 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Distribution of STD Clinic Patients Along a Stages-of-Behavioral-Change Continuum -- Selected Sites, 1993Human immunodeficiency virus (HIV) counseling and testing are important components of the public health effort to contain the acquired immunodeficiency syndrome (AIDS) epidemic. Project RESPECT is a multicenter randomized trial being conducted by CDC at five sexually transmitted disease (STD) clinics to evaluate the efficacy of HIV counseling interventions in preventing HIV and other STDs. Because consistent and proper use of latex condoms is one method to substantially reduce the risk for transmitting HIV and other STDs (1), the HIV prevention interventions being evaluated focus primarily on increasing consistent condom use with primary and other sex partners during vaginal and anal sex. Before initiating the randomized trial, pilot studies were conducted to better characterize the population and to develop an operationally feasible enhanced intervention. This report describes the results of one pilot study. During April and May 1993, patients who came to one of four STD clinics (Denver Metro Health Clinic, City of Long Beach {California} STD Clinic, Newark {New Jersey} STD Clinic, and San Francisco City Clinic) with a new symptom were offered $10 to participate in a pilot study interview. Of 1005 approached, 694 (69%) agreed to participate. Patients were asked about frequency of vaginal and anal sex with their primary and other sex partners, consistency of condom use during vaginal and anal sex, and both long-range ("sometime within the next six months") and short-range ("sometime within the next two weeks") intentions to always use condoms for vaginal and anal sex with their primary and other partners. Denominators vary because not all persons answered every question. Self-reported data were used to classify patients into one of five stages-of-change (SOC) categories: "precontemplation" (i.e., those who never or almost never used condoms and who reported no intention to always use condoms); "contemplation" (i.e., those who never or almost never used condoms but who intended to start always using condoms at some point in time, but usually not in the near future); "ready for action" (i.e., those who sometimes or almost always used condoms and who intended to start always using condoms in the near future); "action" (i.e., those who reported always using condoms but had been doing so for less than 6 months); and "maintenance" (i.e., those who reported always using condoms and had been doing so for 6 months or longer) (2). Two hundred sixty-eight (65%) men and 233 (82%) women reported having an opposite-sex partner they considered to be their primary sex partner (Table_1). Nearly all (97% {443/455}) reported having had vaginal sex with their primary partner during the past 30 days. Twenty-one percent (50/238) of men and 14% (26/193) of women reported always using condoms; 64% (124/193) of women and 55% (130/238) of men reported never using condoms for vaginal sex with their primary partner during this time (p=0.07). Two hundred (49%) men and 82 (29%) women reported having had sex with someone they did not consider to be a primary partner during the past 30 days. Nearly all (98% {273/279}) reported having had vaginal sex with other partners during the past 30 days. Nearly one third (31% {84/269}) of both men and women reported always using condoms; 40% (77/191) of men and 50% (39/78) of women reported never using condoms for vaginal sex with other partners during the past 30 days (p=0.29). Both men and women used condoms significantly more often with other partners than with primary partners (p=0.007). Distributions across the SOC categories for consistent condom use differed significantly by both sex and behavior (Figure_1). For vaginal sex with a primary partner, women were closer to adopting consistent condom use than were men (p less than 0.01). Men were closer to adopting consistent condom use for vaginal sex with other partners than with their primary partner (p less than 0.001). For vaginal sex with a primary partner, men and women were equally likely to be in the ready-for-action, action, and maintenance stages (p=0.74). However, men were more likely than women to be precontemplative than contemplative (p=0.02). Forty-three percent (97/225) of men with primary partners were precontemplative about always using condoms with their primary partners; 14% (15/106) of men with other partners were precontemplative about always using condoms with other partners (p less than 0.001). Reported by: M Fishbein, PhD, Univ of Illinois, Champaign. JM