 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Rapid Assessment of Injuries Among Survivors of the Terrorist Attack on the World Trade Center --- New York City, September 2001On September 11, 2001, a jet aircraft crashed into the north tower of the World Trade Center (WTC) in lower Manhattan. Minutes later, a second aircraft crashed into the south tower. The impact, fires, and subsequent collapse of the buildings resulted in the deaths of thousands of persons. The precise number and causes of deaths could not be assessed in the immediate aftermath of the attack; however, data were available on the frequency and type of injuries among survivors (Figure 1). In previous disasters, such information assisted in characterizing type and severity of injuries and the health-care services needed by survivors (1). To assess injuries and use of health-care services by survivors, the New York City Department of Health (NYCDOH) conducted a field investigation to review emergency department (ED) and inpatient medical records at the four hospitals closest to the crash site and a fifth hospital that served as a burn referral center. This report summarizes findings of that assessment, which indicated that the arrival of injured persons to this sample of hospitals began within minutes of the attack and peaked 2 to 3 hours later. Among 790 injured survivors treated within 48 hours, approximately 50% received care within 7 hours of the attack, most for inhalation or ocular injuries; 18% were hospitalized. Comprehensive surveillance of disaster-related health effects is an integral part of effective disaster planning and response. Within 6 hours of the WTC attack, a NYCDOH rapid assessment team began collecting demographic and clinical data on all persons who sought emergency care from 8 a.m. September 11 to 8 a.m. September 13 at the five Manhattan hospitals. Information about each person included sex, age, mode of arrival at the hospital, date and time of registration or initial assessment, type and anatomic location of injury or illness, whether the injury or illness was attributable to the attack, and whether the person was admitted for additional treatment or was discharged from the ED. Among the 1,688 ED patients who received care at the sampled hospitals during the assessment period, 1,103 (65%) were survivors treated for injuries or illnesses related to the attack. A link between injury or illness and the attack was not established for 96 (6%) patients because of incomplete documentation; specific injury or illness was missing for 161 (15%), and admission and discharge data were not documented for 108 (10%). The median age of 1,103 survivors was 39 years (range: <1--95 years), 729 (66%) were male, 282 (26%) arrived by emergency medical vehicle, and 320 (29%) were rescue workers (e.g., firefighters, police officers, and emergency medical services personnel). A total of 810 (73%) were treated and released from EDs, 181 (16%) were hospitalized for additional treatment, and four (0.4%) died during emergency care. Among the survivors, 152 (14%) had WTC-related noninjury conditions (e.g., cardiac, respiratory, neurologic, or psychiatric illness). Within 12 hours of the first crash, emergency care was sought by 511 (71%) of the 723 survivors with recorded injuries and time of assessment (Figure 2). The survivors with injuries requiring admission and additional treatment presented earlier than those treated and released. Approximately 50% of the survivors admitted for treatment presented within 4 hours of the event (interquartile range: 2.4--8.9 hours). In comparison, approximately 50% of the survivors treated and released from the ED presented within 7.6 hours (interquartile range: 3.5--15.3 hours). Rescue workers arrived later than other survivors and accounted for 59 (51%) of 115 survivors presenting to the EDs during the first 24--48 hours after the attack (Figure 2). Among 790 survivors with injuries, 386 (49%) had inhalation injuries and 204 (26%) had ocular injuries (Table 1). Most inhalation and ocular injuries were attributed to smoke, dust, debris, or fumes. A total of 443 (56%) survivors were treated for inhalation injury, ocular injury, or a combination of both without additional injuries. Among survivors hospitalized with injuries, 52 (37%) sustained inhalation injuries and 27 (19%) sustained burns. Most survivors with fractures (59%), burns (69%), closed head injuries (57%), or crush injuries (75%) were hospitalized for additional treatment. The injury pattern among rescue workers differed from the pattern among other survivors (Table 2). A significantly higher percentage of rescue workers sustained ocular injuries (39% versus 19%; p<0.0001), and a significantly lower percentage of rescue workers sustained burns (2% versus 