 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. History of Foot Ulcer Among Persons with Diabetes --- United States, 2000--2002Foot ulcers and lower extremity amputations (LEAs) are disabling complications of diabetes and lower extremity disease (1,2). In the United States, approximately 60% of all LEAs occur among persons with diabetes (3); of these LEAs, approximately 85% are preceded by a foot ulcer (4). To estimate the percentage of U.S. adults with diabetes who had a history of a foot ulcer, CDC analyzed data from the 2000--2002 Behavioral Risk Factor Surveillance System (BRFSS). This report summarizes the findings of that analysis, which indicate that persons with longer duration of diabetes who used insulin and who smoked were most likely to have a history of foot ulcer. Persons with diabetes can benefit from interventions that prevent or delay foot ulcer and LEAs. BRFSS is a state-based, random-digit--dialed telephone survey of the U.S. civilian, noninstitutionalized population aged >18 years. BRFSS is conducted in the 50 states, the District of Columbia (DC), Puerto Rico, Guam, and the U.S. Virgin Islands. The median response rate was 48.9% (range: 28.8%--71.8%) in 2000, 51.1% (range: 33.3%--81.5%) in 2001, and 58.6% (range: 42.2%--82.6%) in 2002. Persons with diabetes were defined as respondents who answered "yes" to the question, "Have you ever been told by a doctor that you have diabetes?" Women who were told they had diabetes only during pregnancy were excluded. Persons who reported they had diabetes were asked questions regarding foot ulcer from the diabetes module. Persons with a history of foot ulcer were defined as those who responded "yes" to the question, "Have you ever had any sores or irritations on your feet that took >4 weeks to heal?" Other questions from the diabetes module included the following: "How old were you when you were told you had diabetes?"; "Are you now taking insulin?"; "About how often do you check your blood for glucose or sugar?"; and "Have you ever taken a course or class in how to manage your diabetes?" A total of 44 states and DC reported information from the diabetes module for at least 2 years during 2000--2002. Data were weighted to reflect the age, sex, and racial/ethnic distribution in each area. The percentage of persons with diabetes who had a history of foot ulcer was analyzed by using the selected questions from the diabetes module, selected sociodemographic characteristics, obesity (body mass index >30), smoking status, and area of residence. Logistic regression analysis was used to determine the independent associations of various risk factors among persons with a history of foot ulcer. All analyses were conducted by using SAS v8 software with SUDAAN to estimate standard errors and confidence intervals, and t-tests were used to test for significant differences between groups. Prevalence was age-adjusted according to the 2000 U.S. standard population. During 2000--2002, an estimated 11.8% of U.S. adults with diabetes had a history of foot ulcer (Table 1). The percentage decreased with increasing age and increased with longer duration of disease (p<0.001, t-test for trend). The percentage was lower among non-Hispanic blacks than among non-Hispanic whites or Hispanics (p<0.01) and lower among married or cohabitating persons than among persons who were not (p<0.001). Foot ulcers were significantly more prevalent among persons who were obese than among those who were not (p<0.001) and among insulin users than among persons who did not use insulin (p<0.001). The prevalence of foot ulcer increased with smoking, from 10.3% among nonsmokers to 11.9% among former smokers to 15.8% among current smokers (p<0.001, t-test for trend). The percentage did not differ significantly by sex, education level, health insurance coverage, blood sugar monitoring, and diabetes management education. In multivariate analyses, younger age, longer duration of disease, white race, Hispanic ethnicity, not being married or cohabitating, obesity, insulin use, and smoking all were associated independently with a history of foot ulcer. The strongest associations were duration of disease of >21 years (odds ratio [OR] = 2.3), insulin use (OR = 1.6), and current smoking (OR = 1.6). Overall, the age-adjusted prevalence of a history of foot ulcer among persons with diabetes was 12.7% (Table 2). Of the 45 areas (44 states