Douglas, Jr, MD, Denver Disease Control Svc. F Rhodes, Community Research and Service Program, Psychology Dept, California State Univ, Long Beach; LD Hananel, MSW, STD Control Program, Dept of Public Health, City and County of San Francisco. E Napolitano, STD Control Program, New Jersey Dept of Health. Epidemiology Research Br and Behavioral and Prevention Research Br, Program Operations Br, Div of Sexually Transmitted Diseases and HIV Prevention, National Center for Prevention Svcs, CDC. Editorial NoteEditorial Note: The findings in this report indicate that an SOC model can help identify differences in the adoption of consistent condom use that are often overlooked when only frequency of condom use is considered. For example, although men and women did not differ significantly in the frequency with which they used condoms with their primary partners, women were significantly more likely to consider adopting consistent condom use than were men. In addition, most STD clinic patients were in the precontemplative or contemplative stage with respect to consistent condom use -- i.e., although many patients attending the STD clinics never used condoms and had no intention of using them consistently, other patients who had never used condoms had formed long-range or short-range intentions to begin using condoms consistently. Therefore, even among patients who have never used condoms, counseling sessions must have different foci. Interventions that do not consider a person's location on an SOC continuum are likely to be ineffective (2). Changing behaviors is complex and requires knowledge of the factors underlying a specific behavior. Therefore, behavior-change interventions should address those underlying factors (e.g., attitudes, perceived norms, and self-efficacy) that can influence the likelihood that a person will move from one stage to the next. Previous studies suggest that among persons who are HIV seronegative, counseling and testing alone -- particularly in clinic settings -- has little or no effect on reducing high-risk behaviors (3,4). Because many of these studies do not clearly describe the counseling intervention, it is unclear whether they have evaluated the efficacy of risk-reduction counseling or whether they have evaluated only the efficacy of receiving a nonstandardized, relatively unstructured educational message. Behavioral science theory suggests that educational messages about a disease and how it is transmitted will have little impact on behavior change (5). The pilot study was conducted in STD clinics where participants had been evaluated and treated for an STD. Thus, these persons were at higher risk than the general population and were less likely to be correct and consistent condom users. Project RESPECT will evaluate the effectiveness of a theory-based counseling intervention by assessing 1) changes in underlying psychosocial variables (e.g., intentions, attitudes, perceived norms, self-efficacy), 2) movement along an SOC continuum, and 3) changes in incident STDs. Because most clinic patients are in the precontemplative or contemplative SOC, interventions targeted to these stages may produce measurable changes in condom-use intentions and behavior. References
TABLE 1. Percentage of men and women with a primary sex partner and other sex
partner(s), by sexual practice and condom use -- Project RESPECT pilot study, 1993
===========================================================================================
Sex partner status Men (n=410) Women (n=284)
--------------------------------------------------------------------------
Had a primary sex partner *
Had same partner >6 months 64% 68%
Had vaginal sex during preceding 30 days 97% 98%
Always used condoms + 21% 14%
Never used condoms + 55% 64%
Had anal sex during preceding 30 days 5% 4%
Total 65% 82%
Had other sex partner(s) *
Had vaginal sex during preceding 30 days 97% 100%
Always used condoms + 32% 29%
Never used condoms + 40% 50%
Had anal sex during preceding 30 days 2% 5%
Total 49% 29%
--------------------------------------------------------------------------
* 106 (26%) men and 49 (17%) women had both a primary and other sex partner(s) and are
included in both categories.
+ Condom use is a calculated rate of the number of times condoms were used divided by the
number of times participated in vaginal sex; always used condoms=100%; never used con-
doms=0.
===========================================================================================
Return to top. Figure_1 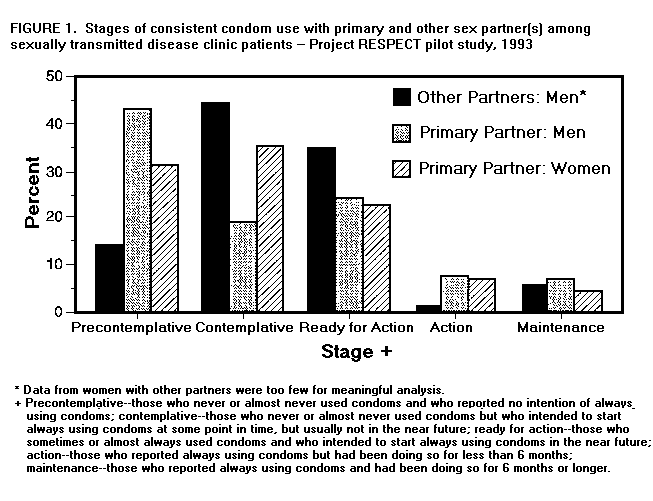 Return to top. Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 09/19/98 |
|||||||||
This page last reviewed 5/2/01
|