 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Advances in Global Measles Control and Elimination: Summary of the 1997 International MeetingSUMMARY A meeting concerning advances in measles control and elimination, the third in a series, was held in Atlanta during August 1997. The meeting was cosponsored by CDC, the Pan American Health Organization, the World Health Organization, and the United Nations Children's Fund. Meeting participants concluded that substantial progress has been made toward controlling measles. Measles transmission has been interrupted in several countries, reinforcing the view that measles eradication is technically feasible using existing vaccines and intervention strategies. However, measles still accounts for 10% of global mortality from all causes among children aged less than 5 years (i.e., approximately 1 million deaths annually). Progress toward measles control varies substantially among countries and regions. Intensified efforts are necessary to implement appropriate control and elimination strategies, including supplementary vaccination campaigns, expansion of routine vaccination services, and surveillance. These strategies and estimates of the resources required to implement them will require adjustment based on accumulating experience. Programmatic and financial obstacles must be overcome if the final goal of measles eradication is to be achieved. INTRODUCTION The Third Meeting on Advances in Measles Control and Elimination was held in Atlanta from August 27 through 29, 1997. The meeting was cosponsored by CDC, the Pan American Health Organization (PAHO), the World Health Organization (WHO), and the United Nations Children's Fund (UNICEF). The objectives of the meeting were to
This report, which summarizes the discussions and conclusions of the meeting, should be read in conjunction with the report of the Second Meeting on Advances in Measles Control and Elimination (1), which concluded,"Participants agreed that measles eradication is technically feasible with available vaccines and recommended adoption of the goal of global eradication with a target date during 2005-2010, with the proviso that measles eradication efforts should not interfere with polio eradication but should build on the successes of the global Poliomyelitis Eradication Initiative." GLOBAL EXPERIENCE WITH MEASLES CONTROL The efforts of individual countries and global efforts through the EPI have substantially reduced measles morbidity and mortality throughout the world. Worldwide, for 1996, global coverage of the population of children aged 1 year with one dose of measles vaccine is estimated at 81% (2) (Figure_1). However, progress in controlling measles varies substantially among WHO regions (Figure_2). An estimated 36.5 million cases and 1 million deaths caused by measles still occur each year. About half of these deaths occur in Africa. Sixteen of 19 countries in which fewer than 50% of children aged 1 year have received at least one dose of measles vaccine are in Africa. Despite poor measles surveillance, Africa also has the highest reported incidence of measles. Measles Elimination in the Western Hemisphere In September 1994, the member nations of PAHO established the goal of eliminating measles from the Western Hemisphere by 2000. The strategy adopted included three complementary approaches to immunization:
Application of this strategy has substantially reduced measles transmission in the Americas (Figure_3). Several countries including Chile, Cuba, and the nations of the English-speaking Caribbean have reported no cases of measles for greater than or equal to 3 years. In other countries of the region, measles transmission is now occurring only sporadically. During 1996, 2,109 confirmed cases of measles were reported in the Western Hemisphere -- the fewest ever reported. Of these cases, 44% were confirmed by laboratory tests or epidemiologically linked to laboratory-confirmed cases, and 56% were classified as "clinically confirmed" (i.e., neither confirmed by serologic test nor epidemiologically linked to a serologically confirmed case). Of the laboratory-confirmed cases, 816 (88%) occurred in the United States and Canada. Most countries in the region reported sporadic cases or no cases of measles. Obstacles to measles elimination in the Americas include increasing numbers of infants and children who are susceptible to measles, the circulation of measles virus in other parts of the world, and importation of cases of measles and subsequent spread of measles virus. The number of infants and children susceptible to measles in a population tends to increase over time even when high routine vaccination coverage with a highly effective vaccine is maintained. For example, in a population with an annual birth cohort of 100,000 children, 90% routine vaccination