 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Malaria Surveillance -- United States, 1995Holly Ann Williams, Ph.D.(1),(2); Jacqueline Roberts, M.S.(2); S. Patrick Kachur, M.D., M.P.H.(2); Ann M. Barber(2); Lawrence M. Barat, M.D., M.P.H.(2); Peter B. Bloland, D.V.M., M.P.V.M.(2); Trenton K. Ruebush II, M.D.(2); Elizabeth B. Wolfe, M.P.H.(2) 1 Epidemic Intelligence Service, Epidemiology Program Office, CDC 2 Division of Parasitic Diseases, National Center for Infectious Diseases, CDC Abstract Problem/Condition: Malaria is caused by four species of Plasmodium (i.e., P. falciparum, P. vivax, P. ovale, or P. malariae), which are transmitted by the bite of an infective female Anopheles sp. mosquito. Most malaria infections in the United States occur among persons who have traveled to areas with ongoing transmission. Occasionally, cases occur in the United States through exposure to infected blood products, by congenital transmission, or by local mosquito-borne transmission. Malaria surveillance is conducted to identify episodes of local transmission and to guide prevention recommendations for travelers. Reporting Period: Cases with onset of illness during 1995. Description of System: Malaria cases confirmed by blood smears are reported to local and/or state health departments by health-care providers and/or laboratory staff. Case investigations are conducted by local and/or state health departments, and reports are transmitted to CDC through the National Malaria Surveillance System (NMSS). Data from NMSS serve as the basis for this report. Results: CDC received reports of 1,167 cases of malaria with onset of symptoms during 1995 among persons in the United States or one of its territories. This number represents an increase of 15% from the 1,014 cases reported for 1994. P. vivax, P. falciparum, P. malariae, and P. ovale were identified in 48.2%, 38.6%, 3.9%, and 2.2% of cases, respectively. More than one species was present in three patients (0.3% of total). The infecting species was not determined in 80 (6.9%) cases. The number of reported malaria cases acquired in Africa (n=519) remained approximately the same as in 1994 (n=517); cases acquired in Asia increased by 32.4% (n=335); and cases acquired in the Americas increased by 37.4 % (n=246). Of 591 U.S. civilians who acquired malaria abroad, 15.6% had followed a chemoprophylactic drug regimen recommended by CDC for the area where they had traveled. Nine patients became infected in the United States. Of these nine cases, five were congenitally acquired; one was acquired by organ transplantation; and one was acquired by a blood transfusion. For two of the nine cases, the source of infection was unknown. Six deaths were attributed to malaria. Interpretation: The 15% increase in malaria cases in 1995 compared with 1994 resulted primarily from increases in cases acquired in Asia and the Americas, most notably a 100% increase in the number of cases reported from South America. This change could have resulted from local changes in disease transmission, travel patterns, reporting errors, or a decreased use of effective antimalarial chemoprophylaxis. In most reported cases, U.S. civilians who acquired infection abroad were not on an appropriate chemoprophylaxis regimen for the country where they acquired malaria. Actions Taken: Additional information was obtained concerning the six fatal cases and the nine infections acquired in the United States. Malaria prevention guidelines were updated and distributed to health-care providers. Persons traveling to a malarious area should take the recommended chemoprophylaxis regimen and use personal protection measures to prevent mosquito bites. Any person who has been to a malarious area and who subsequently develops a fever or influenza-like symptoms should seek medical care; investigation should include a blood smear for malaria. Malaria infections can be fatal if not diagnosed and treated promptly. Recommendations concerning prevention and treatment of malaria can be obtained from CDC. * INTRODUCTION Malaria is caused by infection with any of four species of Plasmodium (i.e., P. falciparum, P. vivax, P. ovale, and P. malariae) that can infect humans. The infection is transmitted by the bite of an infective female Anopheles sp. mosquito. Malaria infection remains a devastating global problem, with an estimated 300-500 million cases occurring annually. Forty-one percent of the world's population lives in areas where malaria is transmitted (e.g., parts of Africa, Asia, Central America, Hispaniola, North America, Oceania, and South America), and approximately 3 million persons die of malaria each year (1). In the past, malaria was also endemic throughout much of the continental United States; an estimated 600,000 cases occurred during 1914 (2). During the late 1940s, a combination of improved socioeconomic conditions, water management, vector-control efforts, and case management was successful at interrupting malaria transmission in the United States. Since then, malaria case sur- veillance has been maintained to detect locally acquired cases that could indicate the reintroduction of transmission and to monitor patterns of antimalarial drug resistance seen among U.S. travelers. Through 1995, most cases of malaria diagnosed in the United States have been imported from regions of the world where malaria transmission is known to occur. Each year, however, several congenital infections and infections resulting from exposure to blood or blood products are reported in the United States. In addition, several cases are reported that might have been acquired through local mosquito-borne transmission (3). State and/or local health departments and CDC thoroughly investigate all malaria cases presumed or known to be acquired in the United States, and CDC conducts an analysis of all imported cases to detect trends in acquisition. This information has been used to guide malaria prevention recommendations for travelers abroad. For example, an increase in P. falciparum malaria among U.S. travelers to Africa, an area with increasing chloroquine-resistance, prompted CDC in 1990 to change the recommended chemoprophylaxis from chloroquine to mefloquine (4). The signs and symptoms of malaria illness are variable, but most patients have fever. Other common symptoms include headache, back pain, chills, increased sweating, myalgia, nausea, vomiting, diarrhea, and cough. The diagnosis of malaria should be considered for any person who has these symptoms and has traveled to an area with known malaria transmission. Malaria should also be considered in the differential diagnosis of persons who have a fever of unknown origin, regardless of their travel history. Untreated P. falciparum infection can progress to coma, renal failure, pulmonary edema, and death. Asymptomatic parasitemia can occur among persons who have been long-term residents of malarious areas. This report summarizes malaria cases reported to CDC with onset of symptoms in 1995. METHODS Sources of Data Data regarding malaria cases are reported to both the National Malaria Surveillance System (NMSS) and the National Notifiable Diseases Surveillance System. Although both systems rely on passive reporting, the numbers of reported cases might differ because of differences in the collection and transmission of data and in the timing of case reports. In addition, NMSS receives more detailed clinical and epidemiologic data regarding each case (e.g., information concerning the area to which the infected person has traveled). Cases of blood-smear-confirmed malaria are identified by health-care providers and/or laboratories. Each slide-confirmed case is reported to local and/or state health departments and to CDC on a uniform case report form that contains clinical, laboratory, and epidemiologic information. CDC staff review all report forms at the time of receipt and request additional information if necessary (e.g., when no recent travel to a malarious country is reported). Reports of other cases are telephoned directly by health-care providers to CDC, usually when assistance with diagnosis or treatment is requested. All cases that have been acquired in the United States are investigated, including all induced and congenital cases and possible introduced or cryptic cases. Information derived from uniform case report forms is entered into a database and analyzed annually. Definition of Terms The following definitions are used in this report:
This report also uses terminology derived from the recommendations of the World Health Organization (5). Definitions of the following terms are included for reference.
