 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Foodborne Diseases Active Surveillance Network, 1996As an important strategy for addressing emerging infections in the United States, in 1994 CDC began implementing Emerging Infections Programs (EIPs) in state health departments, in collaboration with local health departments, academic institutions, and organizations of health professionals (1). EIPs are sites that conduct special population-based surveillance projects, emphasize collaborative epidemiologic and laboratory projects, and pilot and evaluate prevention efforts. The primary foodborne diseases component of the EIP is the Foodborne Diseases Active Surveillance Network (FoodNet) -- a collaborative effort among CDC, the U.S. Department of Agriculture (USDA), the Food and Drug Administration, and the EIP sites. The objectives of FoodNet are to 1) determine more precisely the burden of foodborne diseases in the United States, 2) determine the proportion of specific foodborne diseases associated with certain contaminated foods or with other exposures, and 3) provide the framework to respond rapidly and collaboratively to emerging foodborne diseases. This report summarizes preliminary results from FoodNet for 1996, which document regional and seasonal differences in the incidences of certain bacterial foodborne diseases, and presents findings of the 1995 baseline survey of clinical laboratories, which suggests that, for some pathogens, factors other than differing laboratory practices accounted for regional variations in incidences. Active Surveillance On January 1, 1996, FoodNet began collecting population-based active surveillance data on culture-confirmed cases of seven potentially foodborne diseases (Campylobacter, Escherichia coli O157:H7, Listeria, Salmonella, Shigella, Vibrio, and Yersinia infections) among the 13.2 million residents in five EIP sites *. After identifying the clinical laboratories that routinely tested for infectious agents the stool specimens of residents of the sites (including several out-of-state laboratories), these laboratories were routinely (i.e., weekly or monthly) contacted by investigators to identify cases. After removal of subsequent isolations from chronic carriers, annual incidence rates were calculated using the number of reported cases as the numerator and census estimates for the individual catchment areas as the denominator. In 1996, a total of 7223 culture-confirmed cases of the seven foodborne diseases were identified from stool specimens or specimens from normally sterile sites. Incidence rates were highest for campylobacteriosis (25 per 100,000 population), followed by salmonellosis (16), shigellosis (9), E. coli O157:H7 infection (3), Yersinia infection (1), listeriosis (0.5), and vibriosis (0.2). For all the diseases except salmonellosis, rates varied substantially among the EIP sites (Figure_1). Rates for campylobacteriosis ranged from 14 (Georgia) to 58 (California); for shigellosis, from 4 (Minnesota) to 20 (Georgia); for E. coli O157:H7 infection, from 0.6 (Georgia) to 5 (Minnesota); for Yersinia infection, from 0.5 (California) to 3 (Georgia); and for vibriosis, from 0.1 (Connecticut, Minnesota, and Oregon) to 0.3 (California). Rates also varied by age: for example, among children aged less than 1 year, the rate for salmonellosis ranged from 73 (Connecticut) to 270 (Georgia) and, for campylobacteriosis, ranged from 25 (Georgia) to 193 (California). Isolation patterns varied by season for several pathogens: 50% of E. coli O157:H7, 35% of Campylobacter, and 33% of Salmonella were isolated during summer months (June-August). The percentage of pathogens isolated from normally sterile sites (e.g., blood and cerebrospinal fluid) was 89% for Listeria, 10% for Vibrio, 9% for Salmonella, 3% for Yersinia, and 1% each for Shigella and Campylobacter. Of the 7223 case-patients, 1174 (16%) were hospitalized; hospitalization rates were highest for persons with listeriosis (94%), followed by those with Yersinia infection (32%), E. coli O157:H7 infection (28%), salmonellosis (22%), vibriosis (20%), shigellosis (14%), and campylobacteriosis (10%). Of the 34 deaths, 16 (47%) were associated with salmonellosis; nine (26%), with listeriosis; four (12%), with campylobacteriosis; two (6%), with E. coli O157:H7 infection; two (6%), with shigellosis; and one (3%), with vibriosis. Laboratory Survey To assess variations in laboratory culturing practices, in late 1995 FoodNet investigators mailed a questionnaire to the microbiology supervisor at each of the 234 clinical laboratories that tested stool specimens for infectious agents in the EIP sites. The 230 responding laboratories performed approximately 22,000 bacterial stool cultures in August 1995. Responding laboratories reported that all stool specimens submitted for bacterial culture