 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Heat-Related Illnesses and Deaths -- United States, 1994-1995Although heat-related illness and death are readily preventable, exposure to extreme temperatures causes at least 240 deaths * during years with no heat wave. A heat wave is defined by the National Weather Service as greater than or equal to 3 consecutive days of temperatures greater than or equal to 90.0 F (greater than or equal to 32.2 C). In 1980, 1983, and 1988 (recent years with prolonged heat waves), 1700, 556, and 454 deaths, respectively, were attributed to heat. This report describes four instances of heat-related illness and death that occurred in the United States during 1994 and 1995 and summarizes risk factors for heat-related illness and death. Case 1. On June 13, 1994, in Houston, Texas, a 29-year-old mentally impaired women was found lying on the floor of her garage. She was unresponsive when admitted to a local hospital and had a rectal temperature of 107.9 F (41.9 C). She died within 2 days of arrival at the hospital. The outdoor temperature and humidity had reached 92.0 F (33.3 C) and 91%, respectively. Her underlying cause of death was listed as hyperthermia **. Case 2. On June 18, 1994, in St. Louis, Missouri, a 68-year-old woman who weighed approximately 350 pounds complained of "feeling ill" at 11 p.m. Her spouse phoned paramedics, who found her unresponsive; cardiac rhythm was undetectable after she was placed in the ambulance. At 11:38 p.m., she was pronounced dead on arrival at the emergency department with a rectal temperature of 108.9 F (42.7 C). Her home air conditioning system was operational but had not been used. The outdoor temperature and humidity that day had reached 95.0 F (35.6 C) and 45%, respectively. Her cause of death was listed as hyperthermia, with morbid obesity listed as an "other condition." Case 3. On July 1, 1994, in Tucson, Arizona, a 44-year-old woman, her 53-year-old brother (both mentally retarded), and their 72-year-old mother were found dead in their home by neighbors after they had not been seen for several days. The coroner's report indicated that the mother died first, and the children had remained in the house until they also died. There was no air conditioner in the house, and all windows were closed. The outdoor temperature and humidity had reached 106.0 F (41.1 C) and 36%, respectively. The cause of death for all three was listed as hyperthermia due to heat exposure. Case 4. On June 26, 1995, in College Park, Georgia, a grocery store customer found a 6-year-old boy, a 4-year-old girl, and a 2-year-old boy in a locked car with the windows closed in the store parking lot. After unsuccessfully attempting to attract the children's attention, the customer called 911. Police and paramedics were able to get the 6-year-old to unlock the car door. Paramedics reported the children were unresponsive, disoriented, flushed, and profusely sweating and had delayed reflexes. The children were placed in the shade under a tree and given juice and water for rehydration; they regained alertness and began talking within 30 minutes. The children had been in the car for approximately 10-20 minutes. The outdoor temperature and humidity were 84.0 F (28.9 C) and 60%, respectively, and the estimated temperature inside the car was greater than or equal to 110.0 F (greater than or equal to 43.3 C). Paramedics reported that the children had classic signs of the onset of heatstroke that would have been life-threatening within 5-10 minutes. Reported by: C Anders, JA Jachimczyk, Forensic Center, Harris County Medical Examiner, Houston, Texas. R Green, Medical Examiner's Office, St. Louis, Missouri. B Parks, Forensic Science Center, Tucson, Arizona. D Miller, Western Regional Climate Center, Reno, Nevada. LB Harper, College Park Police Dept, CT Dillard, ER Evans, College Park Fire Dept, College Park, Georgia. Health Studies Br and Surveillance and Programs Br, Div of Environmental Hazards and Health Effects, National Center for Environmental Health, CDC. Editorial NoteEditorial Note: Each year 148-1700 persons die in the United States because of excessive exposure to high temperatures. The highest age-adjusted death rates for heat-related illness have occurred in Alabama, Arkansas, Arizona, Georgia, Kansas, Mississippi, Missouri, Oklahoma, and South Carolina (from one to six per 1 million persons per year during 1979-1992). However, deaths