 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Emergency Medical System Responses to Suicide-Related Calls --- Maine, November 1999--October 2000Suicidal acts are morbid and potentially lethal events that are risks for subsequent completed suicide and possibly other health problems (e.g., substance abuse and depression) (1,2). Suicidal behavior also can have negative consequences on family members, friends, and caregivers (3). In 1996, the cost of health care and lost wages for suicide attempts in Maine was approximately $115 million (4). In 1999, a total of 1,079 persons were hospitalized in Maine for self-injurious behavior. Although Maine has no injury-related surveillance systems, the Maine Bureau of Health (MBOH) assessed the use of Emergency Medical Service (EMS) response data to estimate incidence of EMS responses to suicide-related calls in Maine and to summarize the distribution of these responses by patient and event characteristics. This report describes EMS suicide-related responses during November 1999--October 2000 and indicates that EMS data would be a useful component of an integrated statewide suicidal behavior surveillance system. Maine EMS responders complete a run report form (RRF) for each emergency assistance call. RRF contains a check box titled "concern suicide," which is selected "for patients who have, relevant to this call/run, expressed or displayed any suicidal tendencies or attempts." For any RRF on which "concern suicide" is selected, personal identifiers are removed and the form is sent to the MBOH Injury Prevention Program (MIPP). RRF has defined fields for sex, age, date of birth, incident date, incident location, incident site*, town of residence, insurance payor, and EMS service number. EMS responders can provide additional information in a free text field, from which MIPP extracts data on method of attempt or threat and circumstances surrounding the event. Inclusion criteria for this analysis were 1) "concern suicide" box checked on the RRF, 2) confirmed Maine residency, 3) aged >10 years†, and 4) presence of a unique RRF number. If RRFs were duplicated, only one was counted as a case. Of the 2,152 RRFs received during November 1999--October 2000, a total of 2,036 (95%) were eligible for inclusion in the analysis, of which 967 (47.5%) were made for the intra- or interinstitutional transportation of suicidal residents from nursing homes, psychiatric, correctional, or medical facilities§. Data were evaluated separately for all responses and for the 1,069 noninstitutional (NI) responses. All age-adjusted rates were standardized to the 2000 U.S. standard population and included both completed suicides and nonlethal attempts. For all calls, age-adjusted EMS response rates to "concern suicide" in Maine were 179.2 per 100,000 females and 142.3 per 100,000 for males. For females, age-specific rates were highest among those aged 15--19 years (384.8); for males, rates were highest for those aged 20--24 year (258.1). Because geographic and event data are limited for the institutionalized subgroup, the remainder of the descriptive analysis was limited to the NI cases. For the 1,069 NI cases, age-adjusted EMS response rates were 92.5 and 76.5 among females and males, respectively. Female rates of suicide-related EMS calls were highest among those aged 15--19 years (206.2), but were generally high among females aged 20--44 years (range: 138.8--160.2). Male rates of suicide-related EMS calls were highest among those aged 20--24 years (170.3) and high among those aged 15--19 and 25--34 years (range: 96.0--110.4). Age-specific rates were statistically similar for females aged 20--34 years and >55 years and for males aged 25--54 years. All other age-specific rate differences were statistically significant (p < 0.05). In comparison, suicide completion rates (derived from medical examiner data) were uniform across all female age groups (range: 0--10.7) and were highest among males aged >45 years (range: 25.0--34.8) (Figure 1). Among the 1,069 NI responses, 761 (72.0%) were to the residence of the attempter. EMS calls were most frequent in the summer (27.1%) and least frequent in the winter and spring (23.5% and 23.3%, respectively). Among the 963 (90.1%) NI cases for which method was documented, overdose (29.9%), "suicidal ideation only" (27.0%), and laceration (17.7%) were the most commonly documented methods. Attempts with firearms comprised 3.7%. The case-fatality ratio for EMS calls was 3.8% (1.3% for females and 6.9% for males). Case-fatality ratios were highest among males aged >65 years (15.2%). Method employed also was related to fatality ratios, even in the minority of completions¶ receiving EMS response. Of the 36 EMS responses to firearm-related suicidal behavior, 21 (58.3%) were lethal by the time of RRF completion. Compared with drug overdoses (1.0% lethal), attempts by firearm and hanging receiving EMS response were 58 and 60 times more