Microscopic Diagnosis of Malaria The early diagnosis of malaria requires that physicians consider malaria in the differential diagnosis of every patient who has fever; the evaluation of such a patient should include taking a comprehensive travel history. If malaria is suspected, a Giemsa-stained smear of the patient's peripheral blood should be examined for parasites. Thick and thin blood smears must be prepared properly because the accuracy of diagnosis depends on the quality of the blood film and the experience of the laboratory personnel. ** (See Appendix for proper procedures necessary for accurately diagnosing malaria.) RESULTS General Surveillance During 1995, CDC received reports of 1,167 malaria cases that had onset of symptoms among persons in the United States and its territories, representing a 15% increase from the 1,014 cases reported for 1994 (6). This incidence is the largest number of reported cases since 1980 and includes the largest number of U.S. civilian cases ever reported (Table_1). Since 1988, with the exception of 1992, malaria among U.S. civilians has accounted for most of the cases reported to CDC. In 1995, 599 cases occurred in U.S. civilians compared with 524 cases reported for 1994 (Figure_1). The number of cases among residents of other countries increased from 370 cases to 461, whereas the number of cases among U.S. military personnel decreased from 38 in 1994 to 12 in 1995. For 95 cases, information was not available to determine whether the person was a civilian or in the military. Plasmodium Species The infecting species of Plasmodium was identified in 1,087 (93.1%) of the 1,167 cases in 1995. Of these 1,087 cases, P. vivax and P. falciparum were identified in blood smears from 48.2% and 38.6% of infected persons, respectively (Table_2). The 562 P. vivax cases reported for 1995 represented a 27.4% increase from the 441 cases in 1994, whereas the number of P. falciparum infections increased only slightly. Among cases in which the infecting species was identified, 71.9% of infections acquired in Africa were attributed to P. falciparum; 9.2% were attributed to P. vivax. The converse was true of malaria infections acquired in Asia and the Americas: 82% and 76.2% were attributed to P. vivax and only 8% and 16.7% were attributed to P. falciparum, respectively. Region of Acquisition and of Diagnosis *** The region or country of infection was known for 97.7% cases. Most of the imported cases (n=1,158) were acquired in Africa (44.8%) and the Indian subcontinent (24.8%). In Africa, the largest concentration of cases (n=360; 69.4%) came from countries in West Africa. The other regions where imported cases of malaria were acquired were Central America and Caribbean (18.5%), South East Asia (3%), South America (2.6%), Oceania (2.3%), Middle East (0.5%), and China (0.2%). Less than 1% (0.5%) of cases were acquired in an unknown country in Asia. South America reported a 100% increase in cases compared with 1994. In the United States, the five areas reporting the largest number of malaria cases were California (n=249), New York City (n=238), New York (n=86), Illinois (n=72), and Florida (n=65) (Figure_2). New York City, which began reporting cases to CDC in 1993, reported a 125% increase in cases in 1995 compared with 1994. This large increase in reported number of cases might be because of an increased rate of international travel, improved access to health care, or it might reflect an expanded surveillance system for New York City. Interval Between Arrival and Illness Of those persons who became ill with malaria after arriving in the United States, both the interval between arriving in the United States and onset of illness and the infecting Plasmodium species were known for 851 (72.9%) (Table_5). Symptoms began after arrival in the United States for 782 (92.2%) of these cases. Clinical malaria developed within 1 month after arrival in 292 (79.6%) of the 367 P. falciparum cases and in 154 (35.6%) of the 432 P. vivax cases with onset after return to the United States (Table_5). Only 25 (3.19%) of the 782 persons became ill greater than 1 year after returning to the United States. An additional 66 persons reported becoming ill before arriving in the United States. Imported Malaria Cases Imported Malaria in Military Personnel Twelve cases of imported malaria in U.S. military personnel were reported for 1995. Eight of these cases occurred among personnel of the U.S. Army; two cases, the U.S. Air Force; one case, the U.S. Marine Corps; and one case, the U.S. Navy. Of these 12 cases, two persons did not use any chemoprophylaxis. Imported Malaria in Civilians A total of 1,048 imported malaria cases were reported among civilians. Of these, 591 (56.4%) cases occurred in U.S. residents, and 457 (43.6%) cases occurred among residents of other countries (Table_6). Of the 591 imported malaria cases in U.S. civilians, 287 (48.6%) had been acquired in Africa, approximately the same number of cases reported in 1994. The Central American and Caribbean region accounted for 116 cases (19.6%) of imported malaria in U.S. citizens, whereas travel to the Indian subcontinent accounted for an additional 95 cases (16.1%). Of the 457 imported cases among residents of other countries, most cases were acquired in either Africa (n=177; 38.7%) or the Indian subcontinent (n=174; 38.1%). Use of Antimalarial Chemoprophylaxis Use of Chemoprophylaxis Among U.S. Residents. Information concerning use of chemoprophylaxis was known for 539 (91.2%) of the 591 U.S. residents who had imported malaria. Of these 539 persons, 307 (57%) had not taken chemoprophylaxis, and 148 (27.5%) had not taken a drug recommended by CDC for the area visited. Only 84 (15.6%) U.S. civilians had taken a medication recommended by CDC (7). Seventy-six of these patients had taken mefloquine weekly; one person had taken doxycycline daily; and seven who had traveled only in areas where chloroquine-resistant malaria has not been documented, had taken chloroquine weekly. Of the 148 persons taking a nonrecommended drug, 80 (54.1%) reported taking chloroquine during travel to an area where chloroquine resistance had been documented. Malaria Infection After Use of Recommended Prophylaxis. Ninety-three patients (84 U.S. civilians, 4 persons in the U.S. military, 4 foreigners, and 1 person whose information regarding his status was missing) developed malaria after taking a recommended antimalarial drug. Because of missing data, the length of time before symptom onset could not be determined for 13 (14%) of the 93 persons who reported taking appropriate prophylaxis. Cases of P. vivax or P. ovale. Of the 93 patients who developed malaria after use of recommended