coverage, and 90% vaccine efficacy, approximately 19,000 children are added each year to the population that is susceptible to measles. The state of S o Paulo, Brazil experienced an outbreak of measles during 1997. By the end of December, greater than 31,000 cases had been reported. This outbreak occurred after several years during which few measles cases occurred because of a catch-up measles vaccination campaign in 1987 and a campaign conducted during 1992 to vaccinate children aged 1-10 years with MMR vaccine. After the 1992 campaign, health authorities in S o Paulo state implemented a two-dose measles vaccination strategy. The first dose is routinely administered to infants aged 9 months and the second dose to children aged 15 months. During the 1997 outbreak, most cases occurred among residents of metropolitan S o Paulo. During the 1997 outbreak, most cases occurred among residents of metropolitan Sao Paulo. Provisonal data concerning the age and vaccination status of cases indicate that 64% occurred among persons aged greater than or equal to 15 years, most of whom were unvaccinated; 16% occurred among infants and 6% among children aged 1-4 years, many of whom also were unvaccinated. The highest age-specific incidence rates were observed among infants (849 cases per 100,000 population), followed by persons aged 20-29 years (307 cases per 100,000 population) and children aged 1-4 years (91 cases per 100,000 population). The outbreak spread to other states in Brazil and other countries in the Western Hemisphere. Factors contributing to the outbreak in S o Paulo have not been completely clarified but may include
Genomic sequencing of virus strains isolated from persons with measles in S o Paulo during 1997 revealed that these strains were identical or nearly identical to viruses circulating in parts of Europe, indicating that the outbreak may have been triggered by importation of measles virus from Europe. In Canada, introduction of measles vaccine in 1963 substantially reduced the occurrence of measles. The country relied on a one-dose measles vaccination strategy until 1995, when a major outbreak (i.e., greater than 2,000 cases) prompted adoption of a two-dose vaccination schedule. The second dose is administered to children aged 18 months or 4-5 years. The two-dose strategy was implemented in all 12 Canadian provinces during 1996 and early 1997. Canada's National Advisory Committee on Immunization further recommended that all children and adolescents who had previously received a single dose of measles-containing vaccine receive a second dose. Six provinces completed catch-up vaccination of school children in 1996, achieving 90% coverage. However, during January through April 1997, a measles outbreak occurred in British Columbia and spread to Alberta. British Columbia had carried out catch-up vaccination in 1996, achieving 75% coverage of preschool-aged children and approximately 90% coverage of school-aged children. The outbreak in British Columbia primarily involved young adults (i.e., college students) who were not vaccinated during the 1996 catch-up effort. Alberta had not carried out catch-up vaccination and its outbreak, which occurred from February through July 1997, primarily involved school-aged children. In the United States, measles incidence is at the lowest level ever measured. In 1996, a total of 488 cases was reported and, in 1997, a total of 135 cases. International importations and cases directly linked to international importations accounted for more than half of all cases reported in 1996 and 1997. During 1996, the reported incidence of measles in the United States was less than 1 per 1 million population in all age groups. Measles vaccination coverage among children aged 2 years reached 91% in 1996, and 98% of children entering school had received at least one dose of measles-containing vaccine. Approximately 64% of all school-aged children had received two doses of measles vaccine. Evidence from case investigations and molecular epidemiologic studies indicates that measles transmission has been interrupted in the United States at least three times -- in late 1993, in 1995, and in 1996. During 1992-1996, Japan, Germany, the Philippines, the United Kingdom, France, India, and Italy were the leading sources of measles cases imported to the United States. In 1997, leading exporters of measles cases to the United States were Germany, Italy, Brazil, China, France, Pakistan, and the Philippines (Figure_4). The increasing proportion of all measles cases caused by imported virus strains indicates that further reduction of measles incidence in the United States requires international cooperation and improved global control of measles. Other Global Experiences with Measles Control and Elimination Africa In South Africa, measles vaccine was added to the