and DC) that reported information from the BRFSS diabetes module, Indiana (16.3%), California (16.2%), and Nevada (16.2%) had the highest age-adjusted prevalence of a history of foot ulcer among persons with diabetes, and Colorado (7.4%), Wisconsin (8.8%), and Hawaii (8.9%) had the lowest (Table 2). Reported by: ME Aguiar, MSPH, NR Burrows, MPH, J Wang, MPH, JP Boyle, PhD, LS Geiss, MA, MM Engelgau, MD, Div of Diabetes Translation, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings in this report indicate that approximately 12% of U.S. adults with diabetes had a history of foot ulcer, a risk factor for further ulceration or LEA. This analysis identifies risk factors for foot ulcer and underscores the need to improve foot-related preventive care practices among persons with diabetes, particularly those with longer duration of disease who use insulin and who smoke. Among persons with diabetes, foot ulcers and LEAs can be reduced by 44%--85% (5). These persons should receive annual foot examinations to identify high-risk foot conditions (e.g., peripheral neuropathy, peripheral arterial disease, foot deformities, and history of ulcer or LEAs), and persons with one or more high-risk foot conditions should receive more frequent evaluations (6). Preventive strategies should focus on 1) glycemic control to reduce neuropathy, 2) smoking cessation or prevention, 3) early detection and appropriate management of persons with high-risk foot conditions, 4) provider education, 5) patient education on daily foot care, 6) use of proper footwear, and 7) health-care interventions to improve care (e.g., chart reminders and patient tracking) (6--8). The findings in this report are subject to at least five limitations. First, BRFSS does not include institutionalized persons (e.g., nursing home residents) or persons without telephones. Second, BRFSS data are self-reported and subject to recall bias. These two limitations might explain in part why younger age was associated with a higher prevalence of a history of foot ulcer. Third, factors that were not significant in the analysis (e.g., blood glucose monitoring and diabetes management education) might be confounded with longer duration and severity of disease (e.g., insulin use), and health insurance coverage might not include appropriate foot care. Fourth, the median BRFSS response rate was only 58.6% in 2002; however, BRFSS data have minimal bias compared with census data (http://www.cdc.gov/brfss). Finally, the analysis included data from 44 states and DC and therefore might not be representative of the entire country. CDC conducts surveillance on foot-related preventive care practices and LEAs (http://www.cdc.gov/diabetes/statistics/index.htm) in the United States. To estimate the extent of lower extremity disease and its risk factors, in 1999, CDC and the National Institutes of Health (NIH) included assessments of peripheral vascular disease, peripheral neuropathy, foot deformities, ulcers, and LEAs in the National Health and Nutrition Examination Survey. This information can assist clinicians and public health providers in developing preventive care and community-based interventions. Increasing the proportion of persons with diabetes who receive preventive foot care and reducing LEAs are high public health priorities in the United States and, as such, were included in the national health objectives for 2010. The prevalence of annual foot examinations among persons with diabetes increased during 1995--2001, from 56.0% to 62.3% (9), which is still below the national target of 75% (objective no. 5-14) (10). To improve diabetes-related preventive practices, CDC provides technical assistance to state diabetes prevention and control programs. CDC also collaborates with the Health Resources and Services Administration in the Health Disparities Collaboratives, participates with 13 other agencies in the National Diabetes Quality Improvement Alliance, and cosponsors the National Diabetes Education Program (NDEP) with NIH. NDEP patient education materials on making foot care an essential part of diabetes care are available at http://www.ndep.nih.gov/diabetes/pubs/feet_kit_eng.pdf. References
Table 1 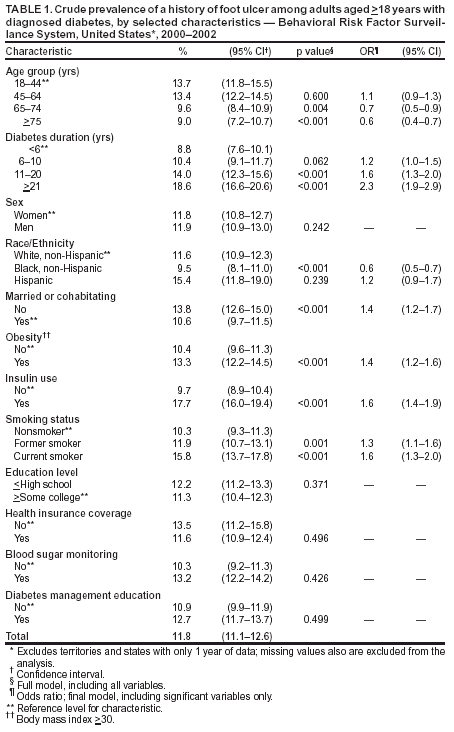 Return to top. Table 2 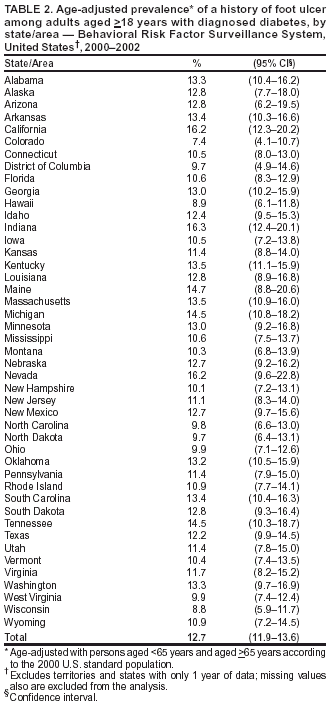 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 11/13/2003 |
|||||||||
This page last reviewed 11/13/2003
|