 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Palmar Pallor as an Indicator for Anthelminthic Treatment Among Ill Children Aged 2-4 Years -- Western Kenya, 1998Infections with the soil-transmitted intestinal helminths (i.e., Ascaris lumbricoides, Trichuris trichiura, and hookworm), estimated to affect approximately 1 billion persons, are among the most common and widespread human infections (1). Among children aged <5 years, intestinal helminth infections cause malnutrition and anemia, two important causes of mortality. Anthelminthic treatment (deworming) improves nutritional status of school-aged children (1). The World Health Organization and the United Nations Children's Fund (UNICEF) have developed guidelines that include interventions for anemia and malnutrition (2) in the integrated management of childhood illness (IMCI) for Immunization Registries -- Continued children aged <5 years seen at first-level health-care facilities in developing countries. Under the IMCI guidelines, in geographic areas where hookworm or Trichuris infections are endemic, children aged 2-4 years with palmar pallor are treated with an anthelminthic drug. This report summarizes an investigation of the use of palmar pallor as an indication for anthelminthic treatment among ill children aged 2-4 years seen at first-level health-care facilities in rural western Kenya; the investigation found that palmar pallor was associated with anemia but not with intestinal helminth infection. Children eligible for enrollment in the investigation were aged 2-4 years and seen for the first consultation for an illness during July 13-August 12, 1998, in three rural government health-care facilities in Bungoma District, Kenya. Enrollment criteria included caretaker consent, absence of a severe illness requiring referral, and no reported anthelminthic treatment during the 6 months preceding the investigation based on an interview with the caretaker. Each child was examined using IMCI guidelines, and a standard questionnaire was used to collect demographic, socioeconomic, and clinical information. Hemoglobin (Hb) levels were measured from a capillary finger-stick blood specimen using a hemoglobin photometer. Blood smears were examined for malaria parasites. Stool samples were processed using a formal-ethyl-acetate concentration technique (3). The intensity of helminth infection was measured by eggs per gram of stool and categorized as light, moderate, or heavy (3). Of the 633 eligible children, 574 (91%) were enrolled; 34 (5%) children were excluded for receiving anthelminthic treatment during the 6 months before the investigation, 13 (2%) for the presence of a severe illness requiring referral, and 12 (2%) because the caretaker refused to participate. Excluded and enrolled children had similar demographic and socioeconomic characteristics. The participants' median age was 37 months (range: 24-59 months); 319 (56%) were boys. A total of 191 (33%) children had palmar pallor, 351 (61%) children had anemia (Hb: <11 gm/dL; normal: 11-16 gm/dL), 329 (57%) had malaria parasitemia, 32 (6%) were infected with Ascaris, 34 (6%) were infected with hookworm, and five (1%) were infected with Trichuris; 66 (12%) children had one or more intestinal helminths. The prevalence of helminth infection was 10% among children aged 2 years, 11% among children aged 3 years, and 16% among children aged 4 years. All Trichuris infections, 97% of hookworm infections, and 78% of Ascaris infections were of light intensity. The sensitivity, specificity, and positive predictive value (PPV) of palmar pallor as an indicator for anemia were 50%, 93%, and 92%, respectively. Palmar pallor was associated with anemia (prevalence ratio [PR]=2.0; 95% confidence interval [CI]=1.8-2.3); however, no association was found between palmar pallor and helminth infection (Table 1). The sensitivity, specificity, and PPV of palmar pallor for identifying children with helminth infections were 27%, 66%, and 9%, respectively. Although malaria parasitemia modified the association between palmar pallor and helminth infection, the sensitivity and PPV of palmar pallor as an indicator for helminth infections in this geographic area remained low in children with or without malaria parasitemia. In the IMCI guidelines, the anthelminthic treatment is specifically for anemia; however, no association was found between palmar pallor and hookworm or Trichuris infection (PR=0.9; 95% CI=0.5-1.8). The sensitivity, specificity, and PPV of palmar pallor for identifying children with hookworm or Trichuris infection were 32%, 67%, and 6%, respectively. Reported by: CN Wamae, Kenya Medical Research Institute; J Mwanza, S Makama, Ministry of Health, Nairobi, Kenya. International Child Survival and Emerging Infections Program Support Activity and Epidemiology Br, Div of Parasitic Diseases, National Center for Infectious Diseases; and an EIS Officer, CDC. Editorial Note:The prevalence of intestinal helminth infection among a population of ill children aged 2-4 years who resided in Bungoma District, Kenya, was low and the infections identified were of low intensity. Findings of the few prevalence studies of intestinal helminth infection among healthy preschool-aged children in tropical areas are higher, ranging from 25% to 90% (4-7). The prevalence of intestinal helminth infections among healthy children aged 4-5 years in Kisumu District, western Kenya, was 60% (7) compared with 16% among children aged 4 years seen for outpatient care in Bungoma District; therefore, wide variation may exist in the prevalence of helminth infections within proximate geographic areas. These differences may be environmental (e.g., Kisumu and Bungoma districts are only 62 miles [100 km] apart; however, Kisumu District is warmer and more humid than Bungoma District) or socioeconomic (e.g., the prevalence of Ascaris and Trichuris infections among school children living in overcrowded conditions in Colombo, Sri Lanka, was seven to 10 times higher than that among children attending rural schools approximately 20 miles [30 km] away) (8). The findings in this report indicate that palmar pallor was predictive of anemia but was not associated with helminth infections. Heavy hookworm infections consistently have been reported to be associated with anemia (9,10). The lack of association between palmar pallor and helminth infection in Bungoma District may be the result of the light intensity of hookworm infections; all but one hookworm infection was considered light. The findings in this report are subject to at least two limitations. First, children who participated in the study may not be representative of all ill children in Bungoma District. Second, the findings may not be generalizable beyond areas with low prevalence and intensity of helminth infections. Most children in Bungoma District with a helminth infection would not have received anthelminthic treatment, and few receiving anthelminthic treatment would have been infected with an intestinal helminth if palmar pallor were used to indicate anthelminthic treatment, as recommended in the IMCI guidelines. These guidelines have been introduced into approximately 60 developing countries; although implementing the guidelines provides a means for delivering the nutritional benefits of anthelminthic therapy to preschool-aged children, additional studies may help to determine under what conditions palmar pallor indicates the need for anthelminthic treatment. These studies should be conducted in areas with varying prevalences of intestinal helminth and malaria infections. References
Table 1 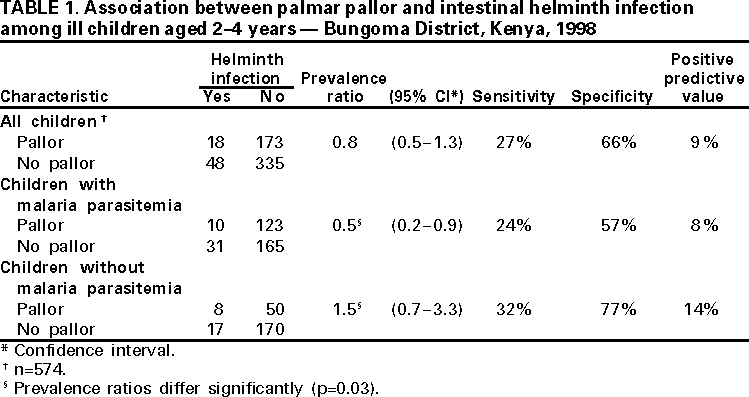 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 4/6/2000 |
|||||||||
This page last reviewed 5/2/01
|