National Immunization Days (NIDs) for polio eradication in 1996. During 1997, efforts were made to ensure that all children aged 1-14 years had received measles vaccine during catch-up vaccination campaigns in 1996 or 1997. Analysis of South Africa's experience during the 1996 NIDs revealed several issues to be addressed in future NIDs in which multiple vaccines are administered (i.e., training personnel to administer injections, disposing appropriately of used needles and syringes, and dealing with different target age groups for the two vaccines). The combined 1996 and 1997 campaigns achieved 91% coverage of the eligible age cohort, although coverage varied substantially among provinces and within provinces. South Africa is moving to eliminate measles, but accomplishing the goal will require strengthening surveillance, improving routine vaccination services, and conducting follow-up campaigns. Several other countries in southern Africa that have made substantial progress in polio eradication, and which have strong basic EPI programs (i.e., Namibia, Botswana, Zimbabwe, and Swaziland), also have launched or are planning catch-up measles vaccination campaigns. These countries have not yet established laboratory-based surveillance. Western Pacific Region The Western Pacific Region of WHO includes the most populous as well as some of the smallest countries of the world. Most countries in the region are now free of polio and are devoting more attention to measles. Approximately 100,000 cases of measles are reported in the region each year, despite measles vaccine coverage exceeding 90%. Many countries of the region are now implementing supplemental measles control activities. During 1996, Mongolia conducted a catch-up campaign to vaccinate children aged 9 months through 11 years, achieving 97% coverage. Few cases of measles were reported in Mongolia from July through December 1996, and no confirmed cases were reported from January through May 1997. Many of the Pacific island nations have been free of measles for some time, although periodic outbreaks caused by measles importations continue to occur. The number and size of these outbreaks have decreased steadily since the introduction of measles vaccination in the mid-1970s. The 20 island nations of Melanesia, Polynesia, and Micronesia are planning intensified measles control efforts. Through coordinated action, these nations hope to emulate the successful measles elimination efforts of the English-speaking Caribbean islands. No measles cases were reported in these 20 nations during 1995, but four outbreaks -- all in Polynesia -- occurred in 1996. Other countries in the Western Pacific Region (e.g., Australia, New Zealand, and the Philippines), have already begun measles elimination initiatives or are considering them. Nationally, New Zealand has achieved 87% coverage with one dose of measles-containing vaccine, but in some segments of the population, coverage is substantially lower. A mass vaccination campaign was planned in July 1997 to prevent an anticipated epidemic in these populations, but onset of the epidemic began in April. The mass campaign was started in May and probably limited spread of measles. China, which implemented a two-dose measles vaccination schedule in 1985, experienced substantial reductions in measles morbidity and mortality beginning in 1987. Fewer than 75,000 cases were reported in 1996, and only 108 deaths were reported in 1995 compared with more than 1 million cases and 4,200 deaths in 1981. In 1997, China issued a national plan for accelerated measles control. The national plan called for the development of provincial plans of action but did not establish a formal national target date for measles elimination. Eastern Mediterranean Region In October 1996, participants in a Consultation on Measles Control/Elimination in the Eastern Mediterranean Region recommended that enhanced control measures be undertaken with the aim of eliminating measles from the region. However, participants also recognized that substantial differences existed among the countries of the region in vaccination strategies, vaccination coverage, sensitivity of surveillance, and occurrence of disease. Eight of the 23 countries in the region use a one-dose measles vaccination strategy; in the 15 that use a two-dose strategy, the age at which the second dose is administered and the vaccine of choice (measles vaccine or combination vaccines {MR or MMR}) vary. In 1996, region-wide coverage of children aged 2 years with at least one dose of measles-containing vaccine was greater than or equal to 80% but varied considerably. In two countries, vaccination coverage among children aged 2 years was less than 50%. A proposed plan and target date for elimination of measles from the region by 2010 was approved by the WHO Regional Committee in