lethal, respectively. Of the 1,069 events, circumstance was reported for 636 (59.5%); a total of 695 circumstances were reported. The most commonly reported circumstances were drug/substance abuse at the time of the incident (220 [31.7%] of all reported circumstances), patient-reported psychiatric illness (200 [28.8%]), domestic discord or violence (117 [16.8%]), and medical illness/pain (49 [7.1%]). Reported by: N Sonnenfeld, Div of Community Health, Maine Bureau of Health; D Bailey, C DiCara, Injury Prevention Program; J Bradshaw, Maine Emergency Medical Svc. A Crosby, MD, Div of Violence Prevention, National Center for Injury Prevention and Control; K Askland, MD, EIS Officer, CDC. Editorial Note:Among all states, Maine ranks 14th in rate of suicide deaths (13.4 per 100,000 population); this rate is 25% higher than the national rate (5). Despite the magnitude of the problem, no surveillance system exists in Maine to monitor suicidal behavior. The findings in this report indicate that EMS NI responses to suicide-related calls in Maine identified characteristics similar to those in community- and population-based studies of nonlethal suicidal behaviors (6--8) and might be an important component of a suicide surveillance system. Virtually all (99%) EMS response data in Maine from state-, municipal-, volunteer-, and fire-department--based and private services are compiled in a centralized database. In addition, Maine is developing an electronic reporting form and a mobile data input system for use across all 141 EMS services. The findings in this report are similar to other population- and community-based studies of the distribution of injuries associated with nonfatal suicidal behavior. Findings were similar for age, sex, location, method, and circumstances of suicide-related injuries. Other findings, such as seasonality of the suicidal act and a description of the institutionalized population, might be important for prevention efforts and require further analysis. Although this approach demonstrates the value of existing EMS response data for injury surveillance, the findings are subject to several limitations. First, no systematic mechanism exists to ensure that only one RRF is filed for each event or for systematically identifying repeat attempters. Second, the dataset contains only those events for which an RRF is completed. Many persons who contemplate or attempt suicide will not seek assistance and no surveillance instrument, except possibly population-based surveys, will detect these events (1). Despite the lack of prevalence data, demographic and event characteristic profiles parallel those previously documented (1,6--9). Moreover, incidence estimates (i.e., estimates of the total societal burden of attempts) may be most valuable in determining health services needs. Third, because unique record linkages with other health service data systems cannot currently be made, the sensitivity of EMS data, even to those who will eventually visit the emergency department or be admitted to the hospital, is unknown. Finally, this analysis includes data for only 12 months; as a result, the sample size is relatively small, which precludes description of temporal trends over several years. However, analysis at the early stage of development provides opportunities for improving the data collection system and preparing for its use in public health surveillance. Prevention of suicidal behaviors and attempts might preclude more life-threatening health problems (1). EMS data provide information about suicidal acts and might be useful in early prevention efforts. In addition, EMS data provide event detail unavailable in other health information systems. Data about the circumstances surrounding violent injuries are critical to understand attempt risk and to develop age- and sex-specific prevention strategies. Although refinements are needed, EMS data, together with medical examiner, hospital discharge, and emergency department data, would be a useful component of an integrated statewide suicidal behavior surveillance system (10). References
* Location is town and state of the incident; site is the type of location (e.g., home, office, school, or highway). † Age cutoff was set at age 10 years because only three RRFs were submitted for children aged <10 years, and suicidal behavior in this age group is sufficiently different than the 10--14 year age group to make comparing them problematic. § The current data entry system does not allow for distinctions between persons being transported from nursing homes and residential facilities versus from correctional facilities. ¶Medical examiner data for November 1999--October 2000 indicated 102 suicides completed by firearm. Therefore, 66 (65%) of firearm-related suicides were completed without an EMS response. Figure 1 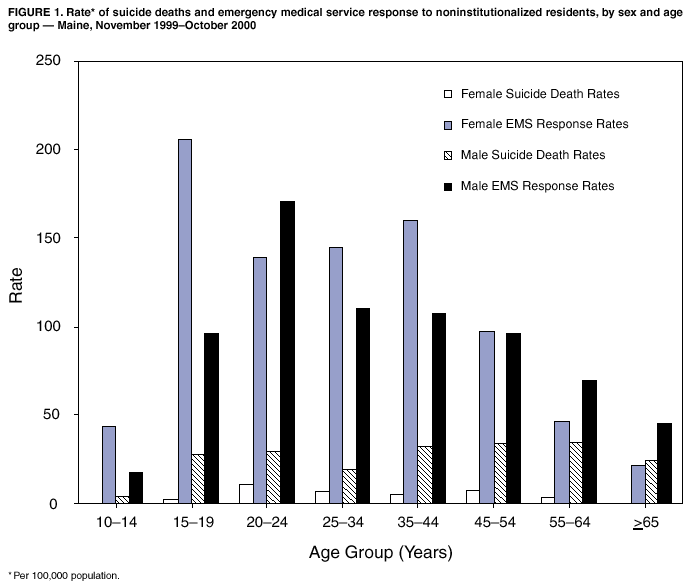 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/24/2002 |
|||||||||
This page last reviewed 1/24/2002
|