporting areas. Current asthma prevalence in the 19 areas ranged from 4.7% (USVI) to 9.1% (DC). Current asthma was highest among non-Hispanic respondents of multiple races (15.6%), followed by non-Hispanic AI/ANs (11.6%), non-Hispanic blacks (9.3%), non-Hispanic whites (7.6%), non-Hispanic persons of "other" race/ethnicity (7.2%), Hispanics (5.0%), non-Hispanic Asians (2.9%), and non-Hispanic NH/PIs (1.3%) (Table 2). Hispanic respondents in Puerto Rico reported higher current asthma (11.6%) than Hispanic respondents in the 19 areas using the adult asthma module (5.0%) and Hispanic respondents in the 50 states and DC (5.5%). Among respondents with current asthma, ED visits were reported with greater frequency by non-Hispanic black (37.2%) and Hispanic (26.0%) respondents and least frequently by non-Hispanic multiracial respondents (13.5%). Non-Hispanic white and non-Hispanic Asian respondents were the least likely to report doctors' office visits for urgent care (25.8% and 17.1%, respectively). These two racial/ethnic populations exhibited the most positive asthma-control profile, with moderate-to-low percentages of respondents reporting each of the negative indicators (i.e., ED visits, urgent care visits, symptoms, attacks, sleep disturbance, and activity limitation). Both racial/ethnic populations also reported a moderate-to-low frequency of routine doctors' visits for asthma care and medication use. Non-Hispanic black, AI/AN, multiracial, and Hispanic respondents all had less positive asthma profiles, with high percentages reporting three to five of the six negative indicators. Reported by: L Rhodes, MPH, CM Bailey, MS, JE Moorman, MS, Div of Environmental Hazards and Health Effects, National Center for Environmental Health, CDC. Editorial Note:Asthma is a chronic respiratory illness often associated with familial, allergenic, socioeconomic, psychological, and environmental factors (3). Although recent reports suggest asthma-related mortality has been declining since 1996, a disparity remains between rates for non-Hispanic whites and those for non-Hispanic blacks and other racial/ethnic populations (4). Non-Hispanic blacks experience higher rates than non-Hispanic whites for ED visits, hospitalizations, and deaths; these trends are not explained entirely by higher asthma prevalence among non-Hispanic blacks (4). Other racial/ethnic populations experience higher asthma mortality and hospitalization rates than non-Hispanic whites while also reporting lower asthma prevalence and fewer outpatient and ED visits. The asthma-control characteristics described in this report can contribute to increased mortality and higher hospitalization rates. In 2002, the BRFSS adult lifetime asthma prevalence estimate and the adult current asthma prevalence estimate for the 50 states and DC were higher than in 2001 and 2000. Consistent with previous BRFSS findings, the data in this report indicate variability across states and territories in the lifetime and current asthma estimates. In addition, racial/ethnic populations with the highest current asthma prevalence in 2001 (non-Hispanics of multiple races, non-Hispanic AI/ANs, and non-Hispanic blacks) reported higher adult current asthma prevalence in 2002. Non-Hispanic whites also reported higher adult current asthma prevalence in 2002 than in 2001. Although non-Hispanic Asians reported the lowest current asthma prevalence in 2001, current asthma prevalence decreased in 2002 in contrast to the increases reported by other racial/ethnic populations. Non-Hispanic NH/PIs also reported a decrease in current asthma prevalence in 2002, compared with 2001. Higher current asthma prevalence cannot be explained by the distribution of BRFSS respondents by race/ethnicity because the change in any racial/ethnic population in the BRFSS data was <1% from 2001 to 2002. Possible reasons for variability include demographic, socioeconomic (e.g., income and education level), and environmental factors (e.g., outdoor air pollution and climate), physician diagnostic procedures, or data-collection practices (3). The findings in this report are subject to at least four limitations. First, the median response rate for the survey was 58.3%. However, BRFSS asthma prevalence is similar to estimates from other surveys with higher response rates, such as the National Health Interview Survey (5). Second, BRFSS does not measure asthma prevalence among institutionalized adults, military personnel, persons aged <18 years, and residents without telephones. Third, the validity of self-reported asthma or asthma-control characteristics in BRFSS is unknown (6). Actual adherence to prescribed medication or asthma treatment plans in respondents with current asthma is unknown. Finally, the asthma-control questions were asked in 19 of the 54 BRFSS reporting areas and might not accurately reflect the asthma-control characteristics of other reporting areas or accurately represent their racial/ethnic distribution. States and territories using the BRFSS Adult Asthma History module can direct asthma management within their jurisdictions and address disparities in asthma risk and control characteristics among racial/ethnic populations. Use of comprehensive state-specific asthma surveillance data to identify populations with poorly controlled asthma is instrumental in developing, implementing, and evaluating asthma-control programs and interventions. Acknowledgment This report is based on data contributed by state BRFSS coordinators. References
* California, Delaware, District of Columbia, Idaho, Iowa, Louisiana, Massachusetts, Michigan, New Hampshire, New Jersey, New Mexico, North Carolina, Ohio, Oklahoma, Rhode Island, Texas, Utah, Wisconsin, and the U.S. Virgin Islands.
Table 1 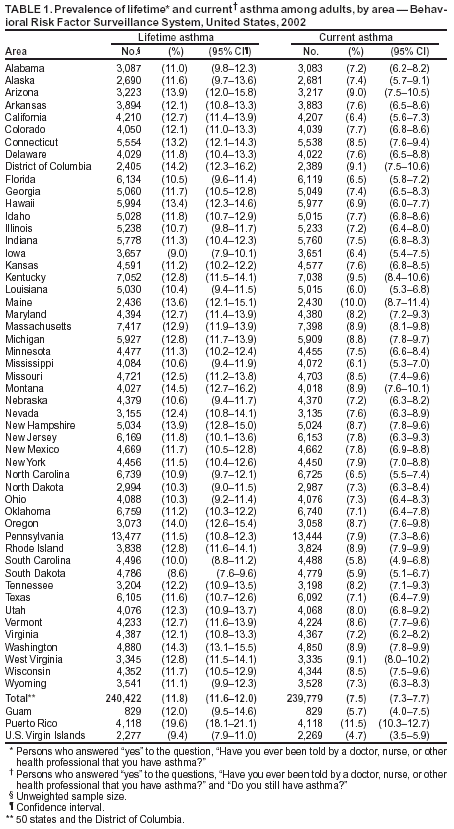 Return to top. Table 2  Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 2/26/2004 |
|||||||||
This page last reviewed 2/26/2004
|