chemoprophylaxis, 56 cases (60.2%) were caused by P. vivax (n=49) or P. ovale (n=7). The malaria case surveillance report indicated that 13 (23.2%) of these patients were noncompliant with their antimalarials. Thirty-six cases of P. vivax or P. ovale occurred 46 days after arrival in the United States. These cases were consistent with relapsing infections and, thus, do not indicate prophylaxis failures. Because of insufficient information regarding eight cases of P. vivax and one case of P. ovale malaria, it could not be determined whether these cases were relapsing infections. Onset of symptoms in three cases of P. vivax began before the persons returned to the United States. Eight cases (seven cases of P. vivax and one case of P. ovale) occurred within 45 days after the patient returned to the United States. Of these cases, two patients were known to be noncompliant with the antimalarial chemoprophylaxis. Region of acquisition varied widely for the remaining six cases (five cases of P. vivax and one case of P. ovale), and no information was provided concerning serum drug levels for any of these patients. For these cases, sufficient data did not exist to indicate a new area of resistant P. vivax or P. ovale. The most likely explanations for these cases are either inappropriate dosing or noncompliance. The remaining 37 cases of malaria reported among persons who had taken a recommended antimalarial drug for chemoprophylaxis include 25 cases of P. falciparum, two cases of P. malariae, and one case of mixed P. vivax and P. falciparum infection. In nine cases, the infecting species was not identified. Cases of P. falciparum. Twenty-one of the 25 P. falciparum cases were from Africa. In 12 (48%) of these 25 cases, noncompliance with antimalarials was reported. The remaining 13 cases of P. falciparum that were acquired while the patient was reported to have used appropriate chemoprophylaxis varied in region of acquisition. Eleven cases were acquired in Africa (four in West Africa, four in East Africa, two in Central Africa, and one in an unknown African location) and two cases in Belize. Serum drug levels of the antimalarials were unavailable for these patients. For these cases, sufficient data did not exist to indicate new areas of resistant P. falciparum. The most likely explanations for these cases are either inappropriate dosing or noncompliance. Purpose of Travel. The purpose of travel to malarious areas was reported for 307 (51.9%) of the 591 U.S. civilians with imported malaria (Table_7). Of these 307 cases, the largest percentage (14%), teachers or students, had traveled to malarious areas; the second largest percentage (8.6%) of case-patients had traveled to visit a friend or relative. Malaria Acquired in the United States Congenital Malaria Five cases of congenitally acquired malaria were reported in 1995. Case 1. On October 22, 1995, following a normal pregnancy, a male infant was delivered by spontaneous vaginal delivery in New York. His mother had immigrated to the United States from Punjab State, India, 1 month before delivery. No information was known concerning whether she took antimalarial chemoprophylaxis or received malaria treatment during her pregnancy. Immediately after birth, the infant was admitted to the newborn intensive-care unit because of fever and evaluated for sepsis. He responded to antibiotics and was discharged 3 days after birth. On November 12, 1995, the infant was readmitted because of fever and cough. A sepsis evaluation indicated a bacterial urinary tract infection (ampicillin-sensitive enterococcus grew in culture). Despite appropriate intravenous antibiotic therapy, the infant remained febrile. The infant also demonstrated evidence of respiratory syncytial virus infection. By the fourth hospital day, intraerythrocytic parasites were detected on peripheral smear and diagnosed as P. vivax; reviews of earlier smears also indicated P. vivax. The patient rapidly defervesced on chloroquine and received a follow-up course of primaquine. He was discharged on November 21, 1995. Blood smears taken from the infant's mother (who was asymptomatic) were negative for malaria parasites. A serum sample tested by the immunoflourescent assay (IFA) technique indicated the following results: P. vivax 1:1024, P. falciparum 1:256, P. malariae 1:64, and P. ovale 1:64. The mother was treated with a standard course of chloroquine and primaquine. Case 2. A male infant was born in Texas prematurely on July 26, 1995, at 27 weeks' gestation. The delivery was complicated by preeclampsia and possible placenta abruptio. The mother had arrived from Zaire 2 months before delivery and reported being treated for malaria three times in the 6 months before departure. The infant required intubation at delivery; on the same day, his platelet count dropped to 15,000, and he received a platelet transfusion. He was also hyperbilirubinemic. One day after delivery, the infant was extubated; he was afebrile and doing well. A routine complete blood count (CBC) taken when the infant was aged 3 days revealed malaria parasites consistent with P. falciparum (less than 1% parasitemia). Quinine treatment was initiated, but because of his prematurity, he was dosed every 12 hours. Parasitemia persisted; therefore, the dosing of quinine was adjusted to every 8 hours. After 3 days of full-dose quinine (6 days total), no parasites were seen on blood smear. The infant also received 5 days of trimethoprim/sulfa. The infant experienced no complications; he recovered and was discharged. Blood smears from the mother demonstrated the presence of P. falciparum, and she was appropriately treated. Case 3. On January 29, 1995, a female infant was born in Texas at 39 weeks' gestation. The mother, a native of Nigeria, was visiting the United States. She reported having a fever at 6 months' gestation and was treated with intravenous fluids and ampicillin in Nigeria. At delivery, the mother was diagnosed with a urinary tract infection and treated with antibiotics. The infant and mother were discharged from the hospital 3 days after delivery. On February 23, 1995, the infant returned to the hospital with a 3-day history of fever to 101.5 F (38.6 C) and mild cough and was admitted for a sepsis evaluation. The infant had no history of rhinorrhea, irritability, respiratory distress, anorexia, emesis, diarrhea, rash, or contacts with ill persons. Examination of blood smear demonstrated the presence of parasites consistent with P. falciparum. The infant was successfully treated with chloroquine, and the mother was successfully treated with chloroquine and primaquine. Case 4. A full-term male infant was born in New Jersey on April 19, 1995, to a mother