October 1997. The Gulf Council countries (i.e., Kuwait, Oman, Bahrain, Qatar, Saudi Arabia, and United Arab Emirates) are aiming for measles elimination by 2000. During NIDs conducted during a 1994 cease-fire in Sudan's ongoing civil conflict, measles vaccine was administered to 61% of children aged less than 5 years. During a similar 1995 "Tranquility Days" cease-fire, vaccination for polio, measles, and other diseases and other public health interventions (i.e., Vitamin A distribution and Guinea worm eradication activities) were also conducted in war-affected areas. Coverage with measles vaccine in Sudan is now approximately 75%, and ten of 26 states have measles vaccination coverage greater than 80%. Coverage in war-affected areas is much lower (less than 30%). As a result of special efforts to immunize war-displaced children, substantially fewer outbreaks of measles have occurred in refugee camps. European Region A strategic plan for elimination of measles from the WHO European Region by 2007 has been developed by the WHO European Advisory Group and will be presented to the WHO European Regional Committee for consideration during 1998. A questionnaire regarding measles control practices and strategies was sent to all 50 member states; 41 responded. In the 38 responding countries that use a two-dose measles vaccination strategy, the age for administration of the second dose ranges from 3 to 14 years. Twenty-one countries in the region report greater than or equal to 90% coverage with at least one dose of measles, eight report coverage of 80%-89%, nine indicate 50%-79% coverage, and three countries report coverage less than 50%. Regionwide, coverage of children aged 12-24 months with at least one dose of measles-containing vaccine is 82%. The regional strategy to eliminate measles includes: establishing political commitment to measles elimination, developing measles elimination plans based on local epidemiologic data, achieving and maintaining high vaccination coverage, and strengthening surveillance. On the basis of their progress in measles control, European countries have been classified into three groups. Group 1 comprises six countries that are close to eliminating the disease. These countries are characterized by;
The four countries in Group 2 have achieved good control of measles but are considered potentially at risk for measles outbreaks. These countries are characterized by
Countries in Group 3 (31 countries) have poor control of measles and are characterized by
UNICEF Urban Measles Control Initiative UNICEF, in collaboration with WHO, is supporting an initiative to reduce deaths among young children (i.e., those aged less than 5 years) through urban measles control. The initiative is intended to catalyze improvements in child health activities in under-served urban areas. In such areas, where a substantial percentage of children is susceptible to the disease, measles circulates easily, affects infants, and is often exported to surrounding rural areas. The UNICEF/WHO strategy is to develop local partnerships to improve routine immunization services in poor urban areas, plan and carry out measles campaigns in high-risk areas, develop community-based measles surveillance, and promote child health and development. The proposed target age group is children aged 9-59 months, although the age group may vary on the basis of local epidemiologic findings. In addition to measles vaccination, campaigns undertaken as part of the initiative will include vitamin A supplementation. Vaccine will be administered with autodestruct syringes, and safety boxes will be provided for disposal of used injection equipment. Development of measles surveillance to evaluate the impact of immunization activities will be an integral part of the initiative. Conclusions: Progress Toward Measles Elimination
MEASLES SURVEILLANCE In a measles elimination program, surveillance is intended to detect measles virus circulation in a timely manner (rather than to detect every single case), allowing public health authorities to undertake rapid ascertainment and investigation of suspected cases, determine risk factors for the disease, and implement outbreak control measures. In Latin America and the English-speaking Caribbean, measles surveillance has been integrated with polio surveillance. Twenty thousand reporting units, at least one in each district or municipio (equivalent to a township or county), have been established in these countries. Weekly reporting is the norm, both for the occurrence of cases and the absence of cases (i.e., negative reporting). Cases are classified as "suspected," "discarded," or "confirmed." A suspected case is any illness that a health-care worker suspects might be caused by measles infection. Surveillance norms call for all suspected cases to be investigated thoroughly