 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Prevalence of Arthritis --- United States, 1997Arthritis and other rheumatic conditions (i.e., arthritis) are among the most prevalent diseases in the United States (1) and the most frequent cause of disability (2). In 1985, an estimated 35 million persons were affected by arthritis (3); in 1990 (1), a study using a broader arthritis definition estimated that 38 million were affected. To better characterize these conditions, CDC analyzed a variety of data for 1997 using common definitions from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The findings of one such analysis in the National Health Interview Survey (NHIS) indicated that, in 1997, the prevalence of persons with arthritis had increased by approximately 750,000 per year since 1990. Findings also support earlier projections that by 2020, 60 million persons may be affected by arthritis and that the activities of 11.6 million persons may be limited by arthritis (1). More widespread implementation of existing interventions may reduce the occurrence and progression of arthritis. Prevalence rates were estimated from NHIS, a probability sample of the civilian, noninstitutionalized population in the United States (1). Data from the 1994--1995 NHIS, the most recent surveys using ICD-9 codes for health conditions, were used to estimate the 1997 prevalence and physical activity limitations from arthritis. Estimates of arthritis prevalence rates were derived from a random sample of 36,057 (16.7%) of 218,646 respondents who were asked about the presence during the 12 months preceding the survey of any of various musculoskeletal conditions and for details of these conditions. Each condition reported was assigned an ICD-9 code. Respondents with one or more codes recommended by the National Arthritis Data Workgroup (NADW) to represent arthritis* (1) were included in the analysis. Estimated rates of activity limitations attributed to arthritis were based on responses from 218,646 respondents who were asked whether they were limited in or prevented from working, housekeeping, or performing other activities as a result of a health condition(s) and, if so, did they attribute the limitation to arthritis. To determine the number of persons affected or limited by arthritis, age- and sex-specific prevalence rates were calculated for the civilian, noninstitutionalized population, the referent population for NHIS, and were applied to the estimated 1997 U.S. population (4) by age and sex. Rates of disease burden for the total population were generated by totaling the age- and sex-specific estimates; 95% confidence intervals were calculated using SUDAAN to account for NHIS's complex survey design. Results of these analyses indicated that an estimated 43 million persons had arthritis in 1997. All age groups were affected, including the working-age population, and rates increased with age. Females had higher arthritis rates than males overall and for each age group (Table 1). An estimated eight million persons (3% of the U.S. population) reported arthritis as a major or contributing cause of activity limitations (Table 1). Rates increased with age and females had higher rates of activity limitations than males overall and for each age group (Table 1). Reported by: Health Care and Aging Studies Br, Div of Adult and Community Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. Editorial Note:The findings in this report indicate that from 1990 to 1997, the prevalence of persons with arthritis and with activity limitations from arthritis increased substantially. Related analyses have documented 744,000 hospitalizations and 44 million ambulatory-care visits for arthritis in 1997 (5). NADW's definition of arthritis aims to include specific conditions that would be understood as arthritis (e.g., systemic lupus erythematosus, infectious arthritis, and carpal tunnel syndrome). Because many persons with arthritis may not consult a physician for their condition (6), NHIS self-reported data may provide a more accurate estimate of the prevalence and impact of arthritis than medical encounter-based data. In addition, the data allow an understanding of the time trends in arthritis because the case definitions and survey methods are the same as the 1990 estimates (1). The findings in this study are subject to at least four limitations. First, the estimates used self-reported data that were not confirmed by a physician. Second, to estimate the total burden of disease, the analysis used rates based on surveys of the civilian, noninstitutionalized population, which represents 98% of the total U.S. population but excluded certain groups (e.g., the institutionalized elderly) that are likely to have different rates. Third, data used intercensal projections for denominators; these projected denominators may be inaccurate. Finally, rate estimates were assumed unchanged from 1995 to 1997; however, this may be reasonable because age- and sex-specific prevalence rates were virtually unchanged from 1990 (1). Further studies are needed to define the prevalence of specific types of arthritis, to provide direct measures of arthritis prevalence, to determine the financial and societal impact of arthritis, and to quantify the impact of arthritis at the state level and in health-care systems. Future analyses of NHIS data will need to accommodate the change from ICD-9--based code assignment of conditions to a symptom-based approach to the case definition of arthritis. Interventions are available that may reduce the occurrence and progression of arthritis. Measures to reduce obesity and avoid occupational and sports injuries can be expected to reduce the risk for osteoarthritis of the knees (7). Other interventions include supervised exercise programs, weight loss, and self-education courses such as the Arthritis Self-Help Course, which has been shown to reduce pain and physician visits (8). Unless such interventions are implemented quickly and widely, national projections suggest that arthritis will become a larger public health problem (1). Health-care providers, policymakers, and the public health community need to plan for the impact of this growth. CDC funds 37 state health departments to develop or enhance prevention programs and to identify new approaches to improving the quality of life for persons affected by arthritis (9). References
* Codes 95.6, 95.7, 98.5, 99.3, 136.1, 274, 277.2, 287.0, 344.6, 353.0, 354.0, 355.5, 357.1, 390, 391, 437.4, 443, 446, 447.6, 696.0, 710--716, 719.0, 719.2--719.9, 720--721, 725--727, 728.0--728.3, 728.6--728.9, 729.0--729.1, and 729.4. Table 1 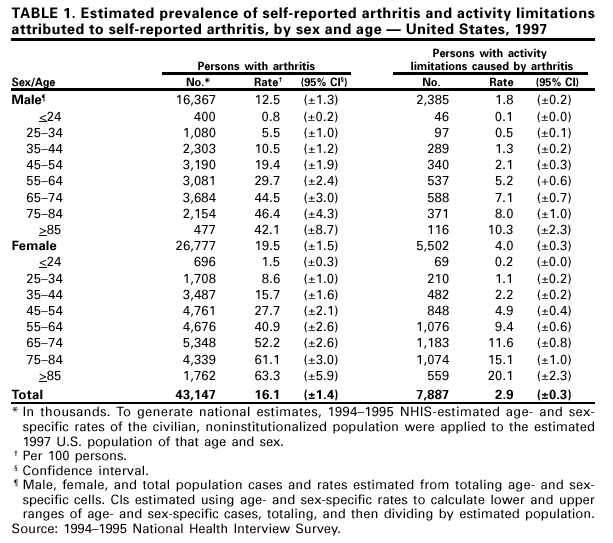 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 5/3/2001 |
|||||||||
This page last reviewed 5/3/2001
|