who had immigrated from India to the United States in 1993. The mother reported no international travel since her immigration to the United States. The delivery was uneventful, and the infant was discharged from the hospital a few days after birth. The infant was taken to a physician on May 25, 1995, at aged 1 month with a history of 3 days of fever. A CBC indicated anemia, and the infant was referred to a local emergency room. A repeat CBC indicated anemia, thrombocytopenia, and the presence of parasites. Results from thick and thin blood smears indicated P. vivax malaria, with an estimated 5% parasitemia. The species and parasite density were later confirmed by CDC. The infant was admitted to the pediatric intensive-care unit and because of the high degree of parasitemia, was started on intravenous quinidine sulfate. The infant received 1 day of intravenous therapy until the parasitemia dropped to 1%-3%; then, the intravenous quinidine was discontinued, and the infant received 2 days of oral chloroquine therapy. He also received a course of intravenous ampicillin for treatment of possible sepsis and was discharged on May 29, 1995. The mother had been asymptomatic during delivery and had negative blood smears. She was treated with courses of chloroquine and primaquine. Case 5. On July 14, 1995, a female infant was born in Kansas at 35 weeks' gestation to a mother who had immigrated from Vietnam in December 1994. The infant initially did well and was discharged several days after delivery. On August 4, 1995, she was readmitted with a history of high fevers and irritability. The infant was treated for neonatal jaundice and subsequently was diagnosed as having parasites consistent with P. vivax. Although the mother reported having had episodes of malaria in Vietnam, she was asymptomatic at the time of delivery. Both the mother and infant were treated with chloroquine and primaquine and recovered without complications. Cryptic Malaria Two cases of cryptic malaria were reported in 1995. Case 1. A woman aged 35 years who was born in Curažao, Netherlands Antilles, but had lived in New York City for several years developed smear-confirmed P. falciparum malaria on August 18, 1995. The diagnosis was not confirmed by CDC, but the hospital laboratory technician reported seeing banana-shaped gametocytes on the smear. The patient had traveled directly from the United States to Curažao without stopovers. She visited Curažao from July 10, 1995, to August 10, 1995. The patient reported no other risk factors for acquisition of malaria infection. Her only previous travel was in 1993 to the Dominican Republic and in 1991 to Venezuela. She recovered after treatment with quinine and doxycycline. Curažao is not a malarious area, and the patient's travel history dates were not consistent with exposure to P. falciparum malaria. Although presumed to be a case of local mosquito-borne infection, this case was classified as cryptic because a source of infection could not be proven. Case 2. On September 3, 1995, a man aged 31 years was admitted to a Michigan hospital with a 5-day history of chills, fever, sweats, and headache (8). On physical examination, he had a fever of 103 F (39.4 C) but no other abnormal findings. His CBC on admission indicated a white blood cell count of 3,100 and a platelet count of 69,000. On September 6, 1995, a blood smear evaluation indicated presence of parasites consistent with Plasmodium, species undetermined. P. vivax malaria infection was confirmed by CDC using slide examination, serologic tests, and DNA amplification using polymerase chain reaction. The patient was successfully treated with chloroquine and primaquine and was discharged on September 9, 1995. The patient had no history of any risk factors associated with malaria transmission, including travel outside of the United States. He lived approximately 5 miles from an airport in a suburban area. The patient reported three outdoor locations where he could have been exposed to anopheline mosquitoes at night: a rural campground in southeast Michigan where he slept outdoors during August 18-19, a suburban golf course south of Detroit where he played golf regularly in the evenings, and his backyard. CDC light traps were placed overnight at the campground and samples of two female competent vectors for malaria, Anopheles quadrimaculatus and Anopheles punctipennis, were recovered close to where the patient had camped. No adult or larval anophelines were recovered from the golf course or his backyard. Findings from an investigation conducted by CDC and the local and state health departments indicated that this case was most likely a local mosquito-borne infection, probably acquired at the campground in Michigan. Induced Malaria Two cases of induced malaria were reported in 1995, one acquired by organ transplantation, the other by transfusion. Case 1. A girl aged 18 years who had immigrated to Washington, D.C., from Ghana in 1991 developed end-stage renal disease of unknown etiology. She underwent a renal transplant on June 26, 1995; the next day, she received 2 units of packed red blood cells. The patient developed a fever, and on July 11, 1995, P. falciparum parasites were identified on her blood smear. The diagnosis was confirmed by CDC. Although the level of parasitemia was 15%, she responded well to treatment with intravenous quinidine and exchange transfusions. The patient had a history of malaria when she lived in Ghana (most recently in 1990) but had not traveled outside of the United States since immigrating in 1991. The kidney donor was her mother, who had immigrated to the United States in December 1993. The mother reported having her last episode of malaria in 1992; she was asymptomatic at the time of donation. The mother's blood smear indicated small rings and trophozoites; P. falciparum was suspected but could not be definitively diagnosed by blood smear. DNA amplification using polymerase chain reaction confirmed P. falciparum. Serologic testing for antimalarial antibodies on the donors of the two units of packed red blood cells was negative. Case 2. On September 28, 1995, the Pennsylvania State Health Department contacted CDC regarding a possible transfusion-associated intraerythrocytic infection. The patient was a woman aged 72 years with a history of multiple medical problems, including a large-cell lymphoma. On September 15, she was admitted to the hospital because of fever and neutropenia following a course of antineoplastic chemotherapy. During the 4 weeks before admission, she had received 8 units of packed red blood cells (4 units on August 9, 2 units on September 3, and 2 units on September 9). During the course of her