and promptly. Thorough investigation includes collection of a single serum specimen at the time of the patient's first contact with the health-care system and collection of appropriate specimens for virus isolation from every detected chain of transmission. A suspected case may be confirmed by a positive immunoglobulin M (IgM) antibody test of the serum specimen or by epidemiologic linkage to a case confirmed by such a laboratory test. Specimens are tested first with a commercial indirect IgM assay. Specimens that yield indeterminate results are tested with an IgM-capture enzyme immunoassay (EIA) developed by CDC (3) and are classified as confirmed if this more specific assay yields a positive result. A suspected case is discarded if a complete investigation fails to identify an epidemiologic link to a laboratory-confirmed case and a negative result is obtained from the IgM antibody test of the blood specimen. Suspected cases that are not completely investigated are classified as "clinically confirmed" and are considered to represent a failure of the surveillance system. During 1996, in the countries of Latin America and the Caribbean, a total of 10,144 suspected measles cases was completely investigated; laboratory tests in 90 (0.9%) cases were positive for measles. Six surveillance indicators are being used in the Americas as of September, 1997:
During 1995-1997, PAHO conducted evaluations of surveillance systems in Brazil, El Salvador, Mexico, Nicaragua, Panama, and Venezuela. The evaluations included interviews with health workers; search of patient records at hospitals, health centers, schools, day care centers, and private clinics; and analysis of the indicators listed previously. The reviews concluded that surveillance systems in three of the countries had the capacity to detect cases rapidly but that surveillance systems in the other three did not. On the basis of these evaluations, PAHO concluded that its surveillance indicators were useful for continually monitoring the quality of the regional and national surveillance systems. PAHO recommended that every member country conduct periodic evaluations to ensure that its surveillance system is capable of timely detection of measles virus circulation. Susceptibility profiles (i.e., estimates of the proportion of the population susceptible to measles by age) can be useful to help guide measles elimination strategies. In countries where measles virus continues to circulate, susceptibility profiles can be developed based on history of vaccination -- whether with one or two doses of measles-containing vaccine -- or history of disease, age distribution, and vaccination status of recent cases. As incidence declines, serologic surveys and mathematical modeling can be used to estimate susceptibility profiles. These profiles can, in turn, be used in deciding the timing of and age range for vaccination campaigns. Repeated serologic surveys are most useful if the incidence of measles is low and the quality of vaccination coverage data is poor. Role of the Laboratory in Measles Surveillance Recent field experience has demonstrated the usefulness and reliability of IgM EIAs for confirmation of suspected measles cases. Commercially available IgM EIAs can be done quickly, are sensitive and specific, and require only one serum specimen. The CDC antibody-capture EIA is used as a confirmatory test after initial testing with one of the commercially available assays, which are usually simpler and faster to perform (3). In tests of persons naturally infected with measles virus, the CDC test was positive in 77% of specimens obtained within 72 hours of rash onset and 100% of specimens obtained 4-11 days after rash onset; for 90% of these patients, second specimens obtained 28 days after rash onset were also IgM-positive (4). The measles virus is a negative-stranded RNA virus with 15,894 nucleotides and six genes. Virus isolation and genotyping can be used to monitor changes in the genotypic pattern over time if genotyping is done before and after major control and elimination efforts. These molecular epidemiologic studies can be used to demonstrate interruption of measles virus transmission when it occurs. To facilitate communication among laboratories, a standard system of nomenclature to categorize the genotypes should be developed. In the interim, eight arbitrarily numbered genotypes -- all of them isolated in North America during the period 1988-1997 -- have been identified. Group 1 includes all vaccine viruses regardless of geographic origin, several recently isolated wild viruses, and all wild viruses isolated from Europe and the United States during the 1950s and 1960s. Measles viruses isolated in Japan are mostly from Groups 2 and 3; viruses isolated in Europe are predominantly Groups 4 and 5. Group 6 viruses predominate in Africa and Group 8 in China and Vietnam. Group 7 viruses have a broad geographic distribution. The resurgence of measles in the United States during 1988-1992 was caused almost entirely by Group 2 viruses. The absence of Group 2 virus from United States since 1993, except in one case imported from the Philippines, indicates that measles transmission was interrupted in the United States in 1993. Conclusions: Measles Surveillance Epidemiologic Aspects