were tested for Salmonella and Shigella, and approximately 99% of specimens were tested for Campylobacter. Culturing practices for Vibrio, Yersinia, and E. coli O157:H7 varied substantially among laboratories surveyed. Overall, 20% (range: 9%-43%) of stool specimens were tested routinely for Vibrio; 34% (range: 13%-52%), for Yersinia; and 47% (range: 6%-82%), for E. coli O157:H7. Overall, 80% (range: 58%-99%) of all bloody stool specimens submitted to these laboratories were tested for E. coli O157:H7. Reported by: S Shallow, MPH, P Daily, MPH, G Rothrock, MPH, California Emerging Infections Program; A Reingold, MD, Univ of California at Berkeley; D Vugia, MD, S Waterman, MD, State Epidemiologist, California State Dept of Health Svcs. T Fiorentino, MPH, R Marcus, MPH, R Ryder, MD, School of Medicine, Yale Univ, New Haven; P Mshar, JL Hadler, MD, State Epidemiologist, Connecticut State Dept of Public Health. M Farley, MD, M Bardsley, MPH, W Baughman, MSPH, Atlanta Metropolitan Active Surveillance Project; J Koehler, DVM, P Blake, MD, KE Toomey, MD, State Epidemiologist, Div of Public Health, Georgia Dept of Human Resources. J Hogan, MPH, V Deneen, MS, C Hedberg, PhD, MT Osterholm, PhD, State Epidemiologist, Minnesota Dept of Health. M Cassidy, J Townes, MD, B Shiferaw, MD, P Cieslak, MD, K Hedberg, MD, D Fleming, MD, State Epidemiologist, State Health Div, Oregon Dept of Human Resources. Food Safety Inspection Svc, US Dept of Agriculture. Center for Food Safety and Applied Nutrition, Food and Drug Administration. Foodborne and Diarrheal Diseases Br, Div of Bacterial and Mycotic Diseases, and Office of the Director, National Center for Infectious Diseases, CDC. Editorial NoteEditorial Note: The preliminary findings from FoodNet for 1996 document regional and seasonal differences in the incidences of certain bacterial foodborne diseases, particularly Campylobacter infection. Potential explanations for these differences include regional and seasonal variations in food-handling practices and the level of contamination of specific food items. Ongoing studies are directed toward determining whether the variations in laboratory culturing practices for E. coli O157:H7, Yersinia, and Vibrio are associated with the regional differences in incidences of the respective diseases. However, differences in laboratory practices did not account for variations in the incidences of Campylobacter and Shigella infections. FoodNet has enabled more precise calculation of incidences of seven bacterial foodborne pathogens and monitors the effectiveness of recent food-safety interventions (e.g., the USDA mandated changes in the meat and poultry inspection process in the United States). Additional studies of the seven diseases will assist in determining reasons for differing hospitalization rates and causes of death. FoodNet investigators also are conducting population-based surveys and surveys of physicians to determine what proportion of persons with diarrhea seeks medical care and what proportion of physicians requests specimens from persons with diarrhea. Analytic studies are being conducted to determine what proportion of E. coli O157:H7 and Salmonella serogroup B and D infections are associated with specific foods, foodhandling practices, and behaviors. In addition to addressing the burden and specific sources of foodborne diseases, FoodNet and EIP have provided the framework for responding to several emerging foodborne diseases in the United States. For example, FoodNet collaborators assisted in the investigations of several multistate outbreaks, including an outbreak of Cyclospora infections associated with consumption of raspberries imported from Guatemala (2) and an outbreak of E. coli O157:H7 infections associated with unpasteurized apple cider (3). On January 1, 1997, the addition of one county in Connecticut and 12 counties in Georgia increased the FoodNet surveillance population in the EIP sites to 14.7 million persons (6% of the U.S. population). In addition, collaborators from Maryland and New York joined EIP in 1997 and plan to conduct active surveillance in several counties in these states. On January 1, 1997, FoodNet initiated active surveillance for hemolytic uremic syndrome (HUS), a sequela of E. coli O157:H7 and other Shiga toxin-producing E. coli infections. At least three of the sites will conduct active surveillance for Cryptosporidia and Cyclospora, and all the sites plan to participate in a case-control study for Campylobacter infections in late 1997. References
* Minnesota, Oregon, and selected counties in California (Alameda and San Francisco), Connecticut (Hartford and New Haven), and Georgia (Clayton, Cobb, DeKalb, Douglas, Fulton, Gwinnett, Newton, and Rockdale). Figure_1 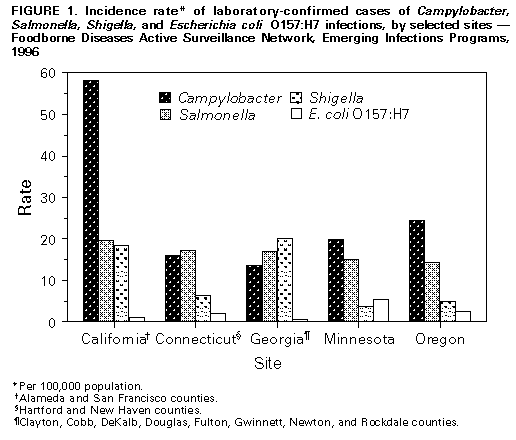 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|