 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Methicillin-Resistant Staphylococcus aureus Skin or Soft Tissue Infections in a State Prison --- Mississippi, 2000On October 25, 2000, the Mississippi State Department of Health (MSDH) notified CDC that, since November 1999, 31 inmates had acquired methicillin-resistant Staphylococcus aureus (MRSA) skin or soft tissue infections at a state prison. During November 1998--October 1999, no MRSA infections had been reported at the prison, which houses approximately 1,200 female and 1,800 male inmates. This report summarizes the case investigation and the nasal culture prevalence survey conducted by MSDH and CDC during November 2000. Findings indicate that MRSA infections were transmitted person-to-person within the prison, and that the number of asymptomatic carriers was unexpectedly high for a nonhealth-care setting. Correctional facilities can reduce the increasing prevalence of MRSA disease by identifying and appropriately treating infected persons and by instituting prevention measures. A case of MRSA infection was defined as a skin or soft tissue lesion occurring in a state prison inmate with symptoms (e.g., pus, pain, warmth, or tenderness) and with MRSA cultured from the site of infection during November 1999--November 2000. Cases were identified by interviews with physicians and inmates and a review of the prison's medical, laboratory, and pharmacy records. Fifty-nine inmates had an illness that met the case definition (Figure 1); 46 (78%) were women, and the median age was 33 years (range: 19--70 years). The median length of incarceration was 397 days (range: 3--3,717 days). Records of 45 (76%) infected inmates were reviewed. Three (7%) had been hospitalized during the year preceding infection. Twenty-six (58%) had infections on the legs and seven (16%) on the arms. Fifteen (33%) were diagnosed with furuncles, 12 (27%) with skin abscesses, and 11 (24%) with open wounds; 21 (47%) had cellulitis, and two (4%) had systemic infections requiring hospitalization. Infections resolved after a median of 3 weeks (range: 1--36 weeks). Systemic antimicrobials were used to treat 44 (98%) infected inmates, 35 (78%) received topical antimicrobials, six (13%) required incision and drainage, and wound dressing was prescribed for 21 (47%). Nineteen (90%) of the 21 infected inmates with wound dressings changed their dressings themselves. During interviews, 15 (33%) infected inmates reported helping or being helped by other inmates with wound care or dressing changes. Twenty-six (58%) reported lancing their own boils or other inmates' boils with fingernails or tweezers; 40 (89%) shared personal items (e.g., linen, pillows, clothing, and tweezers) that potentially were contaminated by wound drainage. To assess the extent of MRSA carriage among the inmates, swab specimens of both anterior nares were collected from all female and a one third systematic sample of male inmates. Of 1,757 inmates sampled, 86 (4.9%) were MRSA carriers. More women (73 of 1,241 [5.9%]) were carriers than men (13 of 516 [2.5%]) (p=0.003), and inmates who had been incarcerated for >60 days were more likely to be carriers (84 of 1,565 [5.4%]) than those who had served less time (one of 142 [0.7%]) (p=0.01). Of the 59 infection-associated isolates, 41 (69%) were tested and genotyped at CDC. All 41 isolates were confirmed as MRSA and 40 (98%) were susceptible to gentamicin, rifampin, trimethoprim-sulfamethoxazole, clindamycin, vancomycin, and chloramphenicol; three (7%) were resistant to levofloxacin. Pulsed-field gel electrophoresis of isolates revealed that three MRSA strains predominated: genotype A (24 [59%]), genotype B (seven [17%]), and genotype C (four [10%]). During December 2000, CDC and MSDH provided the Mississippi State Department of Corrections and the prison with control measures such as optimizing antimicrobial treatment of infected inmates, reinforcing infection control practices (e.g., implementing