 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Trends in Deaths from Systemic Lupus Erythematosus --- United States, 1979--1998Systemic lupus erythematosus (SLE) is a serious autoimmune disease of unknown etiology that can affect several organs. Because SLE affects connective tissues and because painful joints and arthritis are among its most common manifestations, this disease is classified with arthritis and other rheumatic diseases (1). SLE is one of the more fatal forms of rheumatic diseases and non-Causcasian race is a risk factor for death from SLE; however, trends in death from SLE have not been analyzed recently. To characterize deaths from SLE, CDC reviewed SLE deaths during 1979--1998. This report presents the results of that analysis, which indicate that marked age-, sex-, and race-specific disparities exist in SLE death rates and that death rates have increased by approximately 70% during the study period among black women aged 45--64 years. Prevention of deaths requires early recognition and diagnosis of SLE and appropriate therapeutic management. The analysis used National Center for Health Statistics Multiple Cause-of-Death Public Use Data Tapes for 1979--1998. These national mortality statistics were based on data from death certificates filed in state vital statistics offices. Demographic data (e.g., age and race/ethnicity) listed on death certificates were reported by funeral directors, usually from information provided by the decedent's family. Causes of death listed on death certificates were reported by a physician, medical examiner, or coroner by using a format specified by the World Health Organization and endorsed by CDC. An SLE death was defined as any death of a U.S. resident coded with an underlying cause of death of systemic lupus erythematosus (International Classification of Diseases, Ninth Revision, code 710.0). Death rates were calculated by using annual deaths and corresponding U.S. residential population estimates (2). Death rates were calculated for whites and blacks. Rates for other races were not calculated because numbers were too small for meaningful analysis. During 1979--1998, the annual number of deaths increased from 879 to 1,406, and the crude death rate increased from 39 to 52 per 10 million population, with 22,861 deaths reported during the study period (Table 1). Of all SLE deaths, 36.4% occurred among persons aged 15--44 years. For each year, crude death rates increased with age, were >5 times higher among women than men, and were >3 times higher among blacks than whites. Among black women, death rates were highest and increased most (69.7%) among those aged 45--64 years, with little difference in rates among other age groups (Figure 1). Reported by: JJ Sacks, MD, CG Helmick, MD, G Langmaid, JE Sniezek, MD, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings in this report document marked age-, sex-, and race-specific disparities in SLE deaths. Although SLE mortality is most frequently caused by active SLE or by associated organ failure, infection, or cardiovascular disease from accelerated atherosclerosis (3), some studies suggest that renal disease might account for excess SLE deaths among blacks (4). Differential ascertainment and reporting of SLE deaths by race is possible, but probably does not account for the magnitude of observed differences, especially among different age groups for white and black women. A higher incidence of SLE among black women might account for the racial differences in death rates. However, no ongoing population-based studies exist that determine how changes in SLE incidence contributed to the increase in the death rate. Beyond a change in incidence, other remediable reasons for an increase in SLE mortality among black women include later diagnosis, problems in access to care, less effective treatments, and poorer compliance with therapeutic regimens (5). The findings in this report are subject to at least four limitations. First, death rates might be underestimated. Because multiple cause-of-death data were used in this analysis, other causes of death (e.g., kidney disease and heart disease) might have been listed as the underlying cause of death rather than SLE. An additional 17,450 persons who died during 1979--1998 had SLE listed as an associated cause of death on their death certificates. Second, SLE can be difficult to diagnose clinically, and both underdiagnosis and overdiagnosis (e.g., because of positive antinuclear antibody tests) occur (6). However, physicians reporting SLE as the underlying cause of death presumably had sufficient data supporting the diagnosis to cite SLE first instead of other causes. Third, rates for racial/ethnic populations other than white and black were not calculated because numbers were too small for meaningful analysis. These populations might have high rates of SLE (7). Finally, because prevalence estimates for SLE are variable, population death rates were calculated rather than case fatality rates. Arthritis and other rheumatic conditions are highly prevalent, disabling, and costly (8). SLE accounts for 14.5% of all deaths from arthritis (CDC, unpublished data, 1997) and represents one of these conditions that has premature mortality; approximately one third of deaths from SLE occur among persons aged <45 years. Of all deaths from arthritis, SLE accounts for 44.0% of deaths among persons aged <45 years (CDC, unpublished data, 1997). Because of SLE's protean manifestations, preventing excess and premature deaths will require clinical suspicion of the diagnosis, early recognition, appropriate therapeutic management, compliance with treatment, and improved treatment of long-term consequences (e.g., renal disease or accelerated atherosclerosis) (9). One of the public health strategies outlined in The National Arthritis Action Plan (8) is to better define issues related to rheumatic conditions such as SLE. Because further research into the causes of the marked age-, sex-, and race-specific disparities in death rates and temporal changes in death rates is necessary, CDC plans to develop a large population-based registry of SLE to monitor trends in SLE incidence and prevalence and better characterize persons with this disease. Studies conducted from this registry will examine why disparities and death rates exist and how mortality from SLE can be reduced. References
Table 1 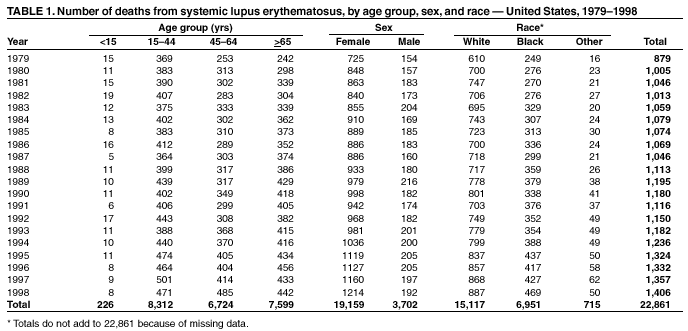 Return to top. Figure 1 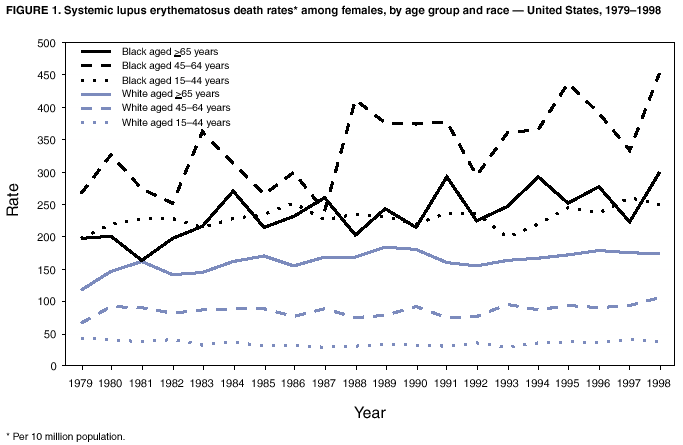 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 5/2/2002 |
|||||||||
This page last reviewed 5/2/2002
|