 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Botulism Outbreak Associated With Eating Fermented Food ---Alaska, 2001On January 18, 2001, the Alaska Division of Public Health was informed by a local physician of a possible botulism outbreak in a southwest Alaska village. This report summarizes the findings of the outbreak investigation, which linked disease to eating fermented food, and describes a new botulism prevention program in Alaska. A case of foodborne botulism was defined as a clinically compatible illness in a village resident with laboratory confirmation of botulism or a history of eating the same food as a laboratory-confirmed case; 14 persons in the village had eaten fermented beaver tail and paw on January 17. Approximately 20 hours later, three of the 14 had symptoms suggestive of botulism, including dry mouth, blurry vision, and general weakness. Two patients developed respiratory failure and required intubation and mechanical ventilation. One of the two intubated patients suffered cardiac arrest and underwent successful cardiopulmonary resuscitation. Approximately 6 hours after the onset of symptoms, the three patients received types A/B and E botulism antitoxin. They subsequently were evacuated to an intensive care unit (ICU) in Anchorage. Two patients recovered without further complication. The third required tracheostomy tube placement and mechanical ventilation for 1 month; this patient had been hospitalized with botulism in 1997. Of the other 11 exposed persons, four reported minor symptoms compatible with botulism, including dry mouth and nausea, and were admitted to a hospital for overnight observation. One was hospitalized for 10 days with persistent ileus. The remaining seven exposed persons were held for observation for 48 hours. Clinical specimens from the 14 exposed persons were tested for botulinum toxin at CDC. Type E toxin was detected in serum specimens from two of the ICU patients and in stool from the third. Although they displayed minor symptoms, the other 11 persons had no toxin found in specimens and were not considered laboratory-confirmed cases. Type E toxin also was detected in three beaver paws tested from the implicated meal. Beaver is hunted in southwest Alaska, and certain parts often are fermented and eaten later. In this outbreak, the tail and paws had been wrapped in a paper rice sack and stored for up to 3 months in the entry of a patient's house. Some of the beaver tail and paw had been added to the sack as recently as 1 week before it was eaten. Reported by: A Horn, K Stamper, D Dahlberg, J McCabe, MD, Bristol Bay Area Health Corporation, Dillingham; M Beller, MD, JP Middaugh, MD, State Epidemiologist, Alaska Dept of Health and Social Svcs. Arctic Investigations Program; Foodborne and Diarrheal Diseases Br, Div of Bacterial and Mycotic Diseases, National Center for Infectious Diseases; and EIS officers, CDC. Editorial Note:This report illustrates how the use of nontraditional fermentation methods is associated with foodborne botulism in Alaska. Botulism results from eating preformed toxin produced by Clostridium botulinum. Botulism begins with cranial nerve paralysis, including diplopia, dilated and fixed pupils, dysarthria, dysphagia, and dry throat. Botulism intoxication can result in death, which most often is caused by respiratory failure. The latent period is typically 12--36 hours but can range from 6 hours to 10 days (1). C. botulinum and closely related organisms produce toxins designated as types A, B, C, D, E, F, and G. Human botulism is most commonly caused by types A, B, and E. Type E is associated with foods of marine or freshwater origin. Alaska's foodborne botulism rates exceed those in any other state and are among the highest in the world (1). During 1950--2000, Alaska recorded 226 cases of foodborne botulism from 114 outbreaks. All patients were Alaska Natives, and all cases with known causes were associated with eating fermented foods (1,2). Approximately 27% of U.S. foodborne botulism cases occur in Alaska. In traditional fermentation, food is kept in a grass-lined hole in the ground or a wooden barrel sunken into the ground or is placed in a shady area above ground for several weeks to months. Since the 1970s, however, plastic or glass containers have been used and fermentation has been done above ground or indoors. The anaerobic condition of sealed containers and warmer temperatures make fermentation more rapid and production of botulism toxin more likely (3--5). These nontraditional methods have been associated with increased botulism rates in Alaska during 1970--1989 (Figure 1) (4,5). Although a plastic container was not used in this outbreak, the beaver tail and paw were fermented in a closed rice sack and stored in a warm area. Early diagnosis and antitoxin treatment have contributed to the decline of the case-fatality rate from approximately 31% during 1950--1959 to no deaths in Alaska since 1994 (1). However, Alaska continues to have high foodborne botulism rates because fermented foods are part of Alaska Native culture. In a 1999 survey, 107 (77%) of 140 Alaska Natives reported having eaten fermented foods at least once in their lifetime (3). In 1998, the Bristol Bay Area Health Corporation, a health-care delivery organization operated by Alaska Natives in southwest Alaska, collaborated with CDC's Arctic Investigations Program to design a community-based botulism prevention strategy, including an education video entitled, "A Helping Hand: Keeping Your Family Safe From Botulism." It features Alaska Native elders and botulism survivors discussing the risks of eating improperly fermented foods and recommends returning to traditional methods. The video also suggests boiling fermented foods for 10 minutes to destroy botulinum toxin. Both an English and an Alaska Native language version of the video were produced and distributed to all village clinics and schools in the Bristol Bay region. Information on botulism prevention also is available at http://www.cdc.gov/phtn/botulism/default/default.htm. References
Figure 1 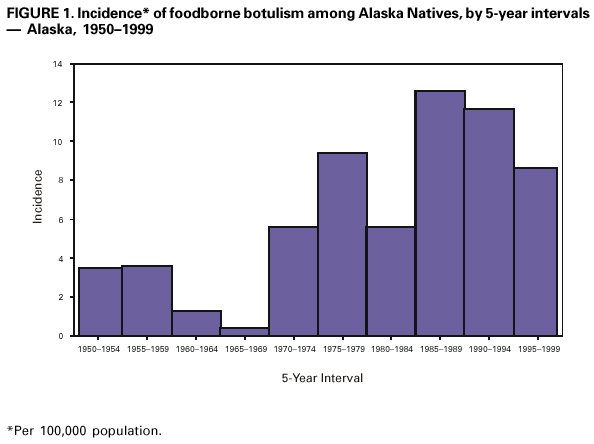 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 8/24/2001 |
|||||||||
This page last reviewed 8/24/2001
|