hospitalization, intraerythrocytic parasites were identified on a peripheral blood smear. The infection was initially diagnosed as babesiosis; quinine and clindamycin therapy was initiated on September 26, and the patient improved. CDC confirmed the presence of P. falciparum after examining the patient's blood smears. On later review, parasites were present in blood smears prepared on September 4. Because the segments from the 6 units received on August 9 and September 3 were not available for testing, these six donors were contacted. All donors reported no international travel within 3 years of their donation, except for one donor who had made a day trip to Tijuana, Mexico, and another donor who could not be reached by telephone. These four donors were asked to visit their nearest Red Cross facility to provide a sample for blood smears and serology testing. One donor (Donor N), a native of Nigeria, reported a remote history of malaria. Specimens from this patient were received at CDC on October 6 and had small numbers of Plasmodia (species undetermined). Serologic testing using IFA was conducted on the patient and Donor N. Results for the index case were P. vivax 1: less than 16, P. falciparum 1:1024, P. malariae 1: less than 16, and P. ovale 1: less than 16. Results for Donor N were P. vivax 1:64, P. falciparum 1: greater than 4096, P. malariae 1: greater than 4096, and P. ovale 1:256. Blood samples collected from the remaining donors were negative by IFA for all four species of Plasmodium. Based on this investigation, the patient likely acquired the P. falciparum infection from the transfused unit of packed red blood cells donated by Donor N. The implicated donor reported no international travel within the preceding 3 years and was, therefore, an eligible donor. He was referred for treatment and will remain on the deferred donor list. Deaths Attributed to Malaria Six deaths attributed to malaria were reported in 1995. Case 1. On September 8, 1995, a clergyman aged 77 years returned to Texas after a month-long mission trip to Ghana. He had taken no antimalarial chemoprophylaxis during his travels. On September 9, he began to experience fever and chills and was seen in a local hospital emergency department on September 13. Blood smears at that time were reported as negative for intraerythrocytic parasites, and he was sent home with oral antibiotics. Five days later, he returned to the hospital because of fever, lethargy, and confusion. P. falciparum was identified on a peripheral blood smear, and arrangements were made to transfer him to a larger referral center. Emergency transportation was delayed for 24 hours. During this time, the patient continued to deteriorate, and his mental status worsened. Intravenous quinidine had been ordered, but treatment was never initiated because the drug had been removed from the hospital formulary and was not available at a nearby affiliated hospital. On arrival at the referral hospital, the patient had received no treatment for his malaria; peripheral blood smears demonstrated the presence of greater than 40% P. falciparum parasitemia. The patient developed hypovolemic shock, renal failure, hypoglycemia, respiratory distress, and disseminated intravascular coagulopathy. Antimalarial therapy was initiated with intravenous quinidine and clindamycin, but the patient died shortly after arriving at the referral center. Case 2. A man aged 49 years from South Asia was working on board a ship in the Gulf of Mexico when he developed an acute febrile illness on October 11, 1995. His last travel to a malarious area was in August 1995, when he had returned to his home in India. On October 20, the patient was sent ashore and hospitalized in Mexico. He rapidly developed acute renal failure, septic shock, and disseminated intravascular coagulopathy and was transferred to a referral hospital in Texas on October 22, 1995. On admission, examination of blood smears demonstrated the presence of overwhelming P. falciparum infection, with 80%-90% of red blood cells infected. Therapy was initiated with intravenous quinidine, but he died the same day before exchange transfusion could begin. Case 3. On October 10, 1995, a woman aged 59 years returned to Illinois from a 6-week missionary trip to Kenya and Zaire. Information concerning whether she took antimalarial chemoprophylaxis was unknown. On October 21, she went to a local hospital complaining of fever, chills, body aches, and shortness of breath. Initial laboratory studies demonstrated the presence of thrombocytopenia with elevated blood urea nitrogen and creatinine. She developed respiratory distress with diminished urine output and was transferred to the intensive-care unit at a referral hospital in Illinois. Hemodialysis was initiated in the intensive-care unit. A peripheral blood smear demonstrated the presence of P. falciparum infection with greater than 5% parasitemia. Treatment was initiated with intravenous quinidine. Despite hemodialysis, the patient continued to exhibit metabolic acidosis requiring bicarbonate infusion. She died on October 22. Case 4. On July 15, 1995, a man aged 67 years, a mining engineer, developed a low-grade fever with gastrointestinal symptoms upon returning to Florida after a business trip in Guyana. He had taken no antimalarial chemoprophylaxis during his travels. The patient was unable to go to his physician's office, but was prescribed BactrimTM over the phone. After 2 days, the fever did not resolve, and the patient went to a local emergency room. Upon examination of his peripheral blood smear, he was diagnosed with P. malariae infection. However, before the patient could be treated, he had signed out of the hospital against medical advice. The next day, he was called at home and prescribed a treatment dose of chloroquine, which he began on the same day. On July 27 during a follow-up visit with his physician, a repeat malaria smear was read as negative, and the patient returned home. When symptoms returned the next day, the patient was encouraged to seek hospitalization but declined to do so. On July 31, he returned to the hospital emergency room because of fever and confusion. At that time, blood smear examination revealed the presence of P. falciparum, which was later confirmed by CDC as having a parasitemia of 5%-8%. He began receiving treatment with intravenous quinidine and oral sulfadoxine-pyrimethamine. The patient developed acute respiratory distress and renal failure, which required dialysis. He suffered a fatal cardiac arrest on August 2. Case 5. On October 16, 1995, a man aged 41 years returned to North Carolina after a 6-month business trip to Rwanda and Zaire. He reported not using any antimalarial