6%; p<0.01). Reported by: Depts of Emergency Medicine and Medical Records, Bellevue Hospital Center, Beth Israel Medical Center, New York Weill Cornell Medical Center, St. Vincent's Medical Center, New York Downtown Hospital, New York, New York. B Boodram, MPH, L Torian, PhD, P Thomas, MD, S Wilt, MD, Integrated Surveillance Unit, New York City Dept of Health. D Pollock, MD, Div of Injury and Disability Outcomes and Programs, National Center for Injury Prevention and Control; M Bell, MD, Div of Healthcare Quality Promotion, National Center for Infectious Diseases; and D Budnitz, MD, EIS Officer, CDC. Editorial Note:Similar to injured survivors of other terrorist attacks on buildings, most survivors of the WTC incident sustained injuries that were treated on an outpatient basis (2,3). The hospital admission rate among survivors of the Murrah Federal building bombing in Oklahoma City, Oklahoma, was approximately 20% (2). However, admission rates associated with terrorist bombings should be compared with caution because the number at risk, the location of survivors at the time of the attack, and building and blast effects vary with each event. Inhalation and ocular injuries were diagnosed and treated more frequently following the WTC attack than the attacks in Oklahoma City and on the U.S. Marine barracks in Beirut, Lebanon (2,4). This difference might be the result of more extensive exposure to smoke and respirable dust after the WTC attack. Multicasualty disaster reports commonly describe a first wave of survivors with minor injuries, a second wave of more severely injured survivors, and subsequent waves of survivors rescued during extrication from the disaster site (5). This report describes one large wave of survivors and a second wave the next day largely comprising rescue workers. Few survivors were extricated from the WTC site, probably because of the limited number of survivable spaces left by the overwhelming forces of the collapse of the 110-story towers (2,6). The initial wave of rescue-worker injuries occurred while responding to the collapse of the upper floors the of the towers. Rescue workers who sought medical care at EDs the following day sustained injuries associated with fires, unstable rubble, sharp-edged building fragments, and exposure to smoke and respirable dust at the attack site. As part of rescue and recovery operations during the rapid assessment period, local, state, and federal agencies distributed protective eye, hand, foot, and respiratory gear and training on correct use. CDC distributed information on these topics through NYCDOH, including information on eye safety (http://www.cdc.gov/niosh/eyesafe.html), respiratory exposures (http://www.cdc.gov/niosh/erfaqs.html), general rescue site safety (http://www.cdc.gov/niosh/emhaz2.html), and respirator cleaning and reuse (http://www.cdc.gov/niosh/respcln.html). The findings in this report are subject to at least two limitations. First, the rapid assessment of the health effects of the WTC attack was a sample that did not encompass all injured survivors who sought emergency medical care near the crash site and did not provide population-based estimates of injury occurrence (1,2). Second, data describing injury circumstances, clinical conditions, treatments, and follow-up care were missing from many survivor records reviewed by the rapid assessment team. Some survivors were treated and released from temporary triage stations outside hospitals without documentation. Numerous survivors were treated by more distant hospitals in New York, New Jersey, and Connecticut, by private physicians, onsite triage stations, or they treated themselves. The rapid assessment of injuries among WTC attack survivors reinforces the need to strengthen capacity for postdisaster surveillance before disasters occur (7,8). Use of electronic data can improve timeliness of surveillance, and in October 2001, NYCDOH began an automated electronic surveillance system to monitor chief complaints reported in 29 area EDs. Standardized patient record keeping can improve completeness of point-of-care data collection and public health reporting. In North Carolina and Oregon, CDC pilot projects are using Data Elements for Emergency Department Systems (DEEDS), a set of recommended specifications for ED patient record systems (9). Improving ED record keeping and reporting systems will assist in the surveillance of disaster-related health effects and are an integral part of effective disaster planning and response (10). References
Table 1  Return to top. Figure 1  Return to top. Table 2 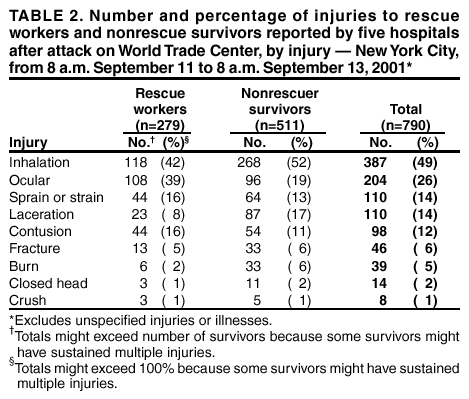 Return to top. Figure 2 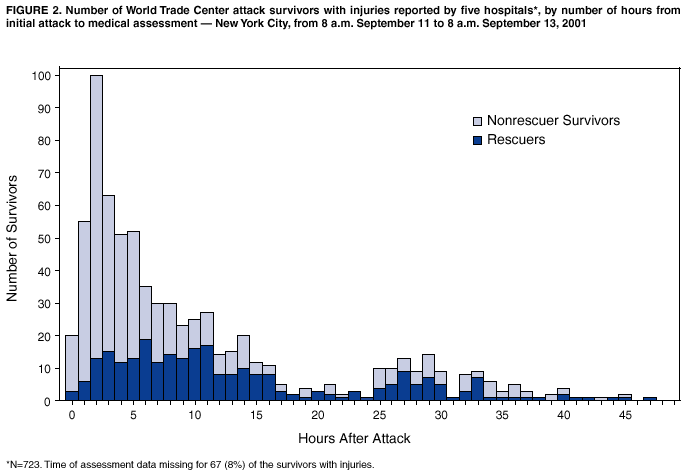 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 1/10/2002 |
|||||||||
This page last reviewed 1/10/2002
|