Laboratory Aspects
VACCINE SAFETY Adverse events that occur after vaccination can be caused by the vaccine, occur coincidentally (i.e., the events may be temporally but not causally related), or result from programmatic errors. Adverse events caused by the vaccine include local and systemic reactions, febrile convulsions, allergic reactions, and anaphylaxis. Adverse events caused by programmatic errors include those resulting from unsafe injection practices (e.g., abscesses at the injection site, toxic shock syndrome, septicemia, and transmission of bloodborne viral infections, including hepatitis B or C and human immunodeficiency virus {HIV}), and illness or injury caused by administration of vaccine to persons for whom it is contraindicated. Unsafe injection practices can affect the vaccine recipient, the person administering the vaccine (e.g., through needle stick injuries), or other members of the community (e.g., because of improper disposal of needles and syringes). Immunization activities represent about 10% of the global total of injections administered each year. Approximately 800 million injections were administered in routine EPI activities in the developing world in 1996, and another 240 million injections were administered in emergency vaccination campaigns. If the world's nations all adopt measles elimination strategies, 1.6 billion children could receive a single additional injection in measles catch-up vaccination campaigns and approximately 150 million could receive follow-up injections each year. Most of these vaccinations are likely to be administered by syringe because currently available jet injectors are not recommended for use in mass vaccination campaigns. New jet injectors are under development and will be field tested beginning in 1998, but their cost and suitability for use in developing countries are unknown. The problems of using disposable needles and syringes for vaccination, whether for routine vaccination or in mass catch-up campaigns, are appreciable. Equipment shortages during mass campaigns or failure to dispose of used equipment after the campaign can increase risks for reuse of disposable syringes. Autodestruct syringes, by contrast, pose no risk for reuse during or after the campaign. Whether autodestruct syringes or disposable syringes are used, collection and incineration of used syringes and needles should be part of all mass vaccination campaigns. Experience in the United Kingdom illustrates the importance of surveillance in establishing the background incidence of adverse events and monitoring their occurrence during and after a catch-up vaccination campaign. During a 1-month period in 1994, MR vaccine was administered to 92% of the United Kingdom's 8.4 million children aged 5-16 years. The surveillance system received 1,231 reports of 2,783 adverse events; included were 709 serious reactions affecting 557 children. More than half the reported events (e.g., allergic reactions, syncope, or convulsions) occurred within 24 hours after vaccination. A total of 120 reports were received of immediate allergic reactions or anaphylaxis. Approximately half of these children were referred to hospitals but few were admitted overnight; all recovered fully. Adrenaline was administered to fewer than half the children reported to have experienced anaphylaxis, indicating that the reported events may not have been true anaphylactic reactions. Investigation revealed that 24 of 29 reports of "convulsions" were episodes of syncope. Rates of most adverse events, including arthritis and facial palsy, were lower than background levels. Conclusions: Vaccine Safety
RESEARCH Presentations during the meeting addressed research in three areas relevant to measles eradication: a) opportunities for research concerning measles immunology, b) development of alternative routes for administration of measles vaccine, and c) optimal age for measles vaccination. Measles virus and measles vaccinology offer unique opportunities for research in several areas -- molecular and basic research, epidemiologic research, clinical disease and diagnostics, new vaccines, and new routes of administration. Studies have begun to examine measles-induced immune suppression, the pathogenesis of measles, alternative formulations and means of administration of measles vaccines, correlates of vaccine-induced cellular and humoral immunity, and the