 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Outbreak of Botulism Type E Associated with Eating a Beached Whale --- Western Alaska, July 2002Botulism is a neuroparalytic illness caused by toxins produced by the bacterium Clostridium botulinum, an obligate anaerobe found commonly in the environment. Intoxication with toxin type E is associated exclusively with eating animal foods of marine (salt or fresh water) origin. Persons who eat raw or fermented marine fish and mammals are at high risk for botulism from type E toxin. On July 17, 2002, the Alaska Division of Public Health investigated a cluster of suspected botulism cases among residents of a fishing village in Alaska. This report summarizes the findings of the outbreak investigation, which linked disease to eating raw muktuk (skin and a pink blubber layer) from a beached whale (Figure). To avoid delays in treatment, health-care providers evaluating patients suspected of having botulism should base treatment decisions on clinical findings. Public health authorities should be notified immediately about any suspected botulism case. During July 13--15, residents of a western Alaska village on the Bering Sea shore shared a meal consisting of muktuk harvested from a beached adult beluga whale found near their village. The villagers estimated that the whale had been dead for at least several weeks. They cut the whale fluke (tail) into pieces and stored them in zipper-sealed plastic bags in a refrigerator until they were eaten 1 or 2 days later. On July 17, after a physician from western Alaska reported three suspected cases of botulism among patients who had eaten the muktuk, the Alaska Section of Epidemiology began an investigation. A case of foodborne botulism was defined as illness in a person who had eaten the muktuk and subsequently had symmetric descending flaccid paralysis of motor and autonomic nerves. Persons who ate muktuk were interviewed and examined, and their hospital records were reviewed. Serum, stool, and gastric contents from patients and leftover blubber were tested for botulinum toxin. Of 14 persons identified who ate the muktuk, eight (57%) had an illness that met the case definition. Five of the eight patients were female; the median age was 73 years (range: 13--83 years). Symptom onset after ingestion of muktuk occurred within 36 hours in all patients (Table). Five patients were hospitalized, four received antitoxin, and two required mechanical ventilation. Three stool, three gastric fluid, and seven serum samples from the eight patients and seven samples of muktuk were tested for botulinum toxin at CDC's National Botulism Surveillance and Reference Laboratory. The diagnostic laboratory received all laboratory specimens on July 26, and results were reported on August 1. Type E toxin was detected in stool from one patient. All seven samples of muktuk were positive for type E botulinum toxin. Reported by: J Middaugh, MD, T Lynn, DVM, B Funk, MD, B Jilly, PhD, Div of Public Health, Alaska Dept of Health and Social Svcs. Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases; S Maslanka, PhD, Div of Applied Public Health Training, Epidemiology Program Office; J McLaughlin, MD, EIS Officer, CDC. Editorial Note:This report summarizes a foodborne outbreak of botulism in a western Alaska village that resulted from residents eating muktuk contaminated with type E botulinum toxin. During 1973--1998, a total of 814 cases and an annual median of 24 cases (range: 14--94 cases) of foodborne botulism were reported to CDC (1); 236 (29%) of these cases occurred in Alaska (CDC, unpublished data, 2003). Although botulism is a rare disease, its presentation is distinctive (Box. Because of the epidemic potential of foodborne botulism, every case should be reported and investigated immediately. All patients suspected of having foodborne botulism should be placed in an intensive care setting, monitored regularly for respiratory function deterioration, and provided mechanical ventilation if necessary. Prompt administration of polyvalent equine-source antitoxin can decrease the progression of paralysis and severity of illness but will not reverse existing paralysis. Botulinum antitoxin is available in the United States only through the public health system. Therefore, rapid clinical diagnosis, notification of public health authorities, and timely administration of antitoxin are imperative (2). Laboratory confirmation of botulinum intoxication cannot be relied on in making treatment decisions because the standard test, the mouse bioassay, requires approximately 4 days for final results (2). In addition, the sensitivity of laboratory testing of clinical samples is low (3,4). In this outbreak, typed toxin was detected in only 8% of samples from patients who had definitive exposure to contaminated muktuk. The probable mode of contamination of the whale in this outbreak was either growth and toxin secretion by C. botulinum present in the intestinal tract of the whale or traumatic introduction of C. botulinum spores into the beached whale tissue from contact with sand, rocks, and driftwood, and subsequent germination and toxin production. C. botulinum type E has been found in Alaska coastline soil (5), and outbreaks of botulism associated with eating beached marine mammals are documented (Alaska Section of Epidemiology, unpublished data, 2003). A previous report on the accumulation of C. botulinum toxins in the North Sea coastal food chain associated with beached whales suggested the disposal of the carcasses as a preventive measure (6). However, because of the impracticality of frequent scanning of the vast Alaska shoreline and high costs associated with disposal, the U.S. Fish and Wildlife Service does not remove beached mammal carcasses regularly. Because of the epidemic potential of foodborne botulism and the status of botulinum toxins as a category A agent of terrorism, health-care providers should be familiar with the presentation of botulism. Treatment is based on clinical diagnosis, and rapid recognition and reporting of cases are the cornerstones of successful public health interventions to prevent additional illnesses. Persons should avoid eating beached marine mammal carcasses and boil raw or fermented Alaska Native dishes >10 minutes before eating to inactivate botulinum toxin. Additional information on botulism prevention is available at http://www.phppo.cdc.gov/phtn/botulism/alaska/alaska.asp and http://www.epi.hss.state.ak.us/pubs/botulism/bot_01.htm. References
Table 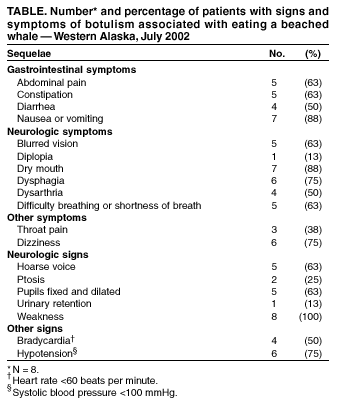 Return to top. Figure  Return to top. Box 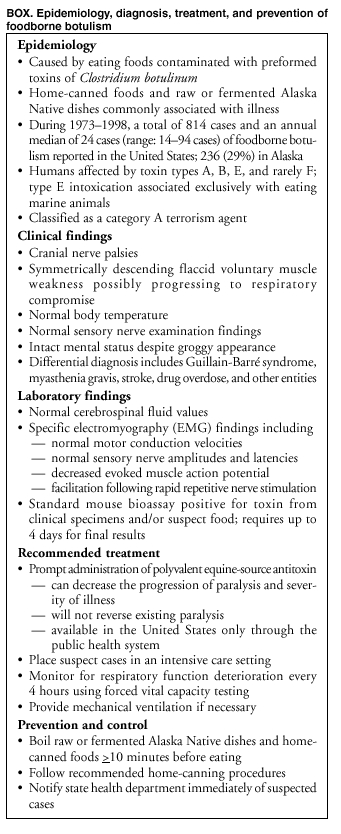 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/16/2003 |
|||||||||
This page last reviewed 1/16/2003
|