Standard Precautions [1] at prison clinics, educating inmates in personal hygiene and wound care), using antibacterial soap, and establishing an MRSA skin infection surveillance system. Reported by: R Culpepper, MD, R Nolan, MD, S Chapman, MD, Univ of Mississippi Medical Center, Jackson; A Kennedy, MPH, M Currier, MD, State Epidemiologist, Mississippi State Dept of Health. Div of Healthcare Quality Promotion, National Center for Infectious Diseases; and an EIS Officer, CDC. Editorial Note:S. aureus is an important and common pathogen in humans. It is found in the nose or on the skin of many healthy, asymptomatic persons (i.e., carriers) and can cause infections with clinical manifestations ranging from pustules to sepsis and death. Most transmission occurs through the contaminated hands of a person infected with or carrying S. aureus. MRSA infections frequently are encountered in health-care settings (2). Since the 1960s, treatment of these infections has become more difficult because S. aureus has progressively acquired resistance to previously effective antimicrobial agents (2). In 1999, 2,538 (53.5%) of 4,744 intensive care unit patients with hospital-acquired S. aureus-associated infection had MRSA (3). Less information is available on long-term--care facilities, where prevalence of MRSA carriage may range from zero to 33% of the residents (4). Risk factors for infection with MRSA in health-care settings include prolonged hospital stay, exposure to multiple or prolonged broad-spectrum antimicrobial therapy, stay in an intensive care or burn unit, proximity to patients colonized or infected with MRSA, use of invasive devices, surgical procedures, underlying illnesses, and MRSA nasal carriage (5). Although community-onset MRSA infections have been reported recently (6), little is known about their epidemiology or prevalence of carriage. Community outbreaks have occurred among injection-drug users; aboriginals in Canada, New Zealand, and Australia; Native Americans/Alaska Natives in the United States; and players of close-contact sports (6). Reported most commonly have been uncomplicated skin infections; however, community-acquired MRSA infections can be severe. Four deaths from community-acquired MRSA in children were reported in Minnesota and North Dakota in 1999 (7). Disease transmission can occur easily among inmates at correctional facilities. In 1999, approximately two million persons were incarcerated in the United States (8). Skin or soft tissue infections are recognized problems in these facilities (9). MRSA disease in prisons can be controlled or prevented using several approaches. First, severe skin disease or treatment failures of presumed S. aureus skin infection should be evaluated with appropriate cultures or other diagnostic tests. Efforts to monitor the etiology of skin disease should be linked to these data to determine whether MRSA is a problem in the facility. MRSA outbreaks can be reported to CDC (telephone [800] 893-0485) through state departments of corrections and state health departments. Second, optimal treatment of MRSA disease should be based on the infecting organism's antimicrobial susceptibility result and, when available, input by infectious disease expertise. Third, close contact among inmates may place them at increased risk for transmission of skin-colonizing or skin-infecting organisms. To prevent skin disease, all inmates should practice good personal hygiene, including daily showers. Inmates should avoid touching wounds or drainage of others and should have access to sinks and plain soap (in this setting, the usefulness of antibacterial soap is unknown). Hands should be washed with soap as soon as possible after touching wounds or dressings. Personnel that provide wound care should follow Standard Precautions (1). References
Figure 1 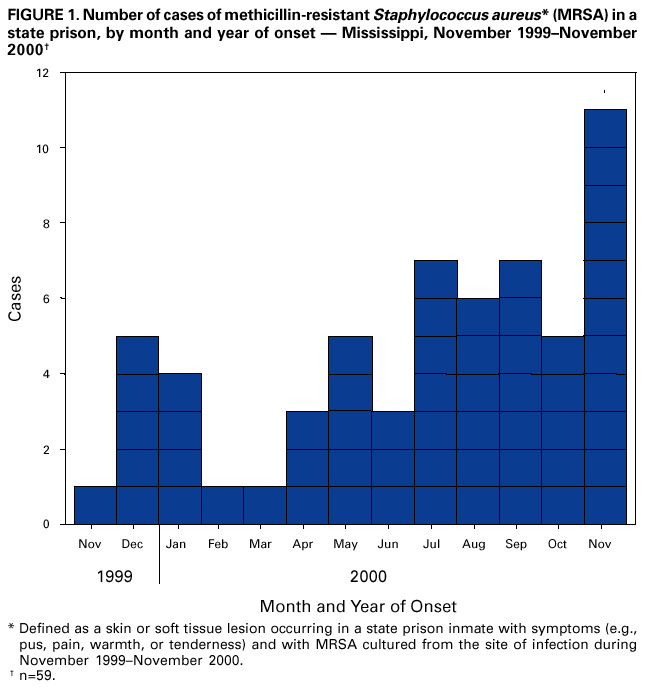 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/26/2001 |
|||||||||
This page last reviewed 10/26/2001
|