role of adjuvants in measles vaccines. Studies of immunocompromised persons infected with measles are particularly important because of the increasing incidence and prevalence of HIV infection. Particularly relevant to control and elimination of measles is research concerning persistent carriage of measles virus by immunocompromised persons. Findings of several studies indicate that aerosol administration of measles vaccine is effective, particularly if Edmonston-Zagreb vaccine is used. Administering measles vaccine by the aerosol route is rapid, might be less costly than single-use needles and syringes, is nontraumatic, avoids risks for transmission of HIV and hepatitis B, and does not require medically trained personnel. Aerosols are easy to administer to school-aged children but are more difficult to administer to younger children and infants. The apparatus for administration of aerosol vaccines has limitations; it is cumbersome, requires crushed ice, and is not useful for single dose administration. Questions remain about possible effects on vaccinators of repeated exposure to aerosolized measles virus and potential adverse effects of aerosol vaccines, particularly among persons infected with HIV. Factors that affect the optimal age for administering the first dose of measles vaccine include the risk for measles among infants, vaccination coverage among young children and infants, the prevalence in the target population of possible alterations in immunity caused by acquired conditions (e.g., HIV infection), and vaccine effectiveness, which is relatively low among infants because of maternally derived antibody but increases as children grow older. Factors that affect the optimal age range for inclusion in catch-up or follow-up measles vaccination activities include cost, the prevalence of measles susceptibility among young adults, and ease of access to unvaccinated persons. Conclusions: Research
ECONOMIC IMPLICATIONS OF MEASLES ELIMINATION An economic evaluation presented at the meeting compared several options for future measles for a hypothetical western European country immunization policy, including the baseline case of no change in vaccination policy. All other options saved costs compared with the baseline. Optimal choices depended upon assumptions concerning past success in measles vaccination. If 70% of children aged less than or equal to 2 years were assumed to have been vaccinated, the optimal strategy would be to increase vaccination coverage with the first dose to greater than or equal to 95%, adopt a two-dose vaccination policy, and conduct mass vaccination campaigns among persons in age groups with susceptibility levels greater than or equal to 5%. In contrast, if past coverage among children aged less than or equal to 2 years were assumed to exceed 90%, increasing vaccination coverage with one dose of measles vaccine, without the addition of a second dose, would save costs compared with no change. In either situation, improving coverage with the first dose should be undertaken before adopting a two-dose vaccination schedule. Also presented at the meeting were findings of an economic assessment that contrasted various global measles prevention strategies -- control, elimination, and eradication. For each country, preliminary estimates were made of measles disease burden, vaccine needs, required financial resources, relative importance of economic and epidemiologic assumptions, and opportunity costs of investing in measles control rather than other selected health interventions. For each country, an estimate of age-specific measles susceptibility based on reported vaccination coverage, vaccine efficacy, reported age-specific attack rates, and case-fatality ratios was constructed. Costs of vaccination included direct vaccine and program costs, administration costs, costs of adverse events, and costs to treat measles cases that are not prevented. A 3% discount rate was used to estimate future costs in 1997 United States dollars. Present costs for vaccines, programs, and treatment of measles cases were estimated at $480 million annually. Findings of the analysis indicate that 80% of measles control program costs and disease treatment costs are paid by high-income countries (as categorized by the World Bank). However, of every 100 persons added each year to the global population that is susceptible to measles, 74 reside in low-income countries. The World Bank categorizes the world's most populous nations, India and China, as low-income countries. Under the assumptions used in this preliminary analysis, eradication would be cost-effective. The additional costs for vaccine and vaccination programs required to achieve eradication were estimated to be $4.7 billion, of which only $0.7-$1.8 billion would be required for low income countries. Conclusions: Economic Implications of Measles Elimination