listed with an underlying cause of hyperthermia represent only a portion of heat-related excess mortality because increased mortality from cardiovascular, cerebrovascular, and respiratory causes also occurs during heat waves (1-4). Heatstroke, the most serious heat-related illness, is a medical emergency characterized by a body temperature greater than or equal to 105.0 F (greater than or equal to 40.6 C) and may include symptoms such as disorientation, delirium, and coma. Onset of heatstroke can be rapid with progression to life-threatening illness within minutes. Heat exhaustion is a milder form of heat- related illness that can develop following exposure for several days to high ambient temperatures and inadequate or unbalanced replacement of fluids and electrolytes. Heat exhaustion is characterized by dizziness, weakness, and fatigue and may be sufficiently severe to require hospitalization. The cases described in this report underscore the increased risk for heat-related illness and death among the very young (particularly infants), the elderly (i.e., persons aged greater than or equal to 65 years) Figure_1, and persons with impaired mobility (5). In addition, persons with chronic illness (e.g., cardiovascular disease) are at increased risk. Persons in these groups may be unable to obtain adequate fluids or to remove themselves from hot environments (e.g., closed automobiles). In extremely hot environments, the body is unable to cool itself through sweating. The risk for heat-related illness and death also may be higher among persons who use certain drugs (1), including neuroleptics (e.g., haloperidol or chlorpromazine), which impair thermoregulatory function; medications with anticholinergic effects (e.g., medication for Parkinson disease), which inhibit perspiration; and major tranquilizers (e.g., phenothiazines, butyrophenones, and thiozanthenes). In addition, excessive alcohol consumption can cause dehydration and may be a predisposing factor in heat-related illness (5). Salt tablets are not recommended and are potentially dangerous (1). Persons whose fluid consumption is restricted for medical reasons or who use diuretic medications should not alter their fluid intake patterns without the advice of their physicians. The risk for illness and death also may be increased in persons who are unacclimatized to the heat and who work or exercise vigorously outdoors, fail to rest frequently, or do not drink sufficient quantities of fluids; acclimatization to warm environments may require gradual exposure to high temperatures for 10-14 days (6). The use of an artificially cooled environment (e.g., air-conditioning or evaporative cooling units), even for a few hours each day, will reduce the risk for heat-related illness (5). Fans can be a source of relief in areas with low humidity. However, because increased air movement (e.g., fans) has been associated with increased heat stress when the ambient temperature exceeds approximately 100 F (37.8 C) and because fans are not protective at temperatures greater than 90 F (greater than 32.2 C) with humidity greater than 35% (the exact temperature varies with the humidity), fans should not be used for preventing heat-related illness in areas of high humidity (5,7). Persons without home air conditioners should be assisted in taking advantage of such environments in private or in public places, such as shopping malls. Immersion in cool water (59.0 F- 61.0 F {15.0 C-16.1 C}) also can be used for maintaining acceptable body temperature. References
* During 1979-1992, a total of 5379 deaths in the United States were attributed to excessive heat, classified according to the International Classification of Diseases, Ninth Revision (ICD-9), as E900.0, "due to weather conditions"; E900.1, "of man-made origin"; or E900.9, "of unspecified origin." These data were obtained from CDC's Compressed Mortality File (CMF), which contains information from death certificates filed in the 50 states and the District of Columbia that have been prepared in accordance with external cause codes. CDC's Wide-ranging ONline Data for Epidemiologic Research computerized information system was used to access CMF data. ** Hyperthermia is the diagnostic term used for deaths resulting from core body temperature greater than or equal to 105 F (greater than or equal to 40.6 C). Figure_1 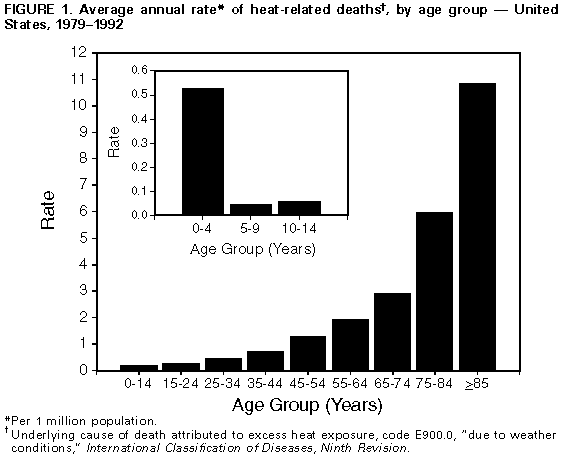 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|