chemoprophylaxis during his travels. On October 21, he developed fever, chills, profuse sweating, myalgia, and anorexia. He attributed his symptoms to influenza and to muscle soreness after playing a game of football. On October 24, he went to a physician and complained of flu-like symptoms, dizziness, severe headache, cough, loss of depth perception, and diarrhea. He was treated with oral antibiotics for presumed bronchitis. On October 25, he developed severe nausea and vomiting and returned to the physician the next day because of fever, tachycardia, and hypotension. On October 26, he was admitted to the hospital for evaluation of suspected hepatitis. In the emergency room, thick and thin blood smears indicated the presence of P. falciparum malaria, with a 10%-15% parasitemia. Additional symptoms included hypoglycemia, decreased urinary output, and respiratory distress. Therapy was initiated with intravenous quinidine, and arrangements were made to transfer the patient to a referral hospital for exchange transfusions. Before transfer, the patient became comatose, developed renal failure, adult respiratory distress syndrome, and disseminated intravascular coagulopathy. In addition, he experienced a cardiac arrest but was successfully resuscitated. On arrival at the referral hospital, an exchange transfusion reduced peripheral parasitemia to less than 5%. Despite this improvement, the patient had a second episode of asystole and died later that day. Case 6. A woman aged 56 years, a resident of New York City, returned to visit her native home in the Dominican Republic from August to December 1994. She took no antimalarial chemoprophylaxis. The woman suffered from chronic renal failure from polycystic kidney disease and received hemodialysis biweekly, including during her visit to the Dominican Republic. On January 12, 1995, she received her regularly scheduled hemodialysis at a hospital in New York. She was diagnosed as anemic and received 2 units of packed red blood cells. Within 1 hour after transfusion of the second unit of blood, she developed fever, chills, and hypotension with no evidence of hemolysis. She was transported to the hospital emergency department, where she developed ventricular tachycardia that progressed to asystole. The patient was admitted to the intensive-care unit with multiple organ failure and developed a Coombs negative hemolytic anemia and disseminated intravascular coagulopathy. Blood smears obtained on January 13 were positive for P. falciparum, with less than 1% of red blood cells infected. The patient was treated with intravenous quinidine gluconate but died on January 16, 4 days after admission. Autopsy results revealed intraerythrocytic parasites, and CDC confirmed infection with P. falciparum in whole blood specimens taken before and after the transfusions on January 1. DISCUSSION A total of 1,167 cases of malaria were reported to CDC for 1995, representing a 15% increase from the 1,014 cases reported for 1994. This increase primarily resulted from an increase in cases acquired in Asia and the Americas, most notably a 100% increase reported from South America. This increase could have resulted from local changes in disease transmission, increased international travel, changing patterns of travel (i.e., immigration from malarious areas or "adventure tourism"), reporting errors, or a decreased use of effective antimalarial chemoprophylaxis. One reason for conducting malaria surveillance is to monitor emergence of drug resistance and the consequent failure of chemoprophylaxis. However, most cases (85.8%) of imported malaria in U.S. civilians occurred in persons who were either not taking or taking inadequate prophylaxis for the region in which they were traveling. Of the 93 persons who reported taking adequate prophylaxis, for 16 cases (i.e., 5 P. vivax, 1 P. ovale, and 10 P. falciparum), sufficient information was not available to determine whether they represented emerging drug resistance, reporting errors, or problems with compliance while using proper antimalarial chemoprophylaxis. Health-care providers should contact CDC if they suspect chemoprophylaxis failure, thus enabling measurement of serum drug levels of the antimalarial drug in question. The importance of taking proper precautions and chemoprophylaxis is underscored by the six fatal cases of malaria in the United States in 1995, including four cases in U.S. civilians who were not on prophylaxis during their exposure to endemic areas. An earlier review of deaths in the United States that were attributed to malaria helped CDC identify several risk factors for fatal malaria, including a) failure to take recommended antimalarial chemoprophylaxis, b) refusal to seek medical care, c) delay in seeking medical care, and d) misdiagnosis (9). A combination of these factors contributed to the six deaths reported in 1995. Signs and symptoms of malaria might be vague, but fever is generally present. Other symptoms include headache, chills, increased sweating, back pain, myalgia, diarrhea, nausea, vomiting, and cough. Prompt diagnosis requires that malaria be included in the differential diagnosis of illness in a febrile person with a recent history of travel to a malarious area. Clinicians should ask febrile patients for a travel history, particularly when evaluating febrile illnesses in international visitors, immigrants, refugees, migrant laborers, and international travelers. Treatment for malaria should be initiated immediately after the diagnosis has been confirmed by a positive blood smear. Treatment should be determined on the basis of the infecting Plasmodium species, the probable geographic origin of the parasite, the parasite density, and the patient's clinical status (10). Although non-falciparum malaria rarely causes complications, persons diagnosed as having P. falciparum infection are at risk for developing severe, life-threatening complications. Health-care workers are encouraged to consult appropriate sources for malaria treatment recommendations or call CDC's National Center for Infectious Diseases, Division of Parasitic Diseases at (770) 488-7788. Detailed recommendations for preventing malaria are available 24 hours a day from the CDC Malaria Hotline by telephone ({888} 232-3228) or facsimile ({888} 232-3299), or CDC's Website less than http://www.cdc.gov/travel/travel.html greater than . In addition, CDC annually publishes updated recommendations in the Health Information for International Travel (7), which is available through the Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402-9235; telephone (202) 512-1800. Acknowledgment The authors gratefully acknowledge the assistance of Jason B. Harris, M.P.H., Duke University School of Medicine, Durham, NC. References
