 |
|
|
|
|
|
|
| ||||||||||
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: mmwrq@cdc.gov. Type 508 Accommodation and the title of the report in the subject line of e-mail. Epidemiology of Measles --- United States, 2001--2003Measles is a highly infectious, acute viral illness that can cause severe pneumonia, diarrhea, encephalitis, and death. To characterize the epidemiology of measles in the United States during 2001--2003, CDC analyzed data reported by state and local health departments. This report summarizes the results of that analysis, which indicated that no endemic measles virus is circulating in the United States; however, imported measles cases continue to occur and can result in limited indigenous transmission. Maintaining immunity through high vaccination coverage levels is essential to limit the spread of measles from imported cases and prevent measles from becoming endemic. Following state laws and regulations, health-care providers, laboratories, and other health-care personnel report confirmed measles cases to state and public health departments; this information is forwarded to CDC. Data on variables such as vaccination status, age, complications, transmission setting, and serologic confirmation of cases also are collected. Measles cases are confirmed either by laboratory test or by meeting the clinical case definition (i.e., illness characterized by generalized maculopapular rash lasting >3 days, a temperature of >101º F [>38.3º C], and cough, coryza, or conjunctivitis) and being epidemiologically linked to a laboratory-confirmed case. Cases among persons who were infected outside the United States are classified as imported. Cases among persons who were infected in the United States are classified as indigenous. Indigenous cases are subclassified into three groups: import-linked (i.e., cases linked epidemiologically to an imported case); imported virus (i.e., cases that cannot be linked epidemiologically to an imported case, but for which imported virus has been isolated from the patient or from an epidemiologically linked patient); and unknown source (i.e., all other cases acquired in the United States for which no epidemiologic link or virologic evidence indicates importation). During 2001--2003, state and local health departments reported annual totals of 116, 44, and 56 confirmed measles cases, respectively (216 total cases). In 2002, a record low measles incidence of 0.15 cases per million population was reported, representing a 59% decrease from the incidence reported in 2000, which had been the lowest previously (1). During 2001--2003, of the total 216 measles cases reported, 96 (44%) were imported, and 120 were indigenous. Of the indigenous cases, 59 (49%) were import-linked, 18 (15%) were imported virus, and 43 (36%) were unknown source cases (Table). Import-associated cases (i.e., imported, import-linked, and imported virus cases) accounted for 80% of all reported cases (Figure). During 2001--2003, the highest percentage (47%) of imported measles cases was reported in 2001 (Figure). Imported cases occurred in 55 international visitors traveling to the United States and 41 U.S. residents exposed to measles while traveling abroad. The largest numbers of imported cases were from China and Japan. The 96 imported cases during 2001--2003 resulted in 42 chains of indigenous transmission. The greatest numbers of cases linked epidemiologically to an imported case were 10 in 2001, 12 in 2002, and nine in 2003. The longest durations of measles transmission following imported cases were 34 days in 2001, 27 days in 2002, and 62 days in 2003. Of the unknown source cases, 29 (67%) were isolated cases, eight (19%) were in chains of transmission involving two cases, and six (19%) were in two outbreaks (i.e., three or more linked cases). During 2001--2003, nine genotypes were identified among measles viruses detected in the United States. Measles virus was isolated from 27 chains of transmission, including 14 (16%) of 87 isolated cases, four (31%) of 13 two-case chains of transmission, and nine (56%) of 16 outbreaks. The most commonly identified genotypes were D7 and H1, which occurred in six and five chains of transmission, respectively. During 2001--2003, a total of 21 states reported no confirmed measles cases, and 23 reported one to nine cases. States reporting >10 cases (Alabama [12], California [50], Hawaii [27], New York [24], Pennsylvania [18], and Washington [16]) accounted for 69% of all cases. Fifteen states reported unknown source cases, and two states (California [14] and Hawaii [six]) reported more than five such cases. Of the 3,140 counties in the United States, 78 reported one or more confirmed cases; 14 counties reported four or more cases (range: four to 27 cases). Twenty-six counties reported unknown source cases, but no county reported more than six. Of 155 (72%) cases in U.S. residents, 116 (75%) occurred in vaccine-eligible persons (i.e., aged >12 months and born after 1957); 27 (23%) had received 1 dose of measles-containing vaccine (MCV), nine (8%) had received 2 doses of MCV, and 80 (69%) were either not vaccinated or had unknown vaccination status. Of 61 (28%) cases in non-U.S. residents, 42 (69%) occurred in vaccine-eligible persons; five (12%) had received 1 dose of MCV, one (2%) had received 2 doses of MCV, and 36 (86%) were either not vaccinated or had unknown vaccination status. In 2003, two measles-related deaths were reported. The first was attributed to measles encephalitis in a child aged 13 years who had chronic granulomatous disease, received a bone marrow transplant in October 2002, and died in January 2003. Measles was confirmed by a positive serologic test for measles IgM and isolation of measles virus from a brain biopsy. Despite an intensive search, no additional cases were detected in the surrounding area. The second measles-related death was in an international traveler aged 75 years infected in Israel who had measles pneumonitis and encephalopathy. Measles was confirmed by reverse transciptase-polymerase chain reaction from nasopharyngeal swab and urine. During 2001--2003, a total of 16 measles outbreaks were reported: 10 in 2001 and three each in 2002 and 2003. In 2001, the largest number of cases occurred in a multistate outbreak involving 13 imported cases and one contact among internationally adopted children (2). In 2002, the largest outbreak was associated with a day care center in Alabama (3); 10 infants who shared the same day care room were exposed to measles from an infant who was infected in the Philippines and attended the day care center. In 2003, the largest outbreak occurred in Hawaii, accounting for 12 cases in persons ranging in age from 3 months to 21 years. This outbreak began simultaneously with a measles outbreak in the Republic of the Marshall Islands (RMI) (4) and included three imported cases from RMI. Reported by: G Dayan, MD, M Papania, MD, S Redd, Epidemiology and Surveillance Div, National Immunization Program; P Rota, PhD, J Rota, MPH, S Liffick, L Lowe, MS, W Bellini, PhD, Div of Viral and Rickettsial Diseases, National Center for Infectious Diseases, CDC. Editorial Note:The findings in this report document a new record low number of cases since measles became a nationally reportable disease in the United States in 1912. The low reported incidence (i.e., less than one case per million) since 1997 and the high percentage of import-associated cases support the conclusion that measles is not endemic in the United States (5). Lack of endemic transmission also is demonstrated by the limited secondary transmission from imported cases. During 2001--2003, as in the previous 4 years, some measles cases of unknown sources were reported for which no link to importation was detected. However, these cases do not occur in temporal or geographic clustering patterns that might suggest a chain of endemic transmission. Moreover, the diversity of measles virus genotypes observed in the United States since 1997 (6) reflects multiple imported sources of virus and indicates that no genotype of measles is endemic in the United States. The outbreak in Alabama in 2002, with 10 of 10 exposed infants infected, demonstrates the high transmissibility of measles when the virus is introduced into susceptible populations; susceptibility to measles is high among U.S. infants. Approximately 95% of women giving birth after 2000 were born after measles vaccine licensure in 1963. Women born in the United States after 1963 transfer less measles antibody to their infants than women born before 1963. This results in increased susceptibility to measles among infants aged <12 months in the United States (7). However, the high level of measles immunity in the United States makes exposure to measles virus a rare event among infants. Infants traveling internationally should be vaccinated as early as age 6 months (8). Although measles is no longer endemic in the United States, imported cases continue to cause occasional limited transmission of measles. Even limited transmission can result in measles-associated deaths. The small number of import-linked cases after an importation demonstrates that population immunity to measles in the United States is sufficiently high to avoid sustained transmission of measles virus (9). The high levels of immunity result from high levels (i.e., >90%) of vaccine coverage with 1 dose of MCV among preschool children (10) and the required 2 doses of MCV for children attending school. Maintaining high levels of immunity through high vaccine coverage levels is essential to limit spread from imported cases and prevent measles from again becoming endemic in the United States. In addition, encouraging and assisting other countries to improve measles control can reduce the risk for importation. Acknowledgment The data in this report are based on contributions by state and local health departments. References
Table 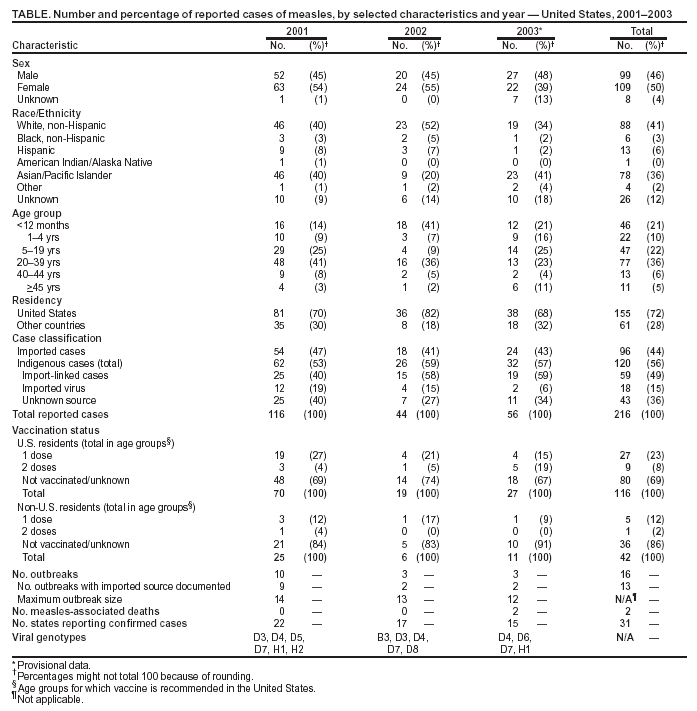 Return to top. Figure 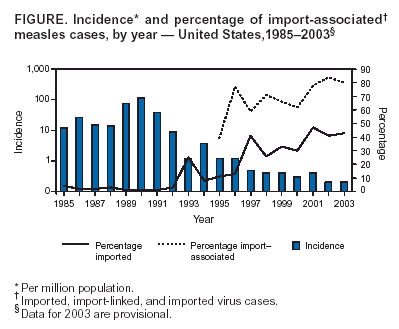 Return to top.
Disclaimer All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to mmwrq@cdc.gov.Page converted: 8/12/2004 |
|||||||||
This page last reviewed 8/12/2004
|