NEXT STEPS Several lessons have been learned from previous efforts to eradicate communicable diseases (5). To eradicate a disease, medical scientists must have a thorough understanding of its natural history. To achieve consensus concerning the appropriate approach to eradication and sustained political commitment of resources, proponents of eradication should consult widely before embarking on the effort. National and international surveillance should be implemented early in the disease eradication program, and surveillance information should be used to guide program strategy. Implementation of the eradication strategy should emphasize flexibility and adaptation to the social, political, and public health circumstances of each country. A specific target date for eradication should be set to focus global efforts and maintain commitment to the goal of eradication. In addition to these general considerations, factors to be considered in implementing measles eradication include the high short-term costs of the endeavor, the risk of failure (i.e., the probability of failure and the potential consequences of failure), and the need to strengthen comprehensive health services to achieve eradication. Among the factors that favor measles eradication are
Factors that do not favor eradication include
In discussions of next steps, speakers urged meeting participants to
The next steps for measles control and elimination activities include design of a global strategy, preparing an operational plan and budget, obtaining political support, developing a partner/donor coalition, and implementing the strategy. Each step requires action at national, regional, and global levels. In addition, a consensus must be developed concerning the timing of measles elimination in relation to polio eradication. Specifically, should measles elimination be undertaken simultaneously with efforts to eradicate polio? Or should the efforts be undertaken sequentially? Meeting participants suggested that measles elimination should not be undertaken at the national level before poliovirus transmission is interrupted. At the global level, in contrast, activities aimed at achieving measles eradication should begin before polio eradication is achieved. Polio eradication must remain the first priority. Meeting participants pointed out that the more rapidly measles elimination activities proceed at the national and regional levels, the more easily measles eradication will be accomplished. Conversely, the more slowly elimination activities proceed, the more difficult eradication will be. Once measles transmission is interrupted in a population, risks for virus importation and reestablishment of transmission increase over time. Conducting repeated follow-up vaccination campaigns is operationally difficult and expensive. Because routine vaccination and follow-up campaigns rarely succeed in vaccinating all susceptible persons in a population, and because the vaccine is not 100% effective, the prevalence of measles susceptibility in the population tends to increase over time. Thus, the more protracted the global measles eradication campaign, the greater the risk for reestablishment of measles in countries where transmission of the virus has been interrupted. Participants also considered funding of measles eradication. Projects that attract donor support are successful (or have a high probability of success), are both politically and socially popular, provide visibility and recognition for donors, and have a specific goal and target date for completion. To attract support from potential partners and donors among governments, nongovernmental organizations, and the private sector, advocates of measles eradication should develop consensus concerning their objectives and strategies and communicate these objectives simply and directly. To succeed, advocates of eradication must reach consensus concerning the global disease burden of measles, likely cost savings from eradicating the disease, and resources required from external sources to accomplish the goal. The advocacy strategy should include identifying the key messages concerning measles eradication, forming coalitions of partners (including those in the private sector), and identifying advocates for fund-raising. Meeting participants considered consistency in messages about each aspect of measles eradication essential to the success of the advocacy strategy. Conclusions: Next Steps
References
Figure_1 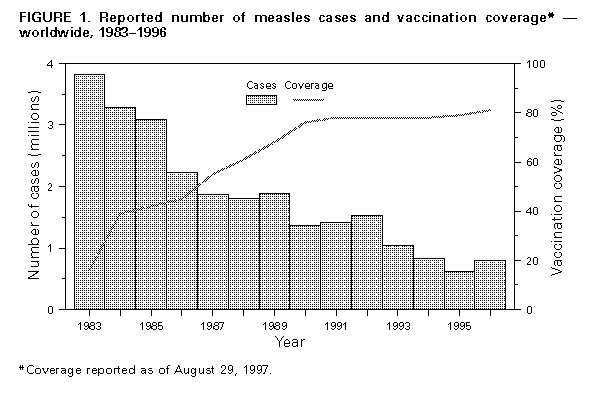 Return to top. Figure_2 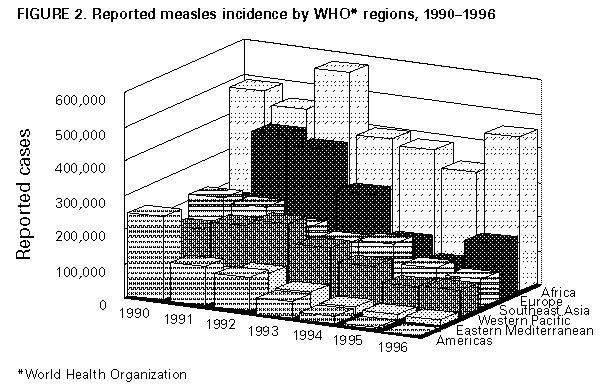 Return to top. Figure_3 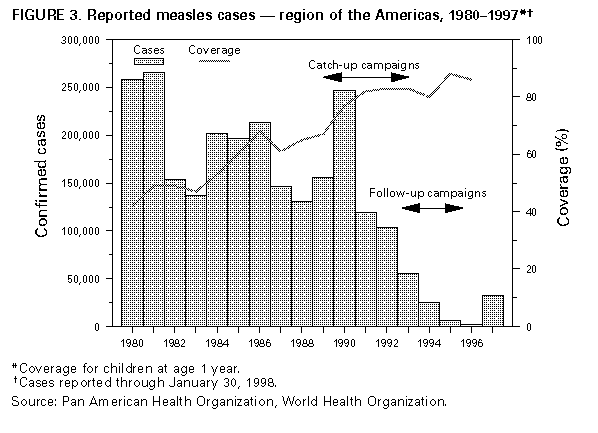 Return to top. Figure_4 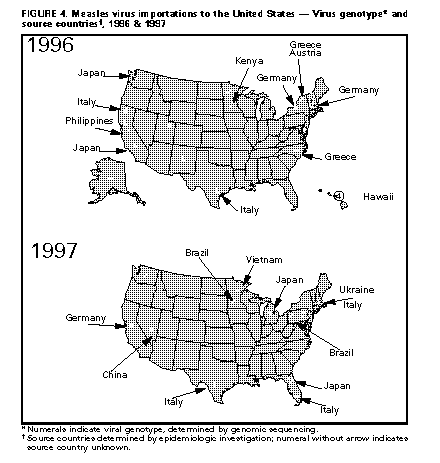 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 10/05/98 |
|||||||||
This page last reviewed 5/2/01
|