* To obtain confirmation diagnosis of blood smears from questionable cases and to obtain appropriate treatment recommendations, contact either your state or local health department or CDC's National Center for Infectious Diseases, Division of Parasitic Diseases, Malaria Epidemiology Section; telephone (770) 488-7788. ** To confirm the diagnosis of questionable cases and to obtain appropriate treatment recommendations, contact either the state or local health department or CDC's National Center for Infectious Diseases, Division of Parasitic Diseases, Malaria Epidemiology Section; telephone (770) 488-7788. *** To track epidemiologic patterns of disease acquisition more effectively, new regional categories have been devised (Table_4). These categories separate world regions into smaller areas. See Table 3 (Table_3) for specific areas of acquisition. Table_1 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size. TABLE 1. Number of malaria cases* in U.S. and foreign civilians and U.S. military personnel -- United States, 1966-1995 ================================================================================================ Year U.S. military personnel U.S. civilians Foreign civilians Unknown Total ------------------------------------------------------------------------------------------------ 1966 621 89 32 22 764 1967 2,699 92 51 15 2,857 1968 2,567 82 49 0 2,698 1969 3,914 90 47 11 4,062 1970 4,096 90 44 17 4,247 1971 2,975 79 69 57 3,180 1972 454 106 54 0 614 1973 41 103 78 0 222 1974 21 158 144 0 323 1975 17 199 232 0 448 1976 5 178 227 5 415 1977 11 233 237 0 481 1978 31 270 315 0 616 1979 11 229 634 3 877 1980 26 303 1,534 1 1,864 1981 21 273 809 0 1,103 1982 8 348 574 0 930 1983 10 325 468 0 803 1984 24 360 632 0 1,016 1985 31 446 568 0 1,045 1986 35 410 646 0 1,091 1987 23 421 488 0 932 1988 33 550 440 0 1,023 1989 35 591 476 0 1,102 1990 36 558 504 0 1,098 1991 22 585 439 0 1,046 1992 29 394 481 6 910 1993 278 519 453 25 1,275 1994 38 524 370 82 1,014 1995 12 599 461 95 1,167 ------------------------------------------------------------------------------------------------ * An episode of microscopically confirmed malaria parasitemia in any person (symptomatic or asymptomatic) diagnosed in the United States, regardless of whether the person experienced previous episodes of malaria while outside the country. A subsequent attack of malaria occurring in a person is counted as an additional case if the demonstrated Plasmodium species differs from the initially identified species. A subsequent attack of malaria occurring in a person while in the United States could indicate a relapsing infection or treatment failure resulting from drug resistance if the demonstrated Plasmodium species is the same species identified previously. ================================================================================================ Return to top. Figure_1 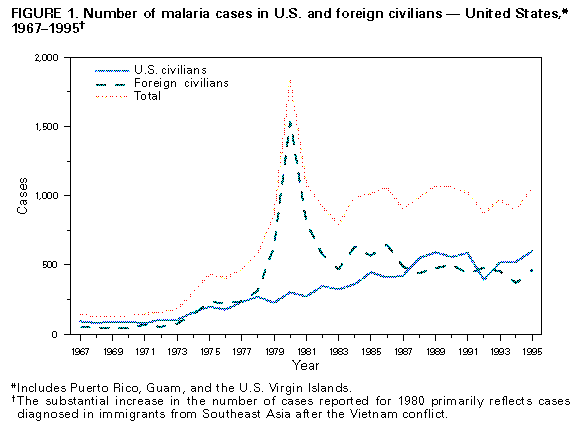 Return to top. Table_2 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 2. Number of malaria cases, by Plasmodium species --
United States, 1994 and 1995
=============================================================
1994 1995
---------------- --------------------
Plasmodium species No. (%) No. (%)
-------------------------------------------------------------
P. vivax 441 ( 43.5) 562 ( 48.2)
P. falciparum 442 ( 43.6) 450 ( 38.6)
P. malariae 43 ( 4.2) 46 ( 3.9)
P. ovale 34 ( 3.4) 26 ( 2.2)
Undetermined 50 ( 4.9) 80 ( 6.9)
Mixed 4 ( 0.4) 3 ( 0.3)
Total 1,014 (100.0) 1,167 (100.1)
=============================================================
Return to top. Figure_2 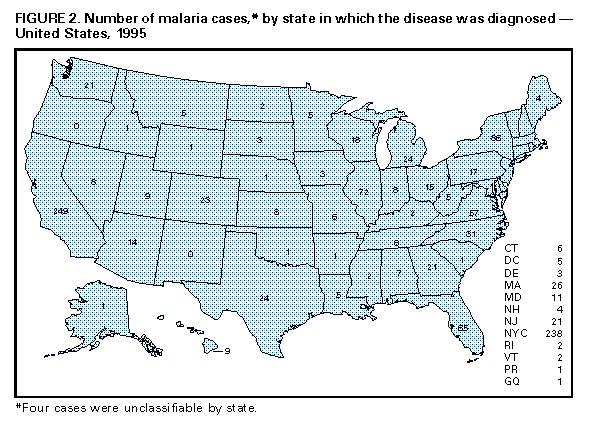 Return to top. Table_3 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 3. Number of malaria cases, by Plasmodium species and area of acquisition -- United States, 1995
=======================================================================================================================================
Plasmodium
species
-------------------------------------------------------------------------------------------------------
Area of acquisition P. vivax P. falciparum P. malariae P. ovale Unknown Mixed Total
---------------------------------------------------------------------------------------------------------------------------------------
AFRICA 48 373 25 19 54 0 519
Angola 0 4 0 0 0 0 4
Benin 0 0 0 1 0 0 1
Botswana 0 1 0 0 0 0 1
Cameroon 0 6 0 0 0 0 6
Congo 0 2 0 0 0 0 2
Cote d'Ivoire 0 13 0 1 4 0 18
Democratic Republic of the 0 5 0 1 0 0 6
Congo (Zaire)
Equatorial Guinea 0 2 0 0 0 0 2
Ethiopia 4 1 0 0 0 0 5
Gambia 0 3 1 0 0 0 4
Ghana 1 56 2 2 7 0 68
Guinea 0 7 0 1 0 0 8
Guinea-Bissau 1 0 0 0 0 0 1
Kenya 3 6 0 1 7 0 17
Liberia 0 8 0 0 1 0 9
Madagascar 3 2 0 0 1 0 6
Malawi 0 2 0 0 0 0 2
Mali 1 3 0 0 1 0 5
Mauritania 2 0 0 0 0 0 2
Mozambique 0 2 0 0 0 0 2
Niger 0 1 1 2 0 0 4
Nigeria 9 154 9 5 19 0 196
Rwanda 3 0 0 0 0 0 3
Sao Tome 1 0 0 0 0 0 1
Senegal 0 6 0 0 0 0 6
Sierra Leone 0 6 0 0 0 0 6
Somali Republic 1 0 0 0 0 0 1
South Africa 0 3 0 0 2 0 5
Sudan 5 0 1 0 0 0 6
Tanzania 1 8 0 0 3 0 12
Togo 1 5 1 0 0 0 7
Uganda 0 5 1 1 0 0 7
Zambia 0 3 0 0 0 0 3
Zimbabwe 0 2 0 0 0 0 2
Africa, East* 2 10 1 2 2 0 17
Africa, West* 2 17 3 1 2 0 25
Africa, Unspecified 8 30 5 1 5 0 49
ASIA 276 27 14 4 11 3 335
Afghanistan 0 0 1 0 0 0 1
Bangladesh 1 0 0 0 0 0 1
China 2 0 0 0 0 0 2
India 207 12 12 4 9 1 245
Indonesia 12 2 0 0 0 1 15
Laos 0 1 0 0 0 0 1
Malaysia 1 0 0 0 0 0 1
Myanmar 2 2 0 0 0 0 4
Pakistan 36 2 1 0 1 0 40
Thailand 3 0 0 0 0 0 3
Viet Nam 4 1 0 0 0 0 5
Yemen 1 5 0 0 0 0 6
Asia, Southeast* 2 2 0 0 0 1 5
Asia, Unspecified* 5 0 0 0 1 0 6
CENTRAL AMERICA AND 159 32 4 2 4 0 201
CARIBBEAN
Belize 8 3 0 0 2 0 13
Costa Rica 1 1 1 0 0 0 3
Dominican Republic 0 1 0 0 0 0 1
El Salvador 3 0 0 0 0 0 3
Guatemala 18 1 0 0 0 0 19
Haiti 2 15 0 0 0 0 17
Honduras 82 4 3 1 1 0 91
Netherlands Antilles 0 1 0 0 0 0 1
Nicaragua 14 3 0 0 1 0 18
Central America, Unspecified* 30 3 0 1 0 0 34
Carribean, Unspecified* 1 0 0 0 0 0 1
NORTH AMERICA 10 2 1 1 1 0 15
United States 1 2 0 0 0 0 3
Mexico 9 0 1 1 1 0 12
SOUTH AMERICA 20 6 1 0 3 0 30
Bolivia 1 0 0 0 0 0 1
Brazil 4 0 0 0 0 0 4
Colombia 2 0 0 0 0 0 2
Ecuador 4 1 1 0 2 0 8
French Guiana 0 0 0 0 1 0 1
Guyana 5 4 0 0 0 0 9
Peru 2 1 0 0 0 0 3
Venezuela 1 0 0 0 0 0 1
South America, Unspecified* 1 0 0 0 0 0 1
OCEANIA 23 3 0 0 1 0 27
Papua New Guinea 15 3 0 0 0 0 18
Solomon Islands 7 0 0 0 1 0 8
Oceania, Unspecified* 1 0 0 0 0 0 1
Unknown* 22 5 0 0 13 0 40
Total 558 448 45 26 87 3 1,167
----------------------------------------------------------------------------------------------------------------------------------------
* Country unspecified.
========================================================================================================================================
Return to top. Table_4 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 4. Number of reported malaria cases, by region of acquisition -- United States, 1995
===================================================================================================
Total
---------------------------------------------------------------------------------------------------
AFRICA
Central Africa 37
Angola, Cameroon, Central African Republic, Chad, Congo, Democratic Republic of
the Congo (Zaire), Equatorial Guinea, Ethiopia, Gabon, Sao Tome, Sudan, Zambia,
Zimbabwe; Central Africa, unspecified*,
East Africa 67
Burundi, Comoros, Kenya, Madagascar, Malawi, Mozambique, Rwanda, Somali Republic,
Tanzania, Uganda; East Africa, unspecified*
North Africa 0
Algeria, Djibouti, Egypt, Libya, Morocco, Tunisia; North Africa, unspecified*
South Africa 6
Botswana, South Africa, Swaziland; South Africa, unspecified*
West Africa 360
Benin, Cote d'Ivoire, Gambia, Ghana, Guinea, Guinea-Bissau, Liberia, Mali,
Mauritania, Niger, Nigeria, Senegal, Seychelles Island, Sierra Leone, Togo, Upper
Volta; West Africa, unspecified*
Africa 49
Unspecified*
Total 519
---------------------------------------------------------------------------------------------------
AMERICAS
Central America and Caribbean 213
Belize, Costa Rica, Cuba, Dominican Republic, El Salvador, Guatemala, Haiti,
Honduras, Mexico, Netherlands Antilles, Nicaragua, Panama; Central America and
Caribbean, unspecified*
North America
Canada, United States of America; North America, unspecified* 9
South America 30
Bolivia, Brazil, Colombia, Ecuador, French Guiana, Guyana, Peru, Suriname,
Venezuela; South America, unspecified*
Total 252
---------------------------------------------------------------------------------------------------
ASIA
China 2
Indian Subcontinent
Afghanistan, Bangladesh, India, Nepal, Pakistan 287
Sri Lanka; Indian Subcontinent, unspecified*
South East Asia 35
Cambodia, Indonesia, Laos, Malaysia, Myanmar, Philippines, Singapore, Thailand,
Viet Nam; South East Asia, unspecified*
Asia 6
Unspecified*
Total 330
---------------------------------------------------------------------------------------------------
MIDDLE EAST 6
Egypt, Iran, Iraq, Turkey, Saudi Arabia, Yemen; Middle East, unspecified*
Total 6
---------------------------------------------------------------------------------------------------
OCEANIA 27
Papua New Guinea, Solomon Islands, Vanuatu; Oceania, unspecified*
Total 27
---------------------------------------------------------------------------------------------------
UNKNOWN+ 32
TOTAL NUMBER OF CASES BY REGION 1,166
---------------------------------------------------------------------------------------------------
* Country unspecified.
+ For one case, information regarding region of acquisition was unavailable.
===================================================================================================
Return to top. Table_5 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 5. Number of imported malaria cases, by Plasmodium species and by interval between date of arrival in the country and onset of illness
-- United States, 1995
=============================================================================================================================================
Plasmodium
species
----------------------------------------------------------------------------------------------
P. vivax P. falciparum P. malariae P. ovale Total
------------------- ------------------- -------------------- -------------------- ---------------
Interval (days) No. (%) No. (%) No. (%) No. (%) No. (%)
--------------------------------------------------------------------------------------------------------------------------------------------
<0* 20 ( 4.6) 44 ( 12.0) 1 ( 3.2) 1 ( 4.8) 66 ( 7.8)
0- 29 154 ( 35.6) 292 ( 79.6) 14 ( 45.2) 4 ( 19.0) 464 ( 54.5)
30- 89 86 ( 19.9) 24 ( 6.5) 5 ( 16.1) 2 ( 9.5) 117 ( 13.7)
90-179 65 ( 15.0) 4 ( 1.1) 4 ( 12.9) 7 ( 33.3) 80 ( 9.4)
180-364 87 ( 20.1) 2 ( 0.5) 5 ( 16.1) 5 ( 23.8) 99 ( 11.6)
>=365 20 ( 4.6) 1 ( 0.3) 2 ( 6.5) 2 ( 9.5) 25 ( 2.9)
Total 432 ( 99.8) 367 (100.0) 31 (100.0) 21 ( 99.9) 851 ( 99.9)
---------------------------------------------------------------------------------------------------------------------------------------------
* Cases with onset of illness before arrival in the United States.
=============================================================================================================================================
Return to top. Table_6 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 6. Number of imported malaria cases in U.S. and foreign civilians, by region of acquisition -- United States, 1995
=============================================================================================================================
U.S. civilians Foreign civilians Total
------------------------- ------------------------ --------------------
Region of acquisition No. (%) No. (%) No. (%)
-----------------------------------------------------------------------------------------------------------------------------
Africa 287 (48.6) 177 (38.7) 464 ( 44.3)
Asia, Unknown 5 ( 0.8) 1 ( 0.2) 6 ( 0.6)
Central America and Caribbean 116 (19.6) 77 (16.8) 193 ( 18.4)
China 2 ( 0.3) 0 ( 0 ) 2 ( 0.2)
Middle East 2 ( 0.3) 4 ( 0.9) 6 ( 0.6)
Oceania 24 ( 4.1) 2 ( 0.4) 26 ( 2.5)
South East Asia 25 ( 4.2) 7 ( 1.5) 32 ( 3.1)
South America 18 ( 3.0) 10 ( 2.2) 28 ( 2.7)
Indian subcontinent 95 (16.1) 174 (38.1) 269 ( 25.7)
Unknown+ 17 ( 2.9) 5 ( 1.1) 22 ( 2.1)
Total 591 (99.9) 457 (99.9) 1,048 (100.2)
-----------------------------------------------------------------------------------------------------------------------------
* Country unknown.
+ Region of acquisition unknown.
=============================================================================================================================
Return to top. Table_7 Note: To print large tables and graphs users may have to change their printer settings to landscape and use a small font size.
TABLE 7. Number of imported malaria cases in U.S. civilians, by purpose
of travel at the time of acquisition -- United States, 1995
==========================================================================
Imported cases
---------------------
Category No. (%)
--------------------------------------------------------------------------
Unknown 284 ( 48.1)
Teacher/Student 83 ( 14.0)
Visitor of a friend or relative 51 ( 8.6)
Tourist 50 ( 8.5)
Missionary 48 ( 8.1)
Business representative 36 ( 6.1)
Peace Corps worker 15 ( 2.5)
Government employee 11 ( 1.9)
Sailor 5 ( 0.8)
Refugee 4 ( 0.7)
Other 4 ( 0.7)
Total 591 (100.0)
==========================================================================
Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 02/25/99 |
|||||